| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 5, May 2023, pages 169-173
A Rare Case of Anterograde Gastroduodenal Intussusception Caused by Migrated Percutaneous Endoscopic Gastrostomy Feeding Tube
Abdelwahap Elghezewia, Mohamed Hammada, Mujtaba Mohamedb, d, Peter Chiricoc, Wesam Frandahb
aDepartment of Medicine, Joan C. Edwards School of Medicine, Marshall University, Huntington, WV 25701, USA
bSection of Gastroenterology and Hepatology, Joan C. Edwards School of Medicine, Marshall University, Huntington, WV 25701, USA
cDepartment of Radiology, Joan C. Edwards School of Medicine, Marshall University, Huntington, WV 25701, USA
dCorresponding Author: Mujtaba Mohamed, Section of Gastroenterology and Hepatology, Joan C. Edwards School of Medicine, Marshall University, Huntington, WV 25701, USA
Manuscript submitted April 20, 2023, accepted May 16, 2023, published online May 31, 2023
Short title: Gastroduodenal Intussusception by PEG Tube
doi: https://doi.org/10.14740/jmc4101
| Abstract | ▴Top |
Gastroduodenal intussusception is a critical condition in which stomach protrudes into the duodenum. It is a very rare condition in adults. Most common causes include intra luminal lesions in the stomach including benign or malignant tumors of the stomach. Most common tumors included are gastrointestinal stromal tumors (GISTs), gastric carcinoma, gastric lipoma, gastric leiomyoma, and gastric schwannoma. It is extremely rare to be caused by migration of percutaneous feeding tube. A 50-year-old woman with a past medical history (PMH) of dysphagia status post percutaneous endoscopic gastrostomy (PEG) tube, history of spastic quadriplegia, presented with acute nausea, vomiting and abdominal distention, and was found to have gastroduodenal intussusception in computed tomography (CT) scan. Condition resolved after retracting PEG tube. Endoscopy did not reveal any intra luminal lesions. External fixation using Avanos Saf-T-Pexy T-fasteners was performed to prevent recurrence of this condition. Most common of causes of gastroduodenal intussusception are GIST tumors of stomach. CT abdomen is the most accurate test and upper endoscopy is needed to rule out any intra luminal causes. Treatment of choice is either endoscopic or surgical resection. External fixation is essential to prevent recurrence.
Keywords: Gastroduodenal intussusception; Percutaneous gastrostomy tube; Treatment
| Introduction | ▴Top |
Anterograde gastroduodenal intussusception is invagination of the stomach into duodenum. It is a rare finding in adults, and the rarest form of intussusception, representing only 10% of all cases of intussusception [1]. Most common causes of gastroduodenal intussusception are gastrointestinal stromal tumors (GISTