| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 3, March 2023, pages 81-87
A Rare Case of Coccidioidomycosis Meningitis
Henrik Ghantarchyana, c , Buzand Oganesiana, Monica M. Gayeda, Bahareh Maknounia, b, Mufadda Hasana, b
aDepartment of Internal Medicine, Arrowhead Regional Medical Center, Colton, CA 92324, USA
bDepartment of Pulmonary and Critical Care, Arrowhead Regional Medical Center, Colton, CA 92324, USA
cCorresponding Author: Henrik Ghantarchyan, Department of Internal Medicine, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted December 22, 2022, accepted January 11, 2023, published online March 31, 2023
Short title: Coccidioidomycosis Meningitis
doi: https://doi.org/10.14740/jmc4040
| Abstract | ▴Top |
Disseminated coccidioidomycosis is a fungal disease endemic to the Southwest United States as well as South and Central America. This dimorphic fungus typically manifests as pulmonary infection; however, there are very rare instances of extrapulmonary disseminated disease especially in immunocompromised hosts. Here, we present a 46-year-old immunocompromised patient with a recent diagnosis of pulmonary coccidioidomycosis that initially presented with acute respiratory failure and was found to have coccidioidomycosis meningitis. This case highlights that despite early and adequate treatment of a known pulmonary coccidioidomycosis infection, dissemination of the disease can still ensue and should be considered in cases of acute encephalopathy.
Keywords: Coccidioidomycosis; Fungal infection; HIV; Immunocompromised; Disseminated
| Introduction | ▴Top |
Coccidioidomycosis is known as valley fever due to its geographic prevalence of California, Arizona, Mexico, Central, and South America. It is mainly caused by Coccidioides immitis or C. posadasii fungus [1]. This rare disease is commonly acquired through inhalation of arthroconidia, which is found in dust or soil.
Once inhaled into the lungs, this fungus will then transform into endospore containing spherules [2]. It is believed that the affected region is the terminal and respiratory bronchioles, mainly due to the size of the inhaled spores, ranging from 3 to 5 µm [1]. In the immunocompetent host, a delayed-type hypersensitivity reaction (DTHR) helps control the infection. Due to the DTHR, symptoms in approximately 60% of the cases are absent [2].
If the fungus is not treated appropriately or is found in an immunocompromised host, coccidioidomycosis can spread to the lungs, brain, and meninges, leading to respiratory failure, sepsis, shock, or even death. One of the more life-threatening forms is when it spreads to the meninges, causing coccidioidomycosis meningitis (CM) [1]. It affects both immunocompetent and immunocompromised individual, but risk of dissemination is higher in immunocompromised host. We present a case of a 46-year-old human immunodeficiency virus (HIV)-positive male diagnosed with CM.
| Case Report | ▴Top |
Investigations
We present a case of a 46-year-old male with a recent diagnosis of coccidioidomycosis who presented to the emergency room for shortness of breath and cough of 2 months duration. This was associated with pleuritic chest pain, malaise, diffuse joint pain and intermittent fevers for 2 months. He denied any hemoptysis, recent travel, incarceration history or homelessness. Patient worked as a farmer in Bakersfield for the past 3 years. Two weeks prior to this hospitalization, the patient was seen at an outside facility for fatigue, fevers, and forearm lesions. He tested positive for Coccidioides antibody IgG.
On arrival, the patient was tachycardic at 133 beats per minute, tachypneic with a respiratory rate of 47, afebrile, normotensive and hypoxic with an oxygen saturation of 85% on room air. On initial examination, he had coarse bilateral breath sounds and labored breathing. There were 1- to 2-cm palpable subcutaneous nodules in the patients forearms bilaterally. He had no notable rashes, joint effusions, or neurologic deficits. The patient was cooperative, alert, oriented and able to answer questions appropriately with limitations due to shortness of breath.
The patient was transitioned to non-invasive mechanical ventilation due to increased work of breathing and was admitted to the intensive care unit (ICU) for acute hypoxemic respiratory failure and severe sepsis.
Diagnosis
A computer tomography (CT) scan of the chest with intravenous (IV) contrast on admission was notable for diffuse multifocal nodular consolidations and ground glass opacities. Patient also had right upper lobe dense consolidations and prominent mediastinal and hilar lymph nodes. He had clear central airways with no evidence of pulmonary embolism.
Treatment
During the first day, the patient was started on IV trimethoprim sulfamethoxazole 15 mg/kg daily, IV cefepime 2 g every 8 h, oral fluconazole 400 mg daily, IV liposomal amphotericin B 5 mg/kg daily, and oral prednisone 40 mg daily. The patient however decompensated overnight and required mechanical ventilation for airway protection. The night of admission, the patient decompensated further into septic shock requiring norepinephrine for blood pressure support.
Throughout his hospitalization, his blood cultures were negative. Tuberculosis (TB) was ruled out and fungal studies were negative for pneumocystis, cryptococcus, and toxoplasmosis, and were notable for coccidiomycosis with titer levels of 1:64 in the blood and 1:1 titer level in the cerebrospinal fluid, seen in Table 1. Infectious disease was consulted during this course. His antiretroviral therapy was held until cryptococcus and TB were ruled out. The patient’s hospital course was complicated by declining mentation, worsening respiratory status despite several different ventilator adjustments, minimal response to proning, and intermittent severe metabolic acidosis with renal failure which improved with dialysis and bicarbonate drips.
 Click to view | Table 1. Significant Laboratory Results From the Cerebrospinal Fluid |
Due to declining mentation, CT scan of the head with IV contrast (Fig. 1) was performed showing a corpus callosum mass extending into the left lateral ventricle with features consistent with primary central nervous system (CNS) lymphoma. Magnetic resonance imaging (MRI) of the brain showed a 4.7 cm hemorrhagic mass located at the corpus callosum, with surrounding edema with high-grade glioma features, as seen on Figure 2. Echocardiogram showed a right ventricular mobile mass representing vegetation, papillary fibroelastoma versus a thrombus. Workups for cardiac and CNS pathologies were not performed due to unstable patient hemodynamics. The patient was later started on IV flucytosine 25 mg/kg daily for 3 days. As the patient lacked clinical improvement, he was switched to IV fluconazole 1,200 mg daily for 6 days.
