| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 10, October 2022, pages 517-520
Retroperitoneal Liposarcoma: The Giant Type
Subhi Mansoura, Nassim Azzama, Yoram Klugera, b, Safi Khuria, b, c
aDepartment of General Surgery, Rambam Medical Care Center, Haifa, Israel
bHepatoPancreatoBiliary and Surgical Oncology Unit, Rambam Medical Care Center, Haifa, Israel
cCorresponding Author: Safi Khuri, HepatoPancreatoBiliary and Surgical Oncology Unit, General Surgery Department, Rambam Medical Care Center, Haa’leya Hashniya, Haifa 31096, Israel
Manuscript submitted September 23, 2022, accepted October 21, 2022, published online October 31, 2022
Short title: Giant Retroperitoneal Liposarcoma
doi: https://doi.org/10.14740/jmc4014
| Abstract | ▴Top |
Retroperitoneal tumors (RPTs) are very rare tumors that arise in the large space of the retroperitoneum. About two-third of these tumors are malignant, of which soft tissue sarcoma (STS) is the most common and comprises almost one-third of malignant RPTs. Twenty to thirty percent of RPTs are benign. The retroperitoneal cavity has a very large potential space for tumor enlargement to a very high diameters without causing specific symptoms, especially during the initial phase of tumor enlargement. On diagnosis, the average tumor weight is 15 - 20 kg and tumor diameter is 20 - 25 cm. The most common retroperitoneal sarcoma type is liposarcoma, which account for 20% of all sarcoma types and 40% of all retroperitoneal sarcomas (RPSs). Other less common STS arise in the retroperitoneum include leiomyosarcoma and undifferentiated pleomorphic type. Giant liposarcoma is usually defined either as tumor diameter of 30 cm or more or tumor weight of 20 kg or higher. This specific type of sarcoma is very uncommon, with few case reports published in the English literature. Herein, we present a case of a healthy 33-year-old male patient, who was admitted due to abdominal distension and increased body weight since few months. An abdominopelvic computed tomography (CT) scan demonstrated a giant retroperitoneal mass of almost 40 cm in diameter in its largest dimension, located in the right retroperitoneal space. Ultrasound (US)-guided fine needle biopsy (FNB) was consistent with well differentiated liposarcoma. Surgical resection of the tumor along with the right colon, right ureter and kidney, third and fourth duodenal parts and part of the right iliopsoas muscle was contemplated. Histopathological report revealed well-differentiated liposarcoma of 50 cm in diameter, with foci of dedifferentiation, presented by pleomorphic sarcoma. Surgical margins were microscopically negative.
Keywords: Retroperitoneal tumors; Rare tumor; Soft tissue sarcoma; Giant retroperitoneal sarcoma
| Introduction | ▴Top |
Retroperitoneal tumors (RPTs) are uncommon heterogeneous group of tumors that arise in the retroperitoneal cavity [1]. Primary RPTs usually develop from cells of the soft tissues (fat, muscles, bones, etc.), lymphatic system, or blood vessels. Tumors that originate from retroperitoneal organs, such as the pancreas, kidneys, adrenal glands or intra-pelvic retroperitoneal organs are not categorized as primary RPTs [2]. Seventy to eighty percent of primary RPTs are malignant, while 20-30% are benign tumors. Soft tissue sarcoma (STS) is known as the most common primary RPT. Although any subtype of STS tumors can develop in the retroperitoneal space, retroperitoneal liposarcoma (RPL), leiomyosarcoma and pleomorphic (undifferentiated) types are the most common [3]. Liposarcoma, which comprises almost 20% of malignant mesenchymal tumors in adults and 40% of retroperitoneal sarcomas, is the most common STS in the aforementioned age group [4]. Four types of liposarcoma are recognized according to the World Health Organization: well differentiated and dedifferentiated types, which are more common in the retroperitoneal cavity, and pleomorphic and myxoid types, which commonly originate in the extremities [5]. The retroperitoneal cavity has the potential for large space, which allows primary RPL to grow to an extremely large size. Due to the previously mentioned reason, primary RPL is usually asymptomatic during the initial phase of the disease, causing symptoms mainly when growing to large size due to pressure effect on nearby structures (duodenum, ureters, kidneys, pancreas, vessels or intrapelvic retroperitoneal organs) and to a lesser extent by organ invasion. The average diameter for primary RPL on diagnosis is 20 - 25 cm and average weight of 15 - 20 kg [6]. Giant RPL is defined as a tumor diameter of 30 cm or more, or tumor weight of 20 kg or more [7]. A very few cases (less than 25) of giant RPL are reported in the English literature as case reports or case series. Herein, we present a case of giant RPL that was treated at our medical center.
| Case Report | ▴Top |
Investigations
A young male patient, 33 years old, without a past medical history presented to our emergency department complaining of abdominal distension and non-intended weight gain for 3 months’ duration. In addition, he also suffered recent early satiety following solid and liquid meals. The patient denied nausea, vomiting or change in bowel habits. His past medical and surgical history were non-relevant.
Diagnosis
Upon his admission, his vital signs were within normal limits: blood pressure (BP): 128/78 mm Hg, pulse: 67 beats/min, respiratory rate: 11/min and temperature of 37 °C. By abdominal exam, the abdomen was distended, soft and lax without tenderness. A palpable huge mass that extends from the right upper quadrat to the right lower quadrant was noticed. Per rectum exam was normal. No evidence of inguinal hernias or leg edema was observed. His laboratory tests, including complete blood count (CBC), liver and kidney function test (LFTs/KFTs) were without exception. An abdomen-pelvic computed tomography (CT) scan with intravenous and oral contrast revealed a huge right retroperitoneal mass with a diameter of almost 40 cm (Fig. 1). The mass consists of low- and high-density areas. It extends from the right hypochondriac region down to the right iliac and hypogastric regions and into the pelvic cavity, causing dislocation of the retroperitoneal and intra-peritoneal organs due to mass effect. The stomach, pancreatic head, and superior mesenteric vein (SMV) are displaced proximally, while the right colon and terminal ileum displaced medially. The patient was admitted with a diagnosis of primary RPT for further investigation. For clinical staging, a chest CT scan was done, which excluded any findings of intra-thoracic metastasis. As a routine part of the workup at our institution, tumor markers including cancer antigen 19-9 (CA19-9) and carcinoembryonic antigen (CEA) were within normal levels. Due to the huge nature of the present tumor, it was decided to treat the patient by a multidisciplinary team (MDT), which included specialized surgeons in the field of RPTs, radiologists, gastroenterologists, and specialized oncologists. The patient was presented at our tumor board meeting. Although a high suspicion for retroperitoneal sarcoma was the main diagnosis, it was decided to complete the investigation by an ultrasound (US)-guided fine needle biopsy (FNB) to diagnose specifically the tumor subtype. Biopsy guided by an US revealed well differentiated liposarcoma.
