| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 6, June 2022, pages 269-273
Cachexia and Invisible Stomach on Endoscopy: An Endoscopist’s Enigma and a Surgeon’s Axiom
Kanthi Rekha Badipatlaa, b, Suresh K. Nayudua, b, Michelle Frances Dominguezb, g, Jeremey Wongc, Kevin Louied, Ali A. Chaudhrie, Robert Karpinosf, Karev Dmitryd
aDivision of Gastroenterology and Hepatology, SBH Health System, Affiliated With Albert Einstein College of Medicine, Bronx, NY 10457, USA
bDepartment of Medicine, SBH Health System, Affiliated with Albert Einstein College of Medicine, Bronx, NY 10457, USA
cSchool of Medicine, City University of New York, Townsend Harris Hall, NY 100316, USA
dDepartment of Surgery, SBH Health System, Affiliated With Albert Einstein College of Medicine, Bronx, NY 10457, USA
eDepartment of Pathology, SBH Health System, Affiliated With Albert Einstein College of Medicine, Bronx, NY 10457, USA
fDepartment of Anesthesia, SBH Health System, Affiliated With Albert Einstein College of Medicine, Bronx, NY 10457, USA
gCorresponding Author: Michelle Frances Dominguez, Department of Medicine, SBH Health System, Affiliated with Albert Einstein College of Medicine, Bronx NY 10457, USA
Manuscript submitted January 5, 2022, accepted May 9, 2022, published online June 11, 2022
Short title: GDI From a Giant Gastric Hyperplastic Polyp
doi: https://doi.org/10.14740/jmc3899
| Abstract | ▴Top |
Gastroduodenal intussusception (GDI) is a very rare clinical entity in adults. GDI can present acutely or chronically in adults with varying spectrum of symptoms and signs. GDI can present acutely with abdominal pain, vomiting and palpable mass. In rare instances it can lead to anemia and cachexia. Computed tomography (CT) of the abdomen can demonstrate GDI in majority of cases. However, endoscopy findings could lead to identifying etiological factor and tissue diagnosis. In majority of the cases endoscopy may show mucosal or submucosal lesion leading to GDI. We bring forward a case of GDI wherein patient presented with cachexia, intermittent vomiting along with anemia. Further workup including imaging has resulted in the rare diagnosis of GDI. Interestingly we encountered a rare of its kind, endoscopic presentation where there was total absence of stomach due to its complete invagination through the pylorus into the duodenum arising from a giant gastric hyperplastic polyp. We have successfully managed this patient with surgical intervention leading to positive clinical outcomes. On review of literature, we found that it is extremely rare to have a completely absent stomach on endoscopy in a patient with no previous surgical intervention. We would like to share our experience so that endoscopists are aware of such uncommon and interesting presentations. To the best of our knowledge, such a case has not been reported so far in literature.
Keywords: Intussusception; Gastroduodenal; Absent stomach; Hyperplastic polyp
| Introduction | ▴Top |
Adult intussusception is an unusual condition in clinical practice and gastroduodenal involvement remains an even more uncommon presentation [1, 2]. While there are many different etiologies for gastroduodenal intussusception (GDI), gastrointestinal stromal tumor (GIST) has been reported in literature as the most common cause of GDI [2]. We present a case of 39-year-old female who underwent esophagogastroduodenoscopy (EGD) for chronic upper gastrointestinal symptoms along with weight loss and anemia. EGD findings included non-visualization of the stomach. Diagnosis of complete GDI was confirmed by computed tomography (CT) scan. Further diagnostic laparoscopy and laparotomy aided in successful management of the giant hyperplastic gastric polyp resulting in GDI. To the best of our knowledge, we are not aware of such an unusual case.
| Case Report | ▴Top |
Investigations
A 39-year-old female presented to our hospital emergency department for acute psychotic episode manifested as bizarre behavior. She was known to be suffering from schizoaffective disorder, epilepsy and bronchial asthma. While she was being managed for her acute psychiatric crisis, she was found to be cachectic. On eliciting further history, it was noted that she has been experiencing episodes of intermittent vomiting associated with anorexia and significant weight loss. She denied history of abdominal pain, gastrointestinal bleeding and other gastrointestinal symptoms. She denied cardiorespiratory and neurological complaints. There was no reported history of fever and urinary complaints. Although she had prior remote history of menorrhagia, her last menstrual cycle was more than 6 months prior to her hospital admission. She reported having a cesarean section in the past. She denied use of tobacco, alcohol or recreational drugs.
On initial assessment, her vital signs were within normal limits. She was noted to have temperature of 36.9 °C, pulse was 85 beats per minute, respiration was 16 breaths per minute and blood pressure was 121/67 mm Hg. Her height was 168 cm, and weight was 48 kg. Body mass index (BMI) was 17. On examination she was thin built and cachectic with loss of muscle mass. Cachexia syndrome was considered given the combination of weight loss, fatigue, anorexia by history, low BMI and muscle wasting on examination and anemia on laboratory tests. Her chart review suggested that she had a prior visit in our hospital system 3 years before current admission and comparative assessments revealed a weight loss of about 51 kg. While she previously weighed 99 kg, this hospitalization weight was recorded to be 48 kg. This is about 50% loss of baseline weight in 3 years and was considerably significant. Gastrointestinal examination revealed a firm palpable mass in the upper abdomen which was non-tender and partly mobile. On auscultation, bowel sounds were noted to be normoactive. Rectal examination had normal tone, no masses and with no evidence of overt gastrointestinal bleeding. Cardiorespiratory and neurological examination were within normal limits. Laboratory studies revealed microcytic anemia with a hemoglobin level of 4.8 g/dL and hematocrit of 18.9%. She received blood transfusion for further stabilization. She was admitted to general medical floor and a gastroenterology consultation was requested.
Diagnosis
Patient underwent EGD under monitored anesthesia care. The esophagus appeared normal. With further advancement of the scope, it appeared that the scope went directly into the small bowel with non-visualization of the stomach. Retroflexion in the small bowel showed the gastroesophageal junction with reduced volume of gastric cardia being seen (Fig. 1). Possibility of a mass lesion at the cardia was considered and mucosal biopsies were done. A colonoscopy was attempted but could not be done due to poor bowel preparation.
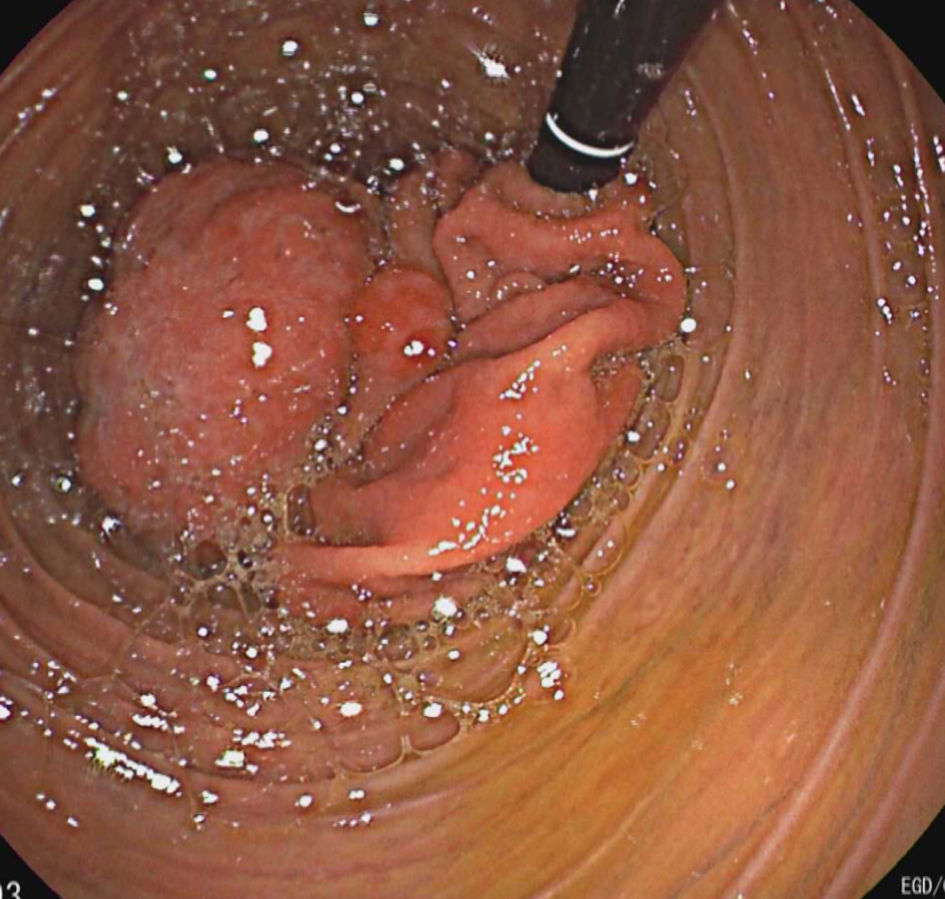 Click for large image | Figure 1. Endoscopy showing duodenum with remnant of stomach on retroflexion. |
A follow-up CT scan of the abdomen with oral and intravenous contrast showed a large mass measuring 23.7 cm in length 12 cm in width and 7.5 cm in antero-posterior dimension extending from the left upper quadrant to the right lower quadrant resulting from invagination of the stomach into either the duodenum or the distal stomach, consistent with GDI or gastro-gastric intussusception (Figs. 2, 3). A secondary dilatation of the distal esophagus was noted. Esophagus was fluid filled and measuring 5.8 cm in width. Severe compression of pancreas and hepatic flexure of the colon was noted on the CT scan.
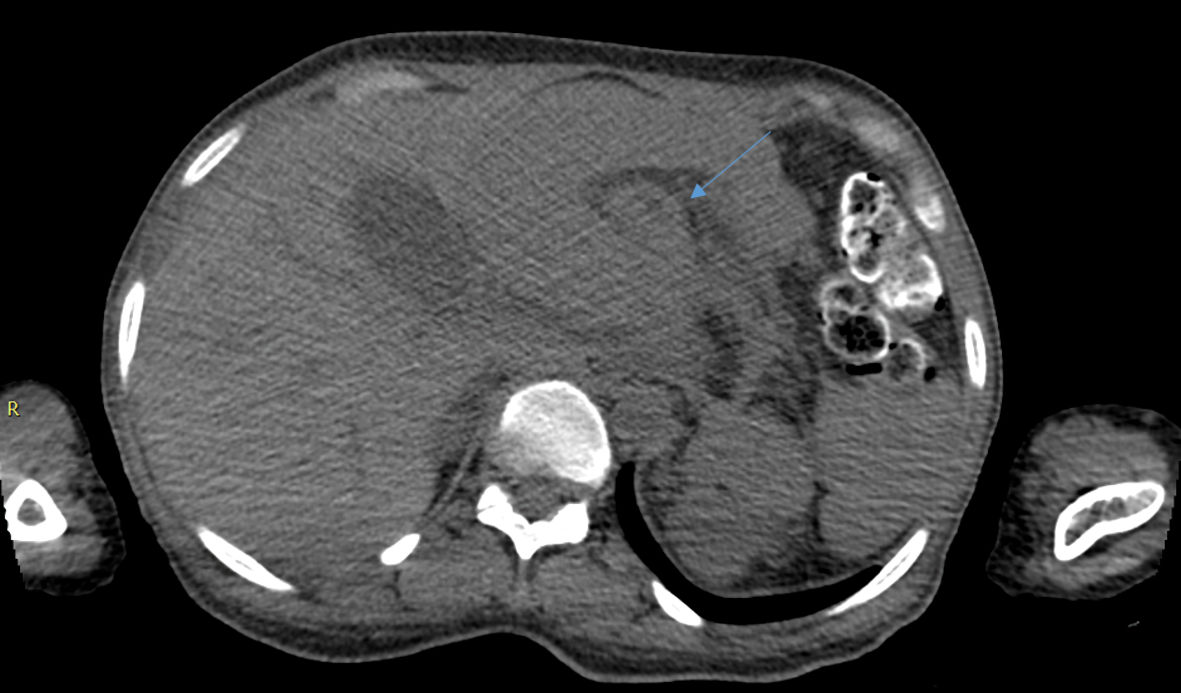 Click for large image | Figure 2. Axial view CT image of the top of intussusception (blue arrow pointing to fat between intussusceptum and intussuscipiens). CT: computed tomography. |
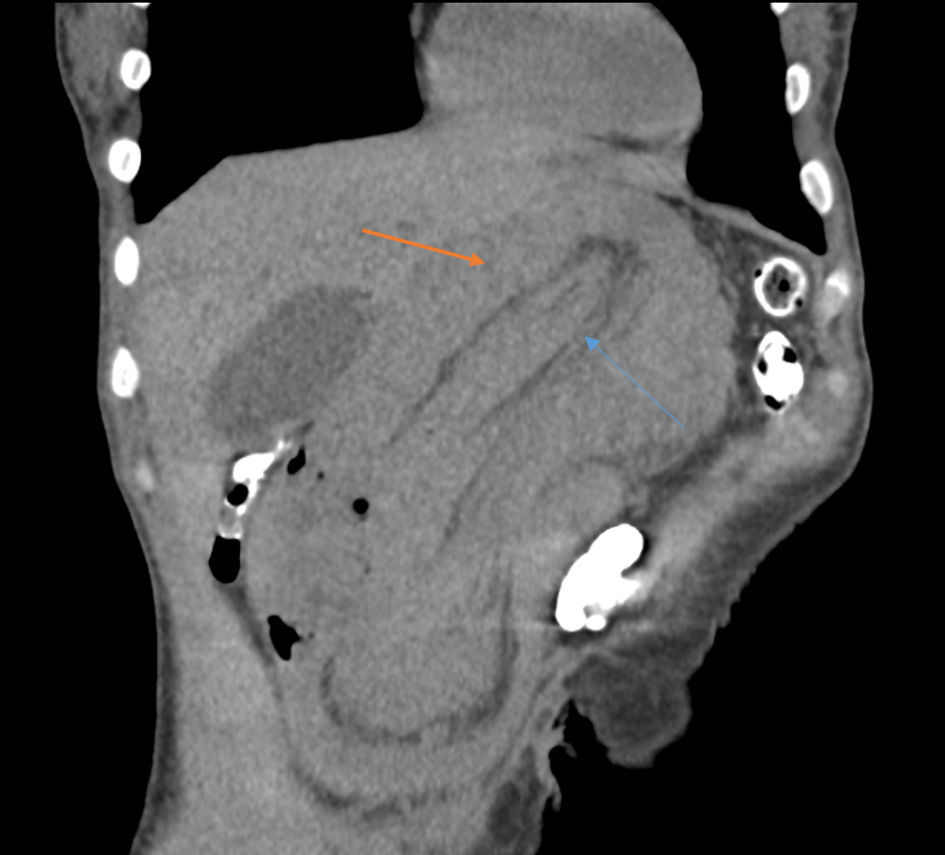 Click for large image | Figure 3. Coronal view CT of abdomen image (blue arrow is intussusceptum; orange arrow is intussuscipiens). CT: computed tomography. |
A preoperative tumor marker profile was obtained which revealed a normal level of alpha fetoprotein, carcinoembryonic antigen (CEA) and cancer antigen (CA) 19-9 levels. CA 125 level was elevated to 89.7 U/mL. An appropriate consultation with gynecology service was obtained. She did not have any gynecological complaints and it was concluded that the elevations could be explained by the gastric lesion.