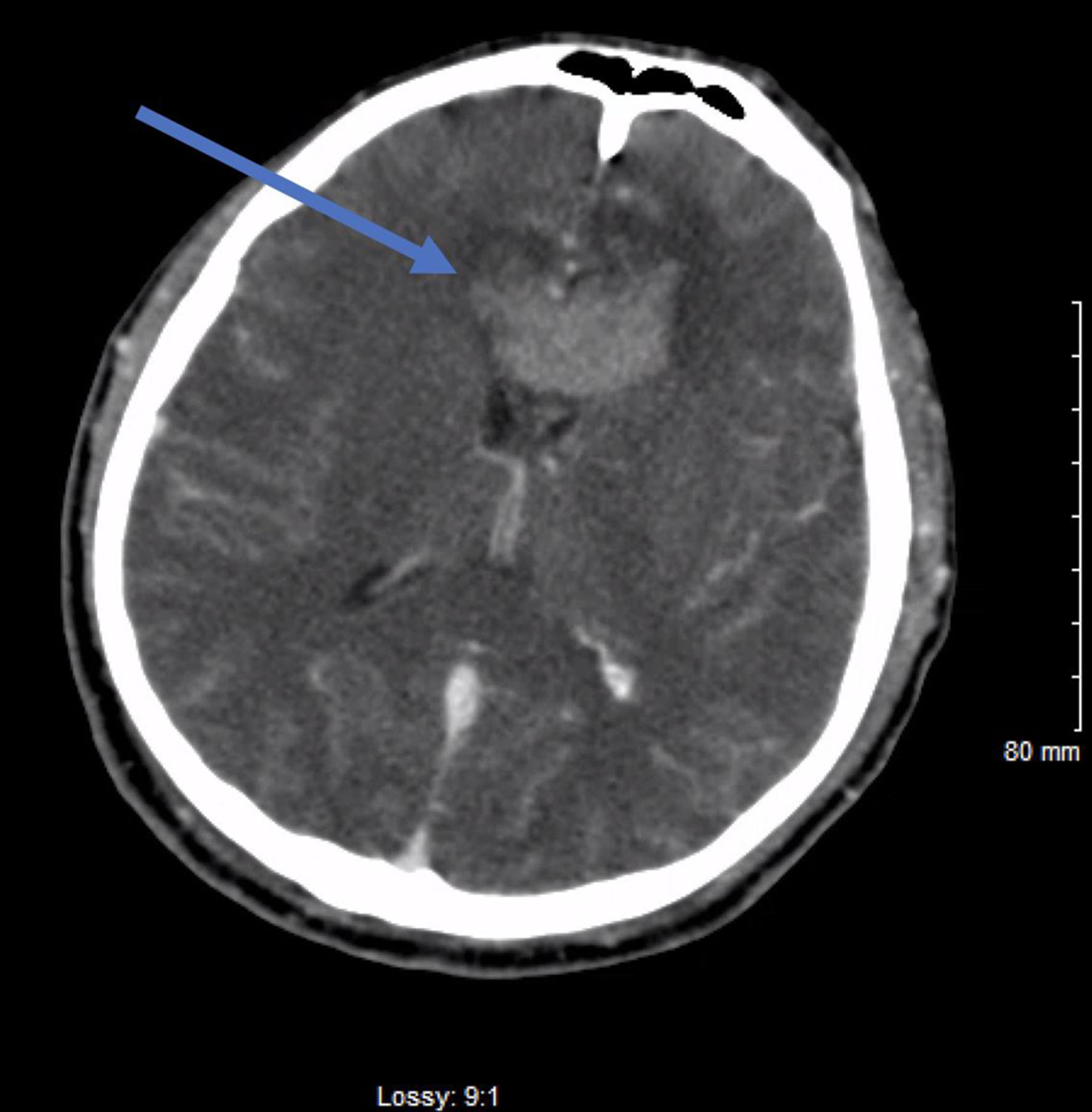 Click for large image | Figure 1. Computed tomography (CT) scan of the head with intravenous (IV) contrast, showing focal hemorrhage versus enhancing mass (blue arrow) involving the genu of the corpus callosum measuring 1.1 × 1.8 × 3.9 cm. |
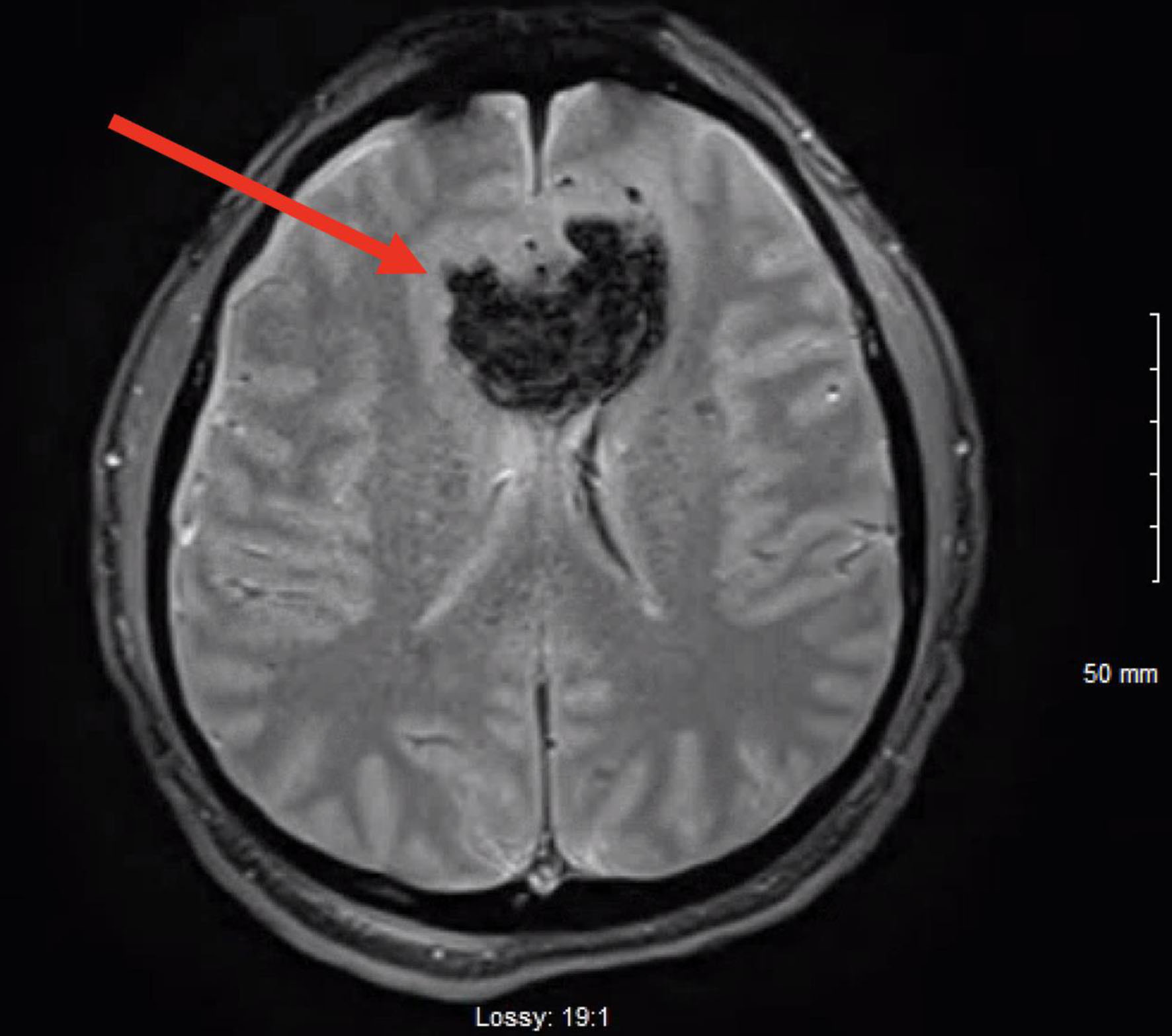 Click for large image | Figure 2. Magnetic resonance imaging (MRI) of the brain without intravenous (IV) contrast, showing large hemorrhagic mass extending across the splenium of the corpus callosum measuring 4.7 cm (red arrow) with surrounding edema. |
Follow-up and outcomes
After a 24-day hospital course, given the critical nature of the patient’s condition and lack of improvement, the decision to place the patient on comfort care was made by his surrogate decision maker. The patient was compassionately extubated and expired soon after.
| Discussion | ▴Top |
Coccidioidomycosis is an infection caused by the Coccidioides species. It usually exists as mycelia which use true septae as their mechanism of invasion and pathology. These cells take different forms to become infectious. Initially the mycelial cells autolyze and thin their cell walls while others are transformed into barrel-shaped, loosely adherent arthroconidia [3]. Hence, due to the loose adherence, the cells are easily airborne at any slight disturbance of the soil. The small size (2 to 5 µm) of the arthroconidia enables them to reach the right terminal bronchiole when inhaled [3]. Once inhaled, the arthroconidia transform into spherules. These spherules then mature and proceed to endosporulation stage forming multiple endospores which release upon rupture. These endospores mature into another endospore filled spherules which then rupture repeating the parasitic cycle. When endospore released in the environment they can transform into mycelial growth [3].
