| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 6, June 2023, pages 200-203
Identifying the Cause of Acute Left-Sided Visual Loss: A Clinical Dilemma
Anirudh R. Damughatlaa, b, c, g, Vanessa Milan-Ortiza, b, Pragna Koletid, Myrna M. Milan-Ortize, Sudhir Reddy Pashamf, Abhishek R. Damughatlac, Saivaishnavi Kamathama, b, Kareem Bazzya, b
aDepartment of Internal Medicine, Wayne State University & Detroit Medical Center, Detroit, MI, USA
bDepartment of Internal Medicine, John D. Dingell Veterans Affairs Medical Center, Detroit, MI, USA
cDepartment of Biomedical Engineering, The Ohio State University, Columbus, OH, USA
dDepartment of Internal Medicine, Suburban Community Hospital, Norristown, PA, USA
eTransitional Program, Metropolitan Hospital Dr. Pila, Ponce, Puerto Rico
fDepartment of Internal Medicine, Guthrie Robert Packer Hospital, Sayre, PA, USA
gCorresponding Author: Anirudh R. Damughatla, Department of Internal Medicine, Wayne State University & Detroit Medical Center, Detroit, MI, USA
Manuscript submitted April 17, 2023, accepted June 5, 2023, published online June 29, 2023
Short title: Cause of Acute Left-Sided Visual Loss
doi: https://doi.org/10.14740/jmc4093
| Abstract | ▴Top |
Given the global increase in the incidence of head and neck cancers over the last decade, the use of chemoradiation has also increased. It is well known that chemotherapy/radiation are established standard therapies in head and neck cancers, especially in patients who are not candidates for surgery. Despite this increase in chemoradiation therapies in head and neck cancers, there is a lack of established guidelines on the surveillance and screening of these patients for long-term complications. We present an interesting case of acute left eye blindness in a veteran patient with a history of laryngeal cancer status post chemoradiation and in the setting of a left ventricular (LV) thrombus on anticoagulation resulting in a diagnostic challenge determining the etiology. This case emphasizes the need for thorough patient-centered annual evaluation, thus providing an opportunity for early noninvasive or minimally invasive intervention.
Keywords: Acute left eye blindness; Laryngeal cancer status post chemoradiation; LV thrombus; Large vessel; Carotid stenosis; Stenosis due to chemoradiation
| Introduction | ▴Top |
Laryngeal cancer is one of the most common cancers of the head and neck, with an incidence of around 13,000 yearly in the United States and representing one-third of head and neck cancers [1]. The cancerous lesions are classified by location, either supraglottic, glottic, or subglottic, as well as by invasive characteristics and nodal metastases of the primary tumor. Treatment modalities differ by the tumor’s location and TNM staging; however, as treatments have advanced, the goal has been to emphasize laryngeal preserving modalities and move away from total laryngectomy. Radiation therapy is a standard option for all stages and one of the mainstay modalities of therapy for advanced cancers at the T3 and T4 stages [2]. Despite preserving the laryngeal architecture, radiation therapy to the neck is not without its particular side effects, with mucosal injury causing dysphagia and voice dysfunction in the short term [3].
Furthermore, in addition to causing strictures, it has been suggested that long-term effects may stem from collateral radiation to the nearby carotid arteries. Radiation induces endothelial damage, proliferation, and fibrosis, which are thought to be mechanisms for accelerating atherosclerosis of the carotid arteries, leading to an increased risk of stroke and transient ischemic attacks [4]. We present an interesting case of acute left eye blindness in a veteran patient with a history of laryngeal cancer status post chemoradiation and in the setting of a left ventricular (LV) thrombus on anticoagulation resulting in a diagnostic challenge in determining the etiology.
| Case Report | ▴Top |
Investigations
Our patient is a 61-year-old male with a history of heart failure with reduced ejection fraction, left ventricle thrombus, left-sided ischemic stroke without any residual weakness, and history of laryngeal adenocarcinoma status post chemoradiation 15 years ago, who presented with sudden left-sided visual loss. He presented initially to the eye clinic due to sudden vision loss and was sent to the emergency department (ED) for further evaluation with neuroimaging. Home medications included apixaban twice daily (BID), aspirin 81 mg daily, and atorvastatin 40 mg nightly. On initial examination, the left eye was nonreactive to light with an absent consensual pupillary response. The rest of the neurological exam was unremarkable, including motor strength and sensation in the bilateral upper and lower extremities.
Diagnosis
A head computed tomography (CT) scan showed no acute intracranial abnormality with remote chronic ischemic changes. However, head and neck computed tomography angiography (CTA) demonstrated complete occlusion of the left vertebral artery from its origin to the cervical segment and complete occlusion of the internal carotid artery (ICA) at its origin with reconstitution at the petrous and cavernous segments (Fig. 1). Brain magnetic resonance imaging (MRI) showed no acute infarct but the presence of small old infarcts in the left occipital and frontal lobes. A fundoscopic exam demonstrated optic nerve edema and evidence of suspected ophthalmic artery occlusion.
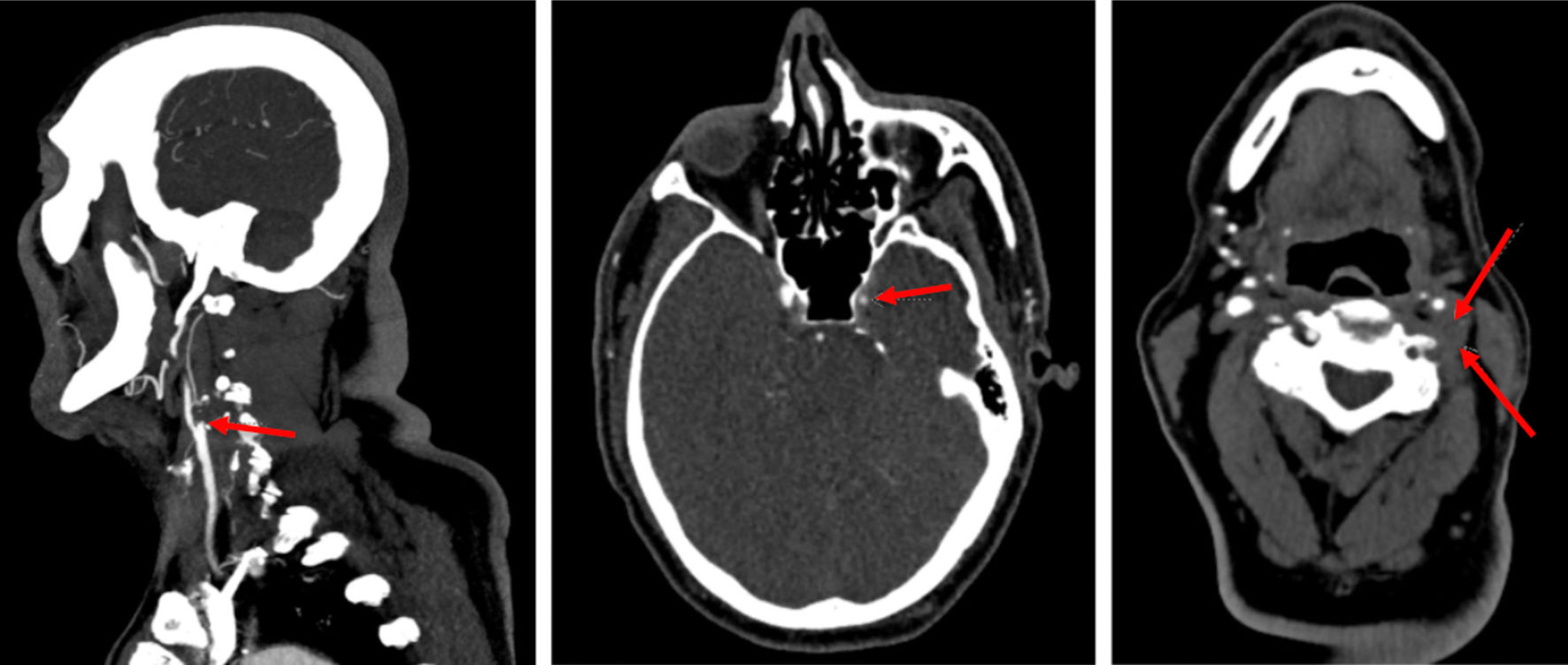 Click for large image | Figure 1. CTA of head and neck with red arrows in each image demonstrating complete occlusion of vertebral and internal carotid arteries. CTA: computed tomography angiography. |
A two-dimensional (2D) echo demonstrated a massive LV thrombus, unchanged from 2 months ago, at which time the patient also had cardiac MRI (Fig. 2). The thrombus was noted to be 2.2 × 4.1 cm in size, and the patient notes daily adherence to his apixaban BID and aspirin. The challenge was determining whether this presentation of ophthalmic artery occlusion was cardioembolic related to the LV thrombus and hence a failure of anticoagulation or related to the occlusive carotid disease.
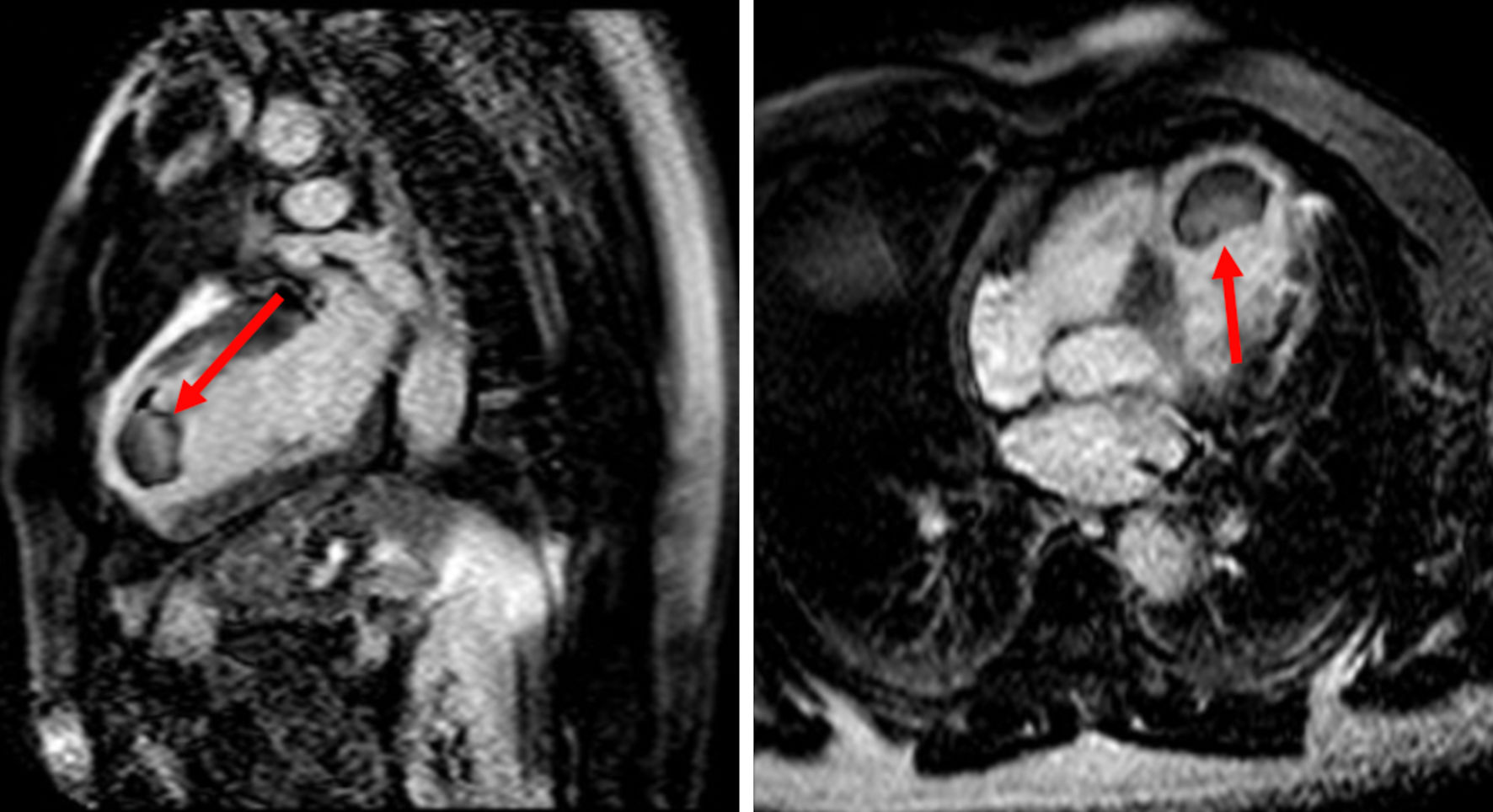 Click for large image | Figure 2. MRI cardiac function with and without contrast with red arrow showing the thrombus. MRI: magnetic resonance imaging. |
Moreover, the patient developed sudden, transient right-sided weakness during the hospital course. CT perfusion (Fig. 3) demonstrated extensive ischemic penumbra in the left cerebral hemisphere consistent with acute decompensated chronic occlusion of the left ICA.
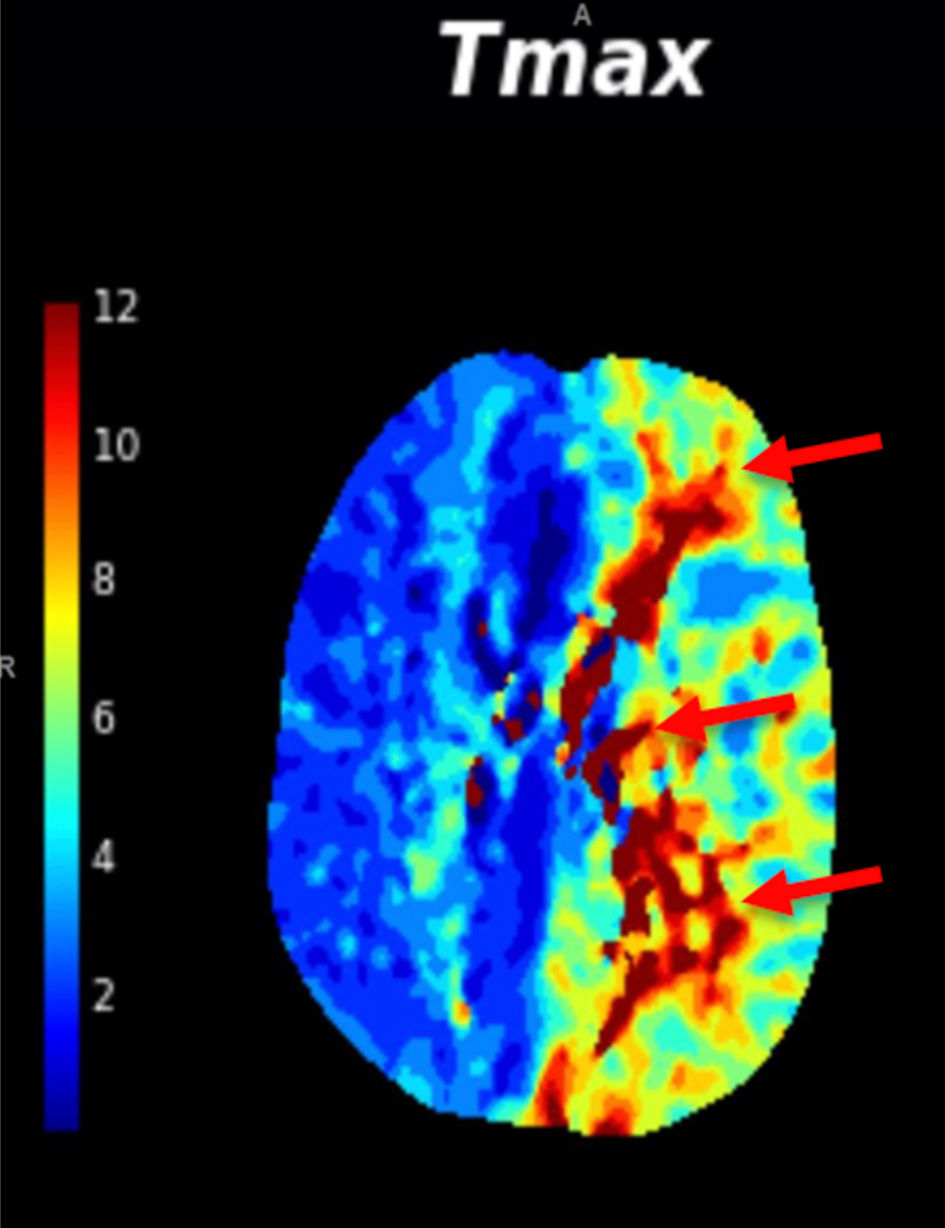 Click for large image | Figure 3. CT perfusion scan showing the areas of hypoperfusion indicated by the red arrows. CT: computed tomography. |
Treatment/follow-up and outcomes
Given the development of contralateral hemispheric symptoms, it was retrospectively determined that the acute visual loss was related to carotid artery disease resulting in a late complication of localized radiation for laryngeal cancer. The patient was transferred to a tertiary facility for endovascular intervention. Hence, acute visual loss accompanied by contralateral deficits is obstructive carotid stenosis until proven otherwise.
| Discussion | ▴Top |
When literature was reviewed for the incidence of carotid artery stenosis in patients who underwent radiotherapy for head and neck cancer, it was reported to be 18% to 38%, while in non-irradiated patients was 9.2% [5]. A logistical regression analysis performed by Cheng et al [6] showed that age (> 60), cerebrovascular symptoms, the interval from irradiation (> 5 years), and nasopharynx and larynx cancer were found to be independent significant (P < 0.05) predictors of 70% or more significant ICA/common carotid artery (CCA) stenosis. Moreover, a prospective cross-sectional study by Akhavan et al found a significant correlation between carotid artery stenosis and age (P = 0.026) [7].
As per the literature review, there does not appear to be a specific length of time for the onset of vascular damage post radiotherapy. Trojanowski et al performed a retrospective study that demonstrated that the mean interval from radiotherapy to symptomatic stenosis was 3 to 7 years; however, some cases have been seen as early as 2 years post radiotherapy [8]. A systematic review and meta-analysis concluded that the yearly incidence of carotid stenosis > 50% increased yearly during the first 3 years following radiotherapy [9]. Cheng et al also demonstrated an increased risk of having severe stenosis in patients irradiated 5 years ago than in those who received a shorter period of radiation [6].
When investigating the pathophysiology of post-radiation vascular changes, several studies have demonstrated that the first apparent vascular change appreciated in patients receiving radiation to the head and neck is the increased intima-media thickness. It was also noted that post-radiation lesions were multifocal and occupied significantly longer segments of arteries compared to lesions caused by atherosclerosis, which are usually unifocal, located in the CCA bifurcation and the initial segment of the ICA [8]. Van Aken et al performed a prospective cohort study in which it was determined that ischemic cerebrovascular events risk was associated with the radiation dose applied to the carotid arteries [10]. Contrary to these studies, Akhavan et al and Carpenter et al showed no relationship between carotid artery radiation dose and the extent of stenosis [7, 11].
Despite variability in the literature regarding the duration of onset to vascular damage post radiotherapy or radiation dose-dependent extent of stenosis, it is widely accepted that radiation increases the prevalence of carotid artery stenosis. When considering treatment options, it has been noted that percutaneous endovascular therapy is the preferred therapeutic modality in patients with carotid artery stenosis who underwent head and neck radiotherapy [8]. This is because plaques are formed in numerous areas of the carotid artery requiring multiple stent placements. Several studies report that restenosis is seen more frequently in irradiated patients than in non-irradiated patients [8].
Given the clinical significance of carotid arterial disease post chemoradiation therapy, it is essential for risk stratification and annual screening, including carotid duplex in patients before and after undergoing chemoradiation therapy for head and neck cancers, to provide optimal patient management. We believe these measures help identify pre-existing disease, monitor treatment-related changes, and facilitate early intervention to reduce the risk of complications such as stroke.