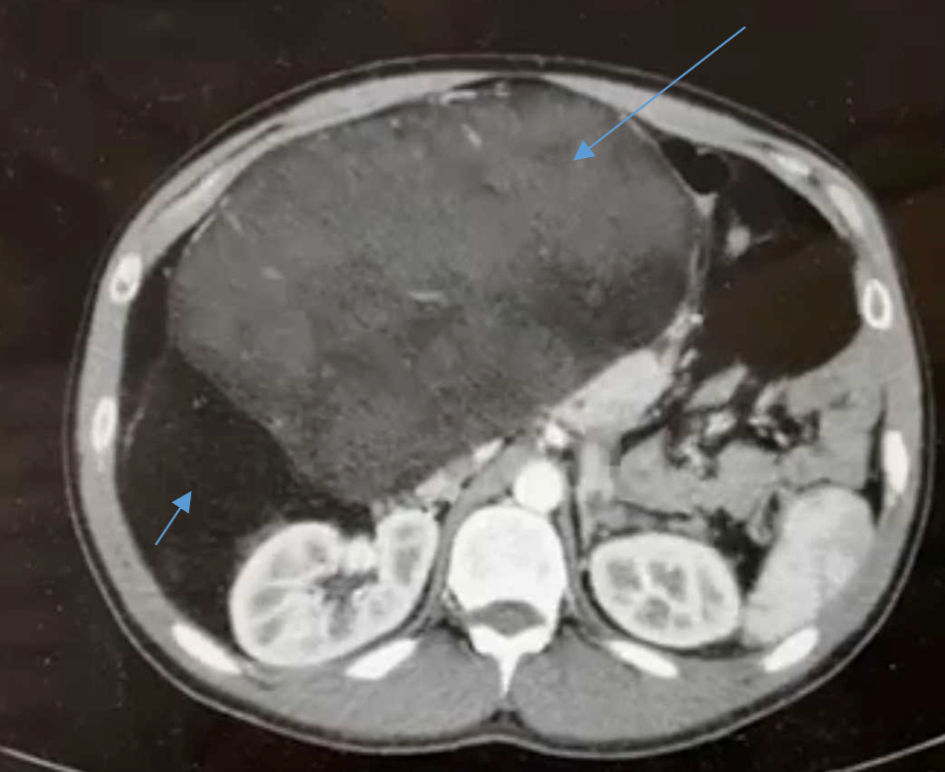 Click for large image | Figure 1. An axial abdominopelvic CT scan demonstrates a huge retroperitoneal mass with area of high (long arrow) and low (short arrow) of density, and the mass displacing the abdominal organs to the left side. CT: computed tomography. |
Treatment
Following the diagnosis of giant RPL, the patient was presented again at the tumor board meeting. Due to the ability for complete surgical resection of the tumor (according to imaging tests), it was decided to treat the patient by means of surgical resection of the tumor along with any suspicious involved organ. Since there was a high risk for resection of the right kidney (due to proximity for the primary tumor), and as a preparation for operation, the patient underwent dimercaptosuccinic acid scan (DMSA scan) which showed bilateral normal kidney function. Following, the patient underwent an exploratory laparotomy with the following findings: a huge right retroperitoneal mass composed mainly of fatty tissue, displacing the gastrointestinal tract to the left abdominal cavity. The tumor involves the right colon, terminal ileum, right kidney, and ureter and third and fourth duodenal parts (Fig. 2). Resection of the primary tumor along with the previously mentioned structures, along with part of the right ilio-psoas muscle were contemplated, with gastrointestinal reconstruction by anastomosing the second duodenal part and proximal jejunum and distal ileum to the transverse colon. The postoperative period was uneventful, and the patient was discharged home on postoperative day 13. The histopathological report demonstrated well differentiated liposarcoma tumor of 50 cm in diameter, with foci of dedifferentiation, presented by pleomorphic sarcoma. The tumor invades to perirenal fat and mesocolon without organ invasion. Microscopic surgical margins were free of tumor cells. The findings of the histopathological report were contemplated with grade 1 (G1, total score of 3) according to the French staging system for sarcoma tumors (FNCLCC).
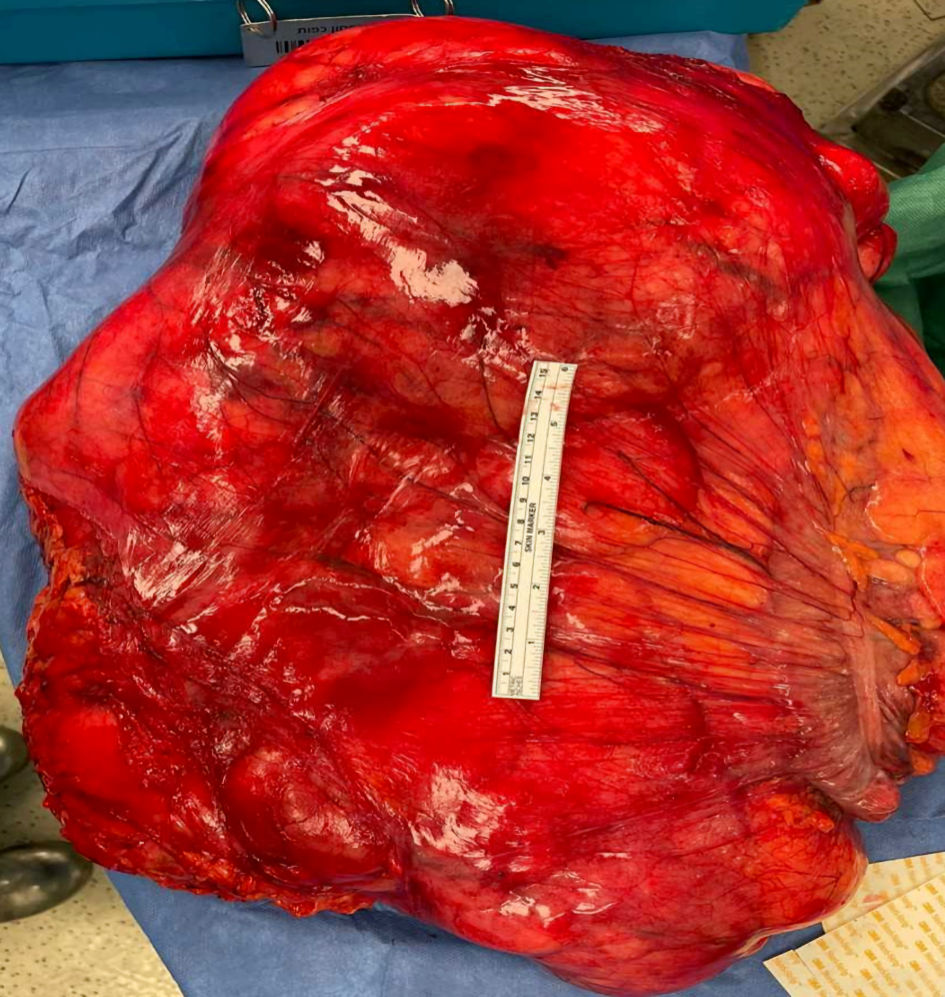 Click for large image | Figure 2. The specimen following resection of the primary RPL (50 cm diameter) which includes the tumor itself along with the right colon, terminal ileum, right kidney and ureter and third and fourth duodenal parts. RPL: retroperitoneal liposarcoma. |
Follow-up and outcomes
The patient’s case was discussed again at the tumor board with the question whether he should be treated by adjuvant radiation therapy. The decision was, due to negative surgical margin, the patient should be followed by clinical and radiological exams. Up to date, the patient has been followed by our outpatient clinic for 15 months. Initially, patient was followed once every 2 weeks up to 6 weeks following surgery, followed by once every 2 months and once every 6 months. During his follow-up, patient is doing well without specific symptoms. Abdominopelvic CT scans on 2 months, 6 months and 12 months following discharge were normal without evidence of disease recurrence.
| Discussion | ▴Top |
Giant primary RPL are extremely rare tumors. Reviewing the current English literature reveals only 24 reported cases of such tumor, 14 case reports [8-21] and case series including 10 cases of giant retroperitoneal dedifferentiated liposarcoma [22]. Herein, we describe the 25th case.
Most of the reported cases occur in male patients, with average age of diagnosis of 57 years old. Our patient was also male and younger than the reported average age (33 years old). The most common clinical presentation is abdominal distension (increased abdominal girth), as in our case.