Treatment
Attempts were made to address the cachexia state. A consultation was obtained from the nutrition department, and she was initiated on protein, iron, vitamin C and thiamine supplementation as recommended. She was also given supplements to promote wound healing with a combination of amino acids, collagen, and micronutrients. With the understanding that the syndrome was largely related to the structural abnormality involving the stomach, a prompt surgical correction with the background of adequate nutritional support seemed to be the most appropriate management. Surgical evaluation was completed, and patient underwent diagnostic laparoscopy under general anesthesia, which subsequently was converted to exploratory laparotomy to facilitate further reduction of this giant intussusception and therapeutic intervention. Frozen section sampling at the time of surgery revealed epithelial tissue with no invasion. Intraoperative findings were significant for a complete gastro-duodenal intussusception, and a giant polypoid lesion originating from endoluminal aspect of gastric wall being the lead point (Fig. 4). GDI was reduced, and wedge gastrectomy was performed.
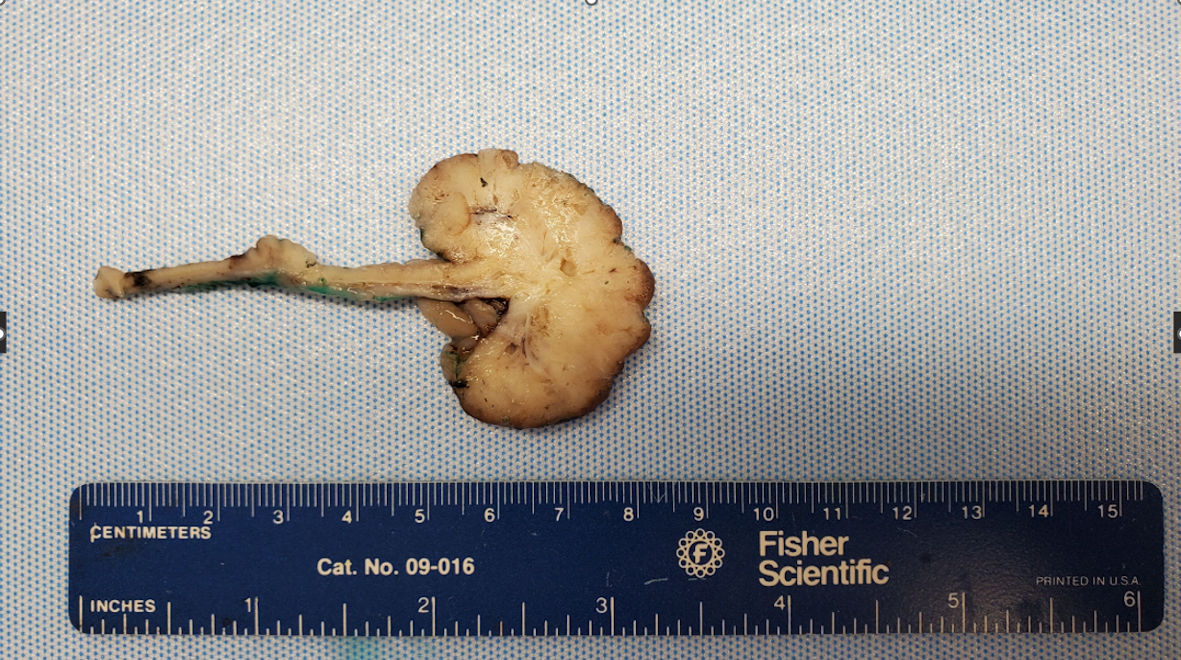 Click for large image | Figure 4. Gross surgical specimen showing pedunculated gastric polyp. |
Endoscopic mucosal biopsies were negative for any neoplastic growth on pathology. Gross surgical pathology specimen was noted to be an exophytic mass. However, pathology from surgical specimen revealed a hyperplastic gastric polyp with surface granulation tissue. Mild foveolar atypia limited to scatted gland crypts was seen, as evaluated with strong uniform nuclear staining with Ki-67 immunostaining (Fig. 5), and background gastric tissue has reactive gastropathy. The lesion was negative for Helicobacter pylori organisms on hematoxylin and eosin (H&E)-stained sections. There was no intestinal metaplasia as evaluated with Alcian blue/PAS special stain and it was negative for dysplasia in multiple step sections.
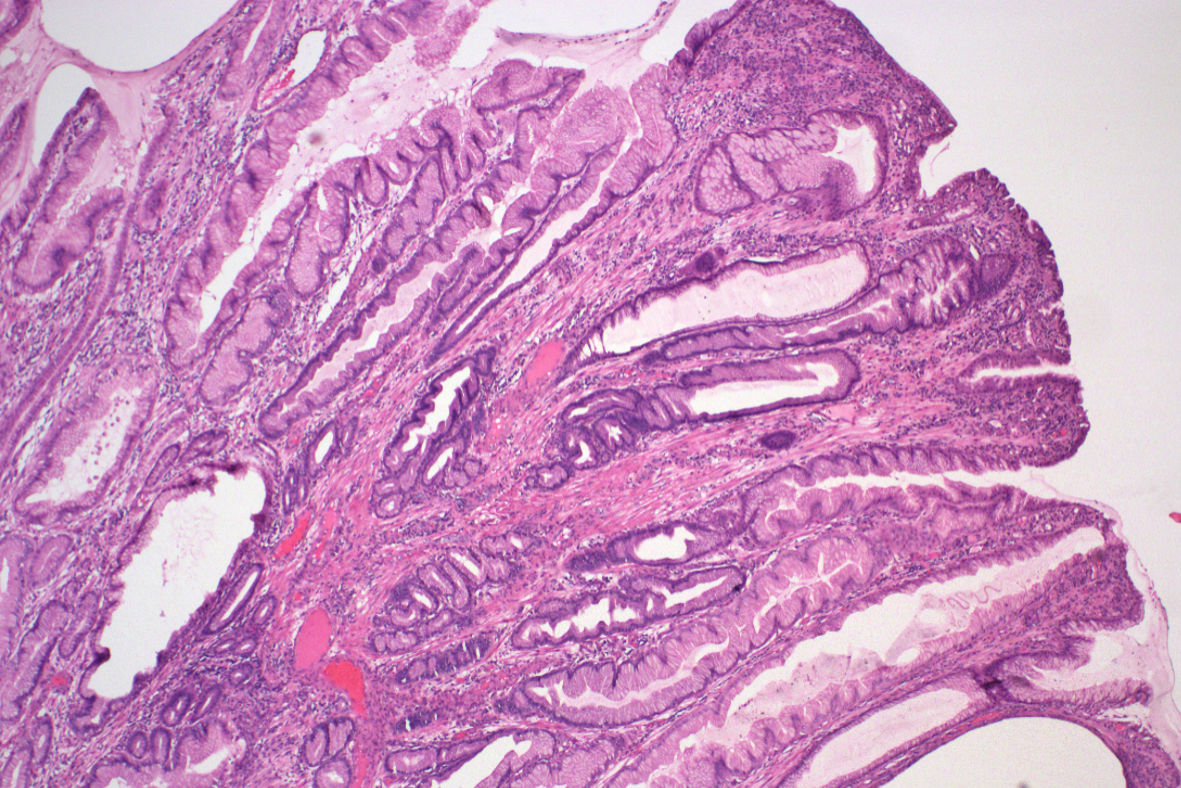 Click for large image | Figure 5. Medium-power image showing gastric hyperplastic polyp on H&E staining. H&E: hematoxylin and eosin. |
Follow-up and outcomes
Her postoperative course was uneventful. Her diet was advanced to regular diet which she tolerated well on the second postoperative day. Her pain was controlled, and she was discharged home in stable condition on the third postoperative day.
| Discussion | ▴Top |
GDI is an uncommon cause of gastric outlet obstruction. It results from a lead point of the stomach wall invaginating into the duodenum through the pylorus.
Most commonly intussusception of the gastrointestinal tract involves the large and small bowel. Gastric involvement is less common [1]. GDI accounts for 10% of the cases of adult intussusception [2].
Clinical presentation varies from acute to subacute or chronic presentations. Symptomatology includes abdominal pain, vomiting, changes in appetite and gastrointestinal bleeding [3].
