| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 3, March 2022, pages 115-118
A Huge Sister Mary Joseph’s Nodule From Signet Ring Cell Gastric Carcinoma Showing Good Response to FOLFOX-Based Chemotherapy Regimen
Ghizlane Raisa, d , Mouna Bourhafourb, Fatima Zahra Nafidia, Fadoua Raisc
aMedical Oncology Department, Faculty of Medicine and Pharmacy of Agadir, University Ibn Zohr , Agadir, CHU Souss Massa, Morocco
bMedical Oncology Department, Faculty of Medicine and Pharmacy of Casablanca, University Hassan II, CHU Ibn Rochd, Casablanca, Morocco
cRadiotherapy Department, University Hospital Center of Montreal, Montreal, QC, Canada
dCorresponding Author: Ghizlane Rais, Medical Oncology Department, Faculty of Medicine and Pharmacy of Agadir, University Ibn Zohr , Agadir, CHU Souss Massa, Morocco
Manuscript submitted January 5, 2022, accepted February 4, 2022, published online March 5, 2022
Short title: A Huge SMJN From Signet Ring Cell GC
doi: https://doi.org/10.14740/jmc3895
| Abstract | ▴Top |
Metastatic involvement of the umbilicus as a result of a visceral carcinoma is a rare entity known as Sister Mary Joseph’s nodule (SMJN). The most common primary sites are the gastrointestinal and gynecological tract. The occurrence of SMJN is commonly associated with advanced peritoneal disease and poor prognosis. The average survival time at the appearance of an umbilical metastasis is estimated at 10 months, and only 13% of patient will be alive at 2 years. Treatment usually involves systemic chemotherapy and palliative care, but the possibility of surgical resection should be considered especially if good response to systemic treatment is achieved in selected patients to maintain or to improve the quality of life. We describe here an unusual case of a 60-year-old man referred with enlarging umbilical lesion, identified as SMJN, that was metastasized from advanced signet ring cell carcinoma of the stomach with generalized peritoneal carcinomatosis. The nodule had rapid progression, and in a few days had reached 15 cm. Chemotherapy was started immediately and patient achieved good clinical and radiological response. A resection of the umbilical nodule was discussed but the patient unfortunately died following a massive pulmonary embolism. This case is unique in view of the unusual size of the SMJN in our patient and the good response to chemotherapy. We present this case to increase physician’s awareness for careful evaluation of the umbilical area and encourage them to look for a primary digestive tumor if an umbilical nodule is observed. Therapeutic response to primary chemotherapy may encourage a multimodal approach allowing resectability of the metastatic umbilical nodule.
Keywords: Umbilicus metastasis; Signet ring cell; Sister Marie Joseph nodule; Multimodal management
| Introduction | ▴Top |
Sister Mary Joseph’s nodule (SMJN) is an eponym to describe cutaneous metastasis of a visceral malignancy to the umbilicus. The umbilical metastasis is rare among skin metastases (5-9%) and usually may occur as part of systemic metastasis to viscera such as liver, lungs, bone, kidney [1, 2], etc. The lesion is often secondary to a deposit from gastric and colonic carcinoma (35-65%) but lesions from primary ovarian, pancreatic, and uterine tumors are reported. Furthermore, most of these metastases are pathologically diagnosed as adenocarcinoma [1]. Accurate diagnosis of SMJN is crucial because it mostly occurs in advanced and metastatic cancers, which signifies its poor prognosis. Moreover, survival time post umbilical metastasis was found to be variable but often short and ranging between 6 and 11months [3, 4]. Palliative management is usually the only option for most patients. However, in carefully selected cases, patients may benefit from more aggressive treatment such as surgery, chemotherapy, and radiotherapy [5].
In this report, a rare huge umbilical metastasis of an advanced gastric signet ring cell carcinoma exhibiting rapid growth is described. The therapeutic approach to our patient is presented and the pertinent literature is reviewed.
| Case Report | ▴Top |
Investigations
The patient is a 60-year-old man, with no significant past medical history. He complains of a 5-month history of abdominal pain and melena with rapidly progressive abdominal distention, weight loss of 6.61 lb and alteration of his general condition. Physical exam found an afebrile and eupneic patient with a stable hemodynamic status. Abdominal examination showed a distended abdomen with a huge soft, non-tender, and fixed umbilical mass, measuring up to 10 cm of largest dimension.