The largest and smallest tumor diameter were 65 cm and 30 cm, respectively [19, 15]. The average size for all cases was 43.5 cm. Tumor diameter for our patient was in the range (50 cm). Abdominopelvic CT scan was the diagnostic imaging test of choice for all cases including ours. In contrary to most of the published cases, where diagnosis of RPL was made postoperatively, we have diagnosed giant RPL preoperatively by US-guided FNB. The main therapeutic management for such tumors is unknown, largely due to the rareness of this group of malignancies, in addition to the absence of scientific data based on prospective studies. Hence, an MDT approach has become crucial in confronting such surgical disease.
The most acceptable management for primary RPL is complete surgical resection with R0 (negative microscopic) margins, yet high rates of local recurrence are high at 66% [23, 24]. Five-year over survival following complete surgical resection is about 54%. Our patient was discussed several times at the tumor board meeting, in the presence of specialized physicians from different sectors, and the decision was to treat him by upfront surgical resection. Surgical resection without preoperative radiation therapy was the mainstay therapy for most of the reported cases as well. Only one patient received adjuvant radiotherapy.
The histopathological report was consistent with complete R0 surgical resection. Clinical and radiological follow-up for 15 months was negative for tumor recurrence.
In conclusion, giant RPL is an extremely rare tumor with very few cases reported in the English literature. Treatment is usually contemplated by an MDT of physicians. Authors are encouraged to report such rare cases to gain knowledge of the different characteristics, presentations, management, as well as follow-up of such rare entity.
Learning points
The main take away points from this case report is that giant RPLs are very rare tumors that usually become symptomatic at a late stage of the disease. An MDT approach is highly advocated to improve tumor recurrence and overall survival rate. Surgical resection with negative microscopic margins is the best therapeutic option.
Acknowledgments
None to declare.
Financial Disclosure
This is a self-financed manuscript without funding source.
Conflict of Interest
The authors do not have any conflict of interest.
Informed Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author Contributions
SM contributed to writing of the manuscript. The paper was drafted by NA. Critical revisions and final approval were made by YK and SK.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
RPTs: retroperitoneal tumors; STS: soft tissue sarcoma, RPL, retroperitoneal liposarcoma; CT: computed tomography; US: ultrasound; FNB: fine needle biopsy
| References | ▴Top |
- Osman S, Lehnert BE, Elojeimy S, Cruite I, Mannelli L, Bhargava P, Moshiri M. A comprehensive review of the retroperitoneal anatomy, neoplasms, and pattern of disease spread. Curr Probl Diagn Radiol. 2013;42(5):191-208.
doi pubmed - Scali EP, Chandler TM, Heffernan EJ, Coyle J, Harris AC, Chang SD. Primary retroperitoneal masses: what is the differential diagnosis? Abdom Imaging. 2015;40(6):1887-1903.
doi pubmed - Rosenberg AE. WHO Classification of Soft Tissue and Bone, fourth edition: summary and commentary. Curr Opin Oncol. 2013;25(5):571-573.
doi pubmed - Mack TM. Sarcomas and other malignancies of soft tissue, retroperitoneum, peritoneum, pleura, heart, mediastinum, and spleen. Cancer. 1995;75(1 Suppl):211-244.
doi - van de Rijn M, Fletcher JA. Genetics of soft tissue tumors. Annu Rev Pathol. 2006;1:435-466.
doi pubmed - Echenique-Elizondo M, Amodarain-Arratibel JA. Liposarcoma retroperitoneal gigante. Cir Esp. 2005;77:293-295.
doi - Makni A, Triki A, Fetirich F, Ksantini R, Chebbi F, Jouini M, Kacem M, et al. Giant retroperitoneal liposarcoma. Report of 5 cases. Ann Ital Chir. 2012;83(2):161-166.