Learning point
Our case highlights that acute visual loss accompanied by contralateral deficits is obstructive carotid stenosis until proven otherwise in a setting of LV thrombus and a history of head and neck chemoradiation. Moreover, it is well reported in the literature that the prevalence of carotid artery stenosis increases significantly post chemoradiation therapy in head and neck cancers; however, there are no guidelines to address these patients. This case emphasizes the need for thorough patient-centered evaluation annually, thus providing an opportunity for early noninvasive or minimally invasive intervention.
Acknowledgments
We have no acknowledgments to make.
Financial Disclosure
There are no financial interests to disclose.
Conflict of Interest
There is no conflict of interest in the manuscript.
Informed Consent
Informed consent was obtained from the patient for case publication.
Author Contributions
Anirudh R. Damughatla DO, took care of the patient, wrote: the abstract, patient’s case, and discussion, and added figures and references. Vanessa Milan-Ortiz MD, cared for the patient and contributed to the case description and discussion. Pragna Koleti MD, contributed to the introduction and discussion and added references. Myrna M. Milan-Ortiz MD, contributed to the discussion and added references. Sudhir Reddy Pasham MD contributed to the discussion and added references. Abhishek R. Damughatla contributed to the abstract, references, and figures. Saivaishnavi Kamatham MD, contributed to the abstract, references, figures, and edited manuscript. Kareem Bazzy MD attending, took care of the patient and reviewed and edited the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Koroulakis A, Agarwal M. Laryngeal cancer. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
pubmed - Obid R, Redlich M, Tomeh C. The treatment of laryngeal cancer. Oral Maxillofac Surg Clin North Am. 2019;31(1):1-11.
doi pubmed - Hutcheson KA, Lewin JS. Functional outcomes after chemoradiotherapy of laryngeal and pharyngeal cancers. Curr Oncol Rep. 2012;14(2):158-165.
doi pubmed pmc - Gujral DM, Chahal N, Senior R, Harrington KJ, Nutting CM. Radiation-induced carotid artery atherosclerosis. Radiother Oncol. 2014;110(1):31-38.
doi pubmed - Fernandez-Alvarez V, Lopez F, Suarez C, Strojan P, Eisbruch A, Silver CE, Mendenhall WM, et al. Radiation-induced carotid artery lesions. Strahlenther Onkol. 2018;194(8):699-710.
doi pubmed - Cheng SW, Wu LL, Ting AC, Lau H, Lam LK, Wei WI. Irradiation-induced extracranial carotid stenosis in patients with head and neck malignancies. Am J Surg. 1999;178(4):323-328.
doi pubmed - Akhavan A, Farghadani M, Emami H, Naderi Beni Z, Naderi Beni A. Effects of neck radiation on result of doppler sonography of carotid arteries in head and neck cancer patients. J Stroke Cerebrovasc Dis. 2021;30(4):105607.
doi pubmed - Trojanowski P, Sojka M, Trojanowska A, Wolski A, Roman T, Jargiello T. Management of radiation induced carotid stenosis in head and neck cancer. Transl Oncol. 2019;12(8):1026-1031.
doi pubmed pmc - Texakalidis P, Giannopoulos S, Tsouknidas I, Song S, Rivet DJ, Reiter ER, Reavey-Cantwell J. Prevalence of carotid stenosis following radiotherapy for head and neck cancer: A systematic review and meta-analysis. Head Neck. 2020;42(5):1077-1088.
doi pubmed - van Aken ESM, van der Laan HP, Bijl HP, Van den Bosch L, van den Hoek JGM, Dieters M, Steenbakkers R, et al. Risk of ischaemic cerebrovascular events in head and neck cancer patients is associated with carotid artery radiation dose. Radiother Oncol. 2021;157:182-187.
doi pubmed - Carpenter DJ, Mowery YM, Broadwater G, Rodrigues A, Wisdom AJ, Dorth JA, Patel PR, et al. The risk of carotid stenosis in head and neck cancer patients after radiation therapy. Oral Oncol. 2018;80:9-15.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