Diagnosis
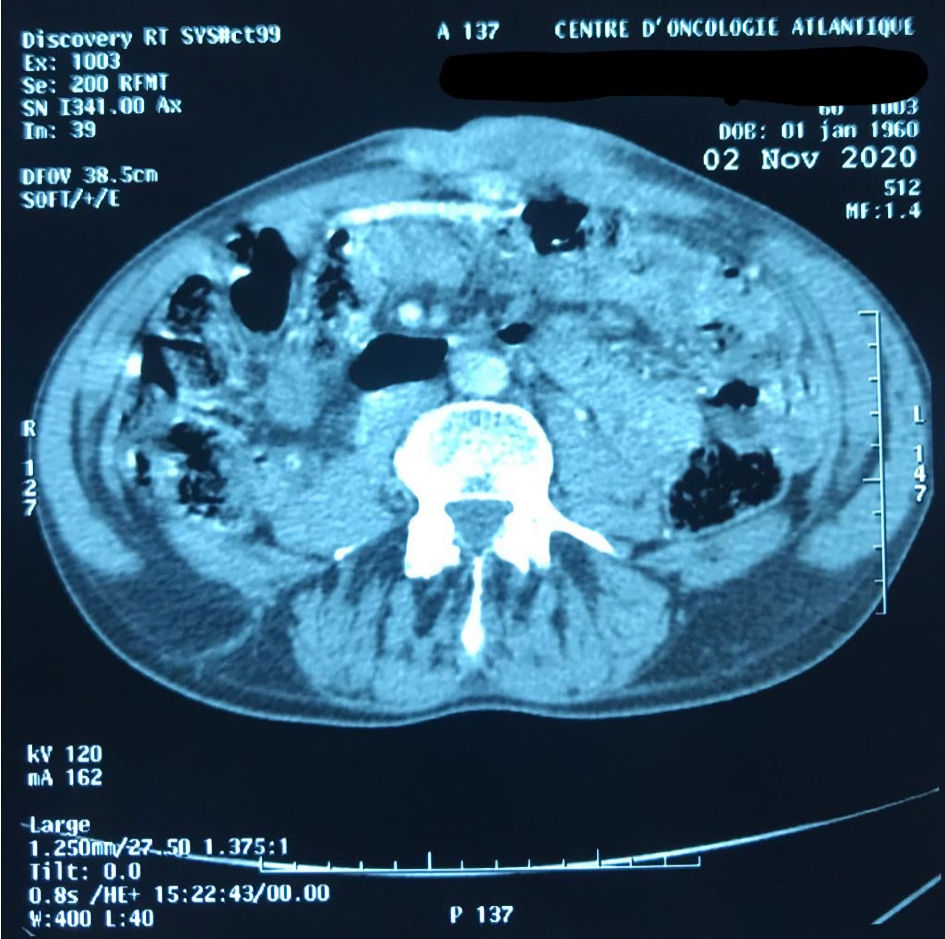
Abdominal computed tomography (CT) scan done before admission has shown a bulky circumferential gastric tumoral process, with diffuse local invasion and several peritoneal nodules along with low abundance ascites suggesting peritoneal carcinosis. The SMJN was also bulging into the umbilicus (Fig 1). A further thoracic CT scan demonstrated locoregional nodal extension to the celiac, mesenteric, and latero-aortic lymph nodal areas as well as bilateral pleural effusion.
 Click for large image | Figure 1. A contrast-enhanced CT scan before treatment showing an enlarged umbilical lesion with intraperitoneal nodule and ascites. CT: computed tomography. |
A gastric endoscopy was then performed and showed multiple bulky gastric tumoral nodules. Gross pathologic examination of the biopsied tissue showed a malignant carcinomatous proliferation. Microscopic examination demonstrated diffuse infiltration of the gastric wall by a proliferation of medium-size unattached, plasmacytoid cells with eccentric core and abundant eosinophilic cytoplasm, favoring a poorly differentiated signet ring cell carcinoma. A subsequent skin biopsy specimen taken from the nodule was suggestive of cutaneous metastasis from signet ring cell carcinoma.
Treatment
One week after admission, the nodule has reached 15 cm (Fig. 2), then a FOLFOX-based chemotherapy regimen was rapidly started (oxaliplatin 85 mg/m2, intravenous (IV) over 2 h on day 1 plus leucovorin 400 mg/m2, IV over 2 h on day 1 plus 5-FU 2,400 mg/m2 over 46 - 48 h continuous infusion; repeat every 2 weeks). He successfully completed the planned six cycles of chemotherapy in a well-respected timely manner.
 Click for large image | Figure 2. The huge Sister Mary Joseph’s nodule bulging into the left para-umbilical area. |
Follow-up and outcomes
Early in his medical visit assessment, the patient presented with a good clinical response, evidenced by a clinically important decrease of the umbilical nodule (Fig. 3). Also, the comparative imaging confirmed the shrinkage of the gastric wall invading mass, which went from 46 mm before chemotherapy to 26 mm after. A good response was also demonstrated in the distant metastatic sites of the peritoneal implants and umbilical mass which measured 22 × 53 mm (Fig. 4).
 Click for large image | Figure 3. Clinical response to chemotherapy with important shrinkage of the umbilical nodule. |
 Click for large image | Figure 4. CT scan demonstrating the good response to the FOLFOX-chemotherapy regimen. CT: computed tomography. |
A resection of the umbilical nodule was discussed but the patient unfortunately died suddenly following a massive pulmonary embolism 8 months after diagnosis.
| Discussion | ▴Top |
Gastric cancer (GC) is the third leading cause of cancer-related mortality among males and the fifth leading cause of cancer-related mortality among females worldwide, with 1 million of new cases diagnosed every year [6]. At the time of diagnosis, majority of patients have unresectable or metastatic disease. The most common sites of metastases are liver, lymph node areas and peritoneum, but in the advanced stages, there may be metastases to any region of the body [7].
Metastasis to the umbilicus from GC is a rare condition, and only few cases have been previously reported [7-15]. SMJN is the term commonly used to refer to cutaneous metastasis from internal malignancies. Dr. Hamilton Bailey was the first one who described this nodule as SMJN in his book entitled “Demonstrations of Physical Signs in Clinical Surgery” in 1949 to honor Sister Mary Joseph, who first suggested a link between patients having abdominal malignant neoplasms and umbilical nodule [1]. The primary malignant tumor associated with SMJN is considerably different in men and women. In men, the most common primary site is the stomach, followed by the colon and pancreas, whereas in women, SMJN originates more frequently from ovarian cancer followed by the endometrium, colorectal and pancreas [1, 4, 16].
Three hypotheses for the metastases in the umbilical region were suggested: direct spread of the tumor, vascular spread, and lymphatic dissemination [8]. In our case, the SMJN was most likely due to direct peritoneal spread since the patient presented with diffuse carcinomatosis, although proving this remains very difficult.
Metastasis to the umbilicus may be the only presenting symptom. However, solitary umbilical metastases are extremely rare, and most patients present in a poor clinical state with several physical signs such as ascites and pleural effusion [9-12].
Clinically, the SMJN usually presents as an irregular and firm nodule of variable size. Often, it presents as a small nodule measuring 1 - 1.5 cm in diameter. Occasionally it could be as large as 10 cm [10]. Sometimes, these nodules may be painful, ulcerated and may present with bloody, serous, or purulent discharge [10, 11]. This was the case in our patient who presented with a huge, tense, erythematous, painful, and rapidly progressive umbilical mass, which measured almost 15 cm of largest diameter. Imaging with CT and/or magnetic resonance imaging (MRI) scan helps to establish the extent of malignancy.
The differential diagnosis of SMJN includes malignant lesions as primary umbilical carcinoma and benign swellings such as pyogenic granuloma, epidermal cyst, hemangioma, abscess, umbilical hernia, and endometriosis (pseudo-SMJN) [11].
Histopathologic assessment is usually carried out to confirm the diagnosis and the origin of metastasis as there is many possible differential diagnoses [5, 9-10]. In most cases, histopathological examination reveals an adenocarcinoma, followed by squamous cell carcinoma, undifferentiated malignant tumors, and signet ring cell carcinoma [12]. In fact, signet ring cell carcinoma accounts for approximately 10% of GCs and most authors have described a worse prognosis for this histological subtype as compared to other GCs [13]. Furthermore, signet ring carcinomas is found in 16-20% of skin metastases including umbilical site from stomach cancers, which is consistent with the highly metastatic potential of these tumors especially for cases with peritoneal invasion [14].
Treatment strategy for cancer associated with SMJN should be individualized for each patient and should consider the primary cancer (gastrointestinal, ovarian, or other), the extension of distant metastases and the resectability of the umbilical nodule [4, 5, 14]. Despite that the occurrence of umbilical metastases is usually considered an ominous sign of advanced peritoneal disease that are unresectable or not amenable to surgery, multimodal strategy aiming to improve surgical outcomes, survival or to maintain quality of life, especially in selected patients, should be considered. Some reports indicate that patients who are treated actively with both surgery and chemotherapy have a much better survival rate than those who are treated with either surgery alone or chemotherapy alone [5, 12-15].
Interestingly, our patient had a good response to FOLFOX-based chemotherapy and was scheduled to receive palliative resection of the umbilical nodule. Unfortunately, patient died before surgery from thromboembolic complication.
The prognosis of umbilical metastasis from gastric adenocarcinoma is very poor. A 2-year survival rate of only 13.5% regardless of the etiology of the primary cancer was reported. The prognosis is particularly worse when these metastases are present at the time of diagnosis, as in our case.
In general, survival rate of treated patients ranges between 5 and 11 months, starting at the time of diagnosis of the umbilical metastases [12, 14, 15].
Learning points
There are three main reasons to present this interesting case report. First, it sheds light on the importance of considering the possibility of umbilical metastases from gastrointestinal cancer whenever an umbilical nodule is discovered. The second one is the unusual large size of SMJN in our patient. Third, it had good response to chemotherapy suggesting a potential benefit from resectability of this nodule even for palliative purposes.
In conclusion, umbilical metastasis is uncommon and usually occurs late in the disease process, underscoring the importance of early detection. Careful examination of umbilical lesions is required to allow early diagnosis of internal malignancies. The purpose of presenting this case report is not only to report an uncommon case of SMJN but also to raise awareness among clinicians adding this clinical entity as a differential diagnosis when an umbilical nodule is discovered.
Acknowledgments
We would like to thank the Department of Radiology at the Regional Center of Oncology, Agadir Morocco, for their cooperation and help.
Financial Disclosure
This research received no external funding.
Informed Consent
Written informed consent was obtained from the patient’s next of kin for publication of this case report and any accompanying images.
Conflict of Interest
The authors declare no conflict of interest.
Author Contributions
GR and MB were involved in the analysis of the data, literature search and writing of the manuscript. FZN helped with the patient management and revision of the manuscript. FR contributed to the preparation of this manuscript, and interpretation of the case. All the authors have read and approved the final version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Pereira WA, Humaire CR, Silva CS, Fernandes LH. Sister Mary Joseph's nodule: a sign of internal malignancy. An Bras Dermatol. 2011;86(Suppl 1):4 S118-120.
doi pubmed - Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990;22(1):19-26.
doi - Zhang CJ, Sun GP, Liu H, Peng WR, Xiong FX, Pan YY, Da J. Primary clear cell adenocarcinoma of the peritoneum presents as Sister Mary Joseph's nodule: a case report and literature review. Eur J Gynaecol Oncol. 2014;35(6):745-748.
- Gabriele R, Conte M, Egidi F, Borghese M. Umbilical metastases: current viewpoint. World J Surg Oncol. 2005;3(1):13.
doi pubmed - Yoshinori I, Takashi K. A long-term survival case of Sister Mary Joseph's nodule caused by colon cancer and treated with a multidisciplinary approach. Nagoya J Med Sci. 2019;81:325-329,.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
doi pubmed - Ekinci AS, Bal O, Ozatli T, Turker I, Esbah O, Demirci A, Budakoglu B, et al. Gastric carcinoma with bone marrow metastasis: a case series. J Gastric Cancer. 2014;14(1):54-57.
doi pubmed - Zhang Z, Wang J, Huang J, Yu X. Umbilical metastasis derived from early stage rectal cancer: a case report. World J Surg Oncol. 2014;12:82.
doi pubmed - Girijala RL, Riahi RR, Cohen PR. Sister Mary Joseph nodule as a cutaneous manifestation of metastatic appendiceal adenocarcinoma: case report and literature review. Cureus. 2018;10(2):e2244.
doi - Husein-ElAhmed H, Aneiros-Fernandez J, Arias-Santiago S, Naranjo-Sintes R. Sister Mary Joseph's nodule as a metastasis of ovarian adenocarcinoma. Int J Dermatol. 2010;49(9):1045-1046.
doi pubmed - Dubreuil A, Dompmartin A, Barjot P, Louvet S, Leroy D. Umbilical metastasis or Sister Mary Joseph's nodule. Int J Dermatol. 1998;37(1):7-13.
doi pubmed - Ioannidis O, Cheva A, Stavrakis T, Paraskevas G, Papadimitriou N, Kakoutis E, Makrantonakis A. Sister Mary Joseph's nodule as the sole presenting sign of gastric signet ring cell adenocarcinoma. Gastroenterol Clin Biol. 2010;34(10):565-568.
doi pubmed - Berlth F, Bollschweiler E, Drebber U, Hoelscher AH, Moenig S. Pathohistological classification systems in gastric cancer: diagnostic relevance and prognostic value. World J Gastroenterol. 2014;20(19):5679-5684.
doi pubmed - Zadeh VB, Kadyan R, Al-Abdulrazzaq A, Al-Otaibi S, Sarhan A, Najem N. Sister Mary Joseph's nodule: a case of umbilical cutaneous metastasis with signet ring cell histology. Indian J Dermatol Venereol Leprol. 2009;75(5):503-505.
doi pubmed - De Angeli M, Carosi M, Vizza E, Corrado G. Sister Mary Joseph's nodule in endometrial cancer: A case report and review of the literature. J Cancer Res Ther. 2019;15(6):1408-1410.
doi pubmed - Dhruv S, Anwar S, Polavarapu A, Kashi M, Andrawes S. Sister Mary Joseph's nodule: where umbilicus holds the truth! Cureus. 2021;13(2):e13091.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