- Yol S, Tavli S, Tavli L, Belviranli M, Yosunkaya A. Retroperitoneal and scrotal giant liposarcoma: report of a case. Surg Today. 1998;28(3):339-342.
doi pubmed - McCallum OJ, Burke JJ, 2nd, Childs AJ, Ferro A, Gallup DG. Retroperitoneal liposarcoma weighing over one hundred pounds with review of the literature. Gynecol Oncol. 2006;103(3):1152-1154.
doi pubmed - Clar H, Leithner A, Gruber G, Werkgartner G, Beham A, Windhager R. Interdisciplinary resection of a giant retroperitoneal liposarcoma of 25 kg. ANZ J Surg. 2009;79(12):957.
doi pubmed - Hashimoto Y, Hatakeyama S, Tachiwada T, Yoneyama T, Koie T, Kamimura N, Yanagisawa T, et al. Surgical treatment of a giant liposarcoma in a Japanese man. Adv Urol. 2010;2010:943073.
doi pubmed - Bansal VK, Misra MC, Sharma A, Chabbra A, Murmu LR. Giant retroperitoneal liposarcoma- renal salvage by autotransplantation. Indian J Surg. 2013;75(2):159-161.
doi pubmed - De Nardi P, Bissolati M, Cristallo M, Staudacher C. Recurrent giant liposarcoma of the spermatic cord. Urology. 2012;79(1):113-114.
doi pubmed - Sharma M, Mannan R, Bhasin TS, Manjari M, Punj R. Giant inflammatory variant of well differentiated liposarcoma: a case report of a rare entity. J Clin Diagn Res. 2013;7(8):1720-1721.
doi pubmed - Zhang WD, Liu DR, Que RS, Zhou CB, Zhan CN, Zhao JG, Chen LI. Management of retroperitoneal liposarcoma: A case report and review of the literature. Oncol Lett. 2015;10(1):405-409.
doi pubmed - Caizzone A, Saladino E, Fleres F, Paviglianiti C, Iaropoli F, Mazzeo C, Cucinotta E, et al. Giant retroperitoneal liposarcoma: Case report and review of the literature. Int J Surg Case Rep. 2015;9:23-26.
doi pubmed - Hazen B, Cocieru A. Giant Retroperitoneal Sarcoma. J Gastrointest Surg. 2017;21(3):602-603.
doi pubmed - Oh SD, Oh SJ, Suh BJ, Shin JY, Oh CK, Park JK, Kim YM, et al. A giant retroperitoneal liposarcoma encasing the entire left kidney and adherent to adjacent structures: a case report. Case Rep Oncol. 2016;9(2):368-372.
doi pubmed - Zeng X, Liu W, Wu X, Gao J, Zhang P, Shuai X, Tao K. Clinicopathological characteristics and experience in the treatment of giant retroperitoneal liposarcoma: A case report and review of the literature. Cancer Biol Ther. 2017;18(9):660-665.
doi pubmed - Herzberg J, Niehaus K, Holl-Ulrich K, Honarpisheh H, Guraya SY, Strate T. Giant retroperitoneal liposarcoma: A case report and literature review. J Taibah Univ Med Sci. 2019;14(5):466-471.
doi pubmed - Xu C, Ma Z, Zhang H, Yu J, Chen S. Giant retroperitoneal liposarcoma with a maximum diameter of 37 cm: a case report and review of literature. Ann Transl Med. 2020;8(19):1248.
doi pubmed - Bachmann R, Eckert F, Gelfert D, Strohaker J, Beltzer C, Ladurner R. Perioperative strategy and outcome in giant retroperitoneal dedifferentiated liposarcoma-results of a retrospective cohort study. World J Surg Oncol. 2020;18(1):296.
doi pubmed - Schwarzbach MH, Hohenberger P. Current concepts in the management of retroperitoneal soft tissue sarcoma. Recent Results Cancer Res. 2009;179:301-319.
doi pubmed - Raut CP, Pisters PW. Retroperitoneal sarcomas: Combined-modality treatment approaches. J Surg Oncol. 2006;94(1):81-87.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