Gastrointestinal examination could reveal a possible mass [4]. Clinical variability could be related to the size and reducibility of the lesion with smaller and reducible lesions presenting with mild and intermittent symptoms [5]. There are variable sized lesions reported in literature, but this large of a size extending diametrically to the opposite abdominal quadrant is very rare. This has caused secondary compression of the colon and the pancreas which was appreciated radiologically. Interestingly, it was a benign hyperplastic polyp on pathology.
Sometimes diagnosis is not made until late given the insidious, intermittent, and nonspecific symptoms [4]. Lesions could largely increase in size by the time formal diagnosis is made as in our case.
Symptoms of gastric outlet obstruction are known to be present in cases of GDI [3]. Rare cases of biliary obstruction and pancreatitis have also been described in literature and are usually a result of obstruction at the level of the ampulla of Vater [6]. Our patient did have severe compression of the pancreas owing to the giant size of the lesion, although she did not have clinical pancreatitis. Secondary gastrointestinal hemorrhage can complicate the clinical picture. CT is helpful in revealing the definitive diagnosis [7].
Both benign and malignant tumors can lead to intussusception [8]. Possible etiologies include gastric polyps, soft tissue lesions like lipoma and leiomyoma, gastro-intestinal stromal tumors, and cancers [9]. Gastro-intestinal stromal tumors are the most commonly reported cause. A prior intervention or procedure could also be considered one of the risk factors to develop an upper gastrointestinal intussusception. There are rare, reported cases of GDI associated with placement of percutaneous endoscopic gastrojejunostomy tubes [10] and after a prior gastric bypass surgery [10]. It could also be an uncommon presentation of peptic ulcer disease [11]. Peutz-Jegher syndrome is the most common gastrointestinal polyposis syndrome that leads to this condition [12].
Endoscopic diagnosis of GDI is possible, and gastroenterologists should be aware of the same [13]. But our case was a complete surprise where complete invagination occurred to an extent that there was no stomach visible.
Successful endoscopic reduction of GDI has been described in literature [14]. Definitive endoscopic resection of the etiological lesion with techniques like submucosal dissection is possible [15] and can be considered when feasible. Management however remains mainly surgical with attempts to restore anatomy as well as possible resection of the causal lesion [16]. Based on the size of the lesion a laparoscopic resection can be attempted [17] although, giant lesions like in our patient typically will need conversion to open laparotomy.
Conclusions
We present this extremely uncommon case of gastrointestinal intussusception arising from a giant hyperplastic polyp. We believe that the intermittent nature of the symptomatology has allowed the patient to delay medical attention while the lesion has progressed to such a humongous size while still being benign on pathology.
We would like to share our experience so that endoscopists can consider GDI as one of the possible differentials when they encounter altered anatomy while performing endoscopic procedures, especially in a patient where there is no prior history of upper gastrointestinal surgery. This case is an enigma wherein a giant gastric hyperplastic polyp caused the entire stomach to telescope through the pyloric opening, where the therapeutic answers were provided by surgical interventions. We are not aware of such an atypical presentation in literature so far. A high index of suspicion coupled with prior knowledge of literature about such atypical endoscopic presentations will help guide gastroenterologists to arrive at a provisional diagnosis and work towards appropriate clinical management.
Learning points
The objective to report this case is to increase knowledge base about this rare condition of GDI. While providing a pertinent background discussion on the general etiological causes and symptomatology we also want to bring forward this case of complete GDI resulting from a giant gastric hyperplastic polyp. We want to highlight the fact that the resulting symptoms could have significant impact on patient’s health with resulting cachexia. Diagnosis is mostly by radiology, with endoscopy also providing additional details. Surgical interventions are the preferred modality of treatment, GDI should be a diagnosis of consideration for endoscopists encountering abnormal anatomy while performing upper gastrointestinal endoscopies.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors report no conflict of interest related to this manuscript.
Informed Consent
Informed patient consent was obtained to write and publish this case report.
Author Contributions
Kanthi Rekha Badipatla, MD, Michelle Frances Dominguez, MD and Jeremey Wong, MD wrote and edited the case report. Kanthi Rekha Badipatla, MD, Suresh K. Nayudu, MD wrote and edited the abstract, introduction and discussion. Kevin Louie, DO, Robert Karpinos, MD, Karev Dmitry, MD reviewed the manuscript. Choudhury A., MD, provided review of pathology.
Data Availability
The authors declare that data supporting the findings of the study are available within the article.
| References | ▴Top |
- Jetha Z, Lisi M. Prolapsed fundic gastric polyp causing gastroduodenal intussusception and acute pancreatitis. J Surg Case Rep. 2018;2018(7):rjy139.
doi pubmed - Rittenhouse DW, Lim PW, Shirley LA, Chojnacki KA. Gastroduodenal intussusception of a gastrointestinal stromal tumor (GIST): case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2013;23(2):e70-73.
doi pubmed - Dokic M, Novak J, Petric M, Rankovic B, Stabuc M, Trotovsek B. Case report and literature review: patient with gastroduodenal intussusception due to the gastrointestinal stromal tumor of the lesser curvature of the gastric body. BMC Surg. 2019;19(1):158.
doi pubmed - Yalamarthi S, Smith RC. Adult intussusception: case reports and review of literature. Postgrad Med J. 2005;81(953):174-177.
doi pubmed - Kim DJ, Lee JH, Kim W. Gastroduodenal intussusception resulting from large hyperplastic polyp. J Gastric Cancer. 2012;12(3):201-204.
doi pubmed - Chahla E, Kim MA, Beal BT, Alkaade S, Garrett RW, Omran L, Ogawa MT, et al. Gastroduodenal intussusception, intermittent biliary obstruction and biochemical pancreatitis due to a gastric hyperplastic polyp. Case Rep Gastroenterol. 2014;8(3):371-376.
doi pubmed - Khanna M, Ramanathan S, Ahmed A, Kumar D. Gastroduodenal intussusception secondary to a pedunculated Brunner's gland hamartoma: CT and endoscopic features. J Gastrointest Cancer. 2014;45(Suppl 1):257-260.
doi pubmed - Kleinhaus U, Weich YL, Maoz S. Gastroduodenal intussusception secondary to prolapsing gastric tumors. Gastrointest Radiol. 1986;11(3):229-232.
doi pubmed - Numpraphrut P, Niltwat S, Parakonthun T, Pausawasdi N. Gastroduodenal intussusception of a gastrointestinal stromal tumor: a rare cause of acute pancreatitis. Clin Endosc. 2022;55(3):447-451.
doi pubmed - Zhang KS, Bansal J, Bansal A, Chitnavis V. Adult intestinal intussusception caused by the gastrojejunostomy tube: an endoscopically treatable phenomenon. Case Rep Gastrointest Med. 2021;2021:4325443.
doi pubmed - March B, Whiting S, Karihaloo C. Gastroduodenal intussusception of remnant stomach after gastric bypass: a case report. Obes Surg. 2019;29(12):4057-4059.
doi pubmed - Hung TH, Huang JW. Severe duodenal ulcer behaves like gastroduodenal intussusception. Ann R Coll Surg Engl. 2022;104(1):e14-e16.
- Mokhtari A, De Leucio A, Boitsios G. Gastroduodenal Intussusception in Peutz-Jeghers Syndrome. J Belg Soc Radiol. 2022;106(1):4.
doi pubmed - Lin JT. Endoscopic diagnosis of gastroduodenal intussusception. Endoscopy. 1996;28(3):324.
doi pubmed - Park YM, Kim JW, Jang JY. Gastroduodenal Intussusception and Endoscopic Reduction. Clin Gastroenterol Hepatol. 2019;17(11):e133.
doi pubmed - Hsieh YL, Hsu WH, Lee CC, Wu CC, Wu DC, Wu JY. Gastroduodenal intussusception caused by gastric gastrointestinal stromal tumor: A case report and review of the literature. World J Clin Cases. 2021;9(4):838-846.
doi pubmed - Siow SL, Wong CM, Febra S, Goh RET. Laparoscopic transgastric resection of gastroduodenal intussusception due to gastric leiomyoma. Med J Malaysia. 2020;75(5):609-611.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