In susceptible/immunocompromised patients, the host response is subacute, compared to healthy individuals who are able to contain the infection within the lungs, which allows further extrapulmonary infection with the Coccidioides species [3]. The dissemination into extrapulmonary regions occurs through macrophage trafficking carrying the spores to different body areas. Interferon-γ, produced by Th1, is an integral part of the immune system’s defense against disseminated coccidioidomycosis. This is due to a direct correlation noticed amongst resolution of the disease and production of interferon-γ by lymphocytes. Microbial killing is achieved by through production of macrophages and other innate cells as a direct response to the Coccidioides antigen [4].
Due to the patient’s instability, we were unable to biopsy the corpus callosum mass extending into the left lateral ventricle; however, it presented with features consistent with primary CNS lymphoma. However, this brain mass could have also been a CNS lymphoma, glioblastoma or even a cryptococcoma. The cerebrospinal fluid (CSF) findings of Coccidioides IgG antibodies were consistent with CM. CNS dissemination is serious and usually presents as coccidioidal meningitis as well as encephalitis, mass-occupying lesions, brain abscesses, and aneurysms [5]. As per the CDC, a thorough workup includes serologic testing for IgM and IgG antibodies against Coccidioides in addition to obtaining cultures from blood, sputum, CSF and urine [6].
To bring into perspective the rarity of this infectious disease, a literature review was conducted on the number of case reports that have been published about patients with CM. We performed a systematic review for eligible case reports through a search on PubMed using the following terms “coccidioidomycosis meningitis”. The case reports included were published in English, between the years of January 2012 and December 2022 for subjects 19 years or older.
We found a total of 20 articles that were evaluated, which can be seen in Table 2 [7-17]. Five were excluded as they did not meet our inclusion criteria. One case was excluded as the diagnosis was never confirmed. Three were removed as they did not have meningeal spread. Here we review 14 individual cases of CM.
 Click to view | Table 2. Demographic Details, Diagnostic Information, Human Immunodeficiency Virus Status, and Outcomes for Patients Diagnosed With Coccidioidomycosis Meningitis (Review of Literature) |
We examined the age of the infected individuals and noticed the mean age of diagnosis was 42 years old. Four out of the 14 eligible cases were females (28.57%), with the remaining 10 of the 14 being males (71.42%). Many of the cases identified were located in California; however, values were unable to be calculated as some of the case reports did not highlight geographical locations. Out of the 14 cases, 13 were in HIV-negative individuals (92.8%), while only one was in an HIV-positive individual (7.14%). The recovery rate out of these 14 individuals was 10 (71.42%), while three expired (21.4%), and one was comatose (7.14%). There was one case highlighted by Patel et al, who described a 30-year-old pregnant female diagnosed with CM. With appropriate treatment, she had a full recovery. Interestingly enough, the placenta was found to have evidence of Coccidioides; however, the newborn had no signs of infection.
It is important to pursue a myriad of differential diagnoses when considering a severely immunocompromised patient. A differential diagnosis we considered on admission was TB. Given his immunocompromised state, appropriate testing for TB yielded negative results. Histoplasmosis, a dimorphic fungus, was a differential that was considered. Commonly found in soils and yeast forms, its portal of entry is through inhalation [18]. Patient was tested for histoplasmosis through urine studies and was found to be negative. Pneumocystis species are a type of fungus that are found in many people’s lungs and are generally under control in those individuals who are immunocompetent. However, in those patients who are immunocompromised, it can cause a severe pneumonia [19]. In our patient, we did a bronchoalveolar lavage and pneumocystis was not found within the secretions. Cryptococcus and aspergillus can also severely affect immunocompromised patients. These were also considered in our immunocompromised patient; however, tests for both fungi were found to be negative.
Before the highly active antiretroviral therapy (HAART) medication becoming an effective medication of HIV/AIDs, Coccidioides was a significant opportunistic infection for patients with HIV living in endemic regions as their immune responses were unable to control the viral replication and immune reconstitution without the use of HAART [18]. It is suggested in data that a peripheral CD4 count ≥ 250/µL can maintain an immune response against any coccidioidal manifestations [2]. Hence patients with HIV and a CD4 count ≥ 250/µL can be managed in the same way as immunocompetent individuals. The general treatment includes treatment with either fluconazole or itraconazole at a daily dose of 400 mg; however, itraconazole is not the drug of choice for coccidioidal meningitis, although there are some case series has been placed on oral itraconazole with stable disease [2].
Patients with CD4 count lower than 250/µL should receive antifungal rather than potent antifungal therapy [2]. More significantly, patients who have low CD4 count requiring hospitalization with severe disease require initial therapy with amphotericin B combined with triazole [2]. Furthermore, because only a few cases of immune response inflammatory syndrome (IRIS) occurred during HIV and coccidioidal infection, it is crucial to initiate potent antiretroviral therapy alongside the antifungal therapy which was done here for our patient when he started showing symptoms and lab values consistent with coccidioidal IRIS [2]. The most effective method in reducing the incidence and severity of coccidioidomycosis in HIV-infected patients is to start and maintain HAART therapy [2].
Learning points
We would like to highlight the importance of disseminated coccidioidomycosis and its appropriate workup. In an immunocompromised patient, if the suspicion for opportunistic infections exists, we suggest obtaining cultures of blood, urine, and CSF. We recommend obtaining an extensive workup to exclude other causes with similar presentations to coccidioidomycosis, such as tuberculosis, pneumocystis, cryptococcus, and toxoplasmosis.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
Written informed consent was obtained from the patient.
Author Contributions
HG participated in patient care, writing of the case report, revisions, and submission process. BO participated in patient care, writing of the case report and revisions. MG participated in patient care, writing of the case report and revisions. BM participated in patient care, writing of the case report and revisions. MH participated in patient care and revisions.
Data Availability
All data in our report was obtained from the patient’s hospitalization. Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Alcauskas T, Zablockiene B, Zablockis R, Svetikas L, Bilotaite L, Jancoriene L. Pulmonary coccidioidomycosis: a case report and literature review. Medicina (Kaunas). 2022;58(5):655.
doi pubmed pmc - Ampel NM. The treatment of coccidioidomycosis. Rev Inst Med Trop Sao Paulo. 2015;57 Suppl 19:51-56.
doi pubmed pmc - Akram SM, Koirala J. Coccidioidomycosis. In: StatPearls. Treasure Island (FL), 2022.
- Tsai M, Thauland TJ, Huang AY, Bun C, Fitzwater S, Krogstad P, Douine ED, et al. Disseminated coccidioidomycosis treated with interferon-gamma and dupilumab. N Engl J Med. 2020;382(24):2337-2343.
doi pubmed pmc - Spickler AR. Coccidioidomycosis. 2021. Retrieved from http://www.cfsph.iastate.edu/DiseaseInfo/factsheets.php.
- Centers for Disease Control and Prevention. Information for healthcare professionals about valley fever (Coccidiomycosis). 2021. Centers for Disease Control and Prevention. Retrieved December 16, 2022, from https://www.cdc.gov/fungal/diseases/coccidioidomycosis/health-professionals.html.
- Mao Y, Li X, Lou H, Shang X, Mai Y, Yang L, Peng F, et al. Detection of Coccidioides posadasii in a patient with meningitis using metagenomic next-generation sequencing: a case report. BMC Infect Dis. 2021;21(1):968.
doi pubmed pmc - Davis MR, Chang S, Gaynor P, McCreary EK, Allyn P. Isavuconazole for treatment of refractory coccidioidal meningitis with concomitant cerebrospinal fluid and plasma therapeutic drug monitoring. Med Mycol. 2021;59(9):939-942.
doi - Phelps RRL, Lu AY, Lee AT, Yue JK, Winkler EA, Raygor KP, Oh T, et al. Cerebrovascular complications of coccidioidomycosis meningitis: Case report and systematic review. J Clin Neurosci. 2020;80:282-289.
doi - Lang R, Stokes W, Lemaire J, Johnson A, Conly J. A case report of Coccidioides posadasii meningoencephalitis in an immunocompetent host. BMC Infect Dis. 2019;19(1):722.
doi pubmed pmc - Buchanan IA, Ravina K, Strickland B, Fredrickson V, She R, Mathew A, Rennert R, et al. Multiple intracranial aneurysms from coccidioidal meningitis: case report featuring aneurysm formation and spontaneous thrombosis with literature review. World Neurosurg. 2019;121:117-123.
doi - Stewart ER, Eldridge ML, McHardy I, Cohen SH, Thompson GR, 3rd. Liposomal amphotericin B as monotherapy in relapsed coccidioidal meningitis. Mycopathologia. 2018;183(3):619-622.
doi - Garoon RB, Foroozan R, Vaphiades MS. Don't drink in the valley. Surv Ophthalmol. 2017;62(3):383-386.
doi - Nelson S, Vytopil M. Recurrence of coccidioidal meningitis after discontinuation of fluconazole. JAMA Neurol. 2013;70(12):1586.
doi - Tan LA, Kasliwal MK, Nag S, O'Toole JE, Traynelis VC. Rapidly progressive quadriparesis heralding disseminated coccidioidomycosis in an immunocompetent patient. J Clin Neurosci. 2014;21(6):1049-1051.
doi - Patel S, Lee RH. The case of the sinister spores: the patient was hospitalized for a menacing infection in the second trimester of pregnancy. Am J Obstet Gynecol. 2013;208(5):417.e411.
doi pubmed - Trible R, Edgerton N, Hayek S, Winkel D, Anderson AM. Antiretroviral therapy-associated coccidioidal meningitis. Emerg Infect Dis. 2013;19(1):163-165.
doi pubmed pmc - Yadav P, Kumar D, Bohra GK, Garg MK, Bharti JN, Purohit AH, Meena DS. Progressive disseminated histoplasmosis in idiopathic CD4 lymphocytopenia an underdiagnosed combination - a case report. Med Pharm Rep. 2022;95(2):209-213.
doi pubmed pmc - Tasaka S. Pneumocystis pneumonia in human immunodeficiency virus-infected adults and adolescents: current concepts and future directions. Clin Med Insights Circ Respir Pulm Med. 2015;9(Suppl 1):19-28.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


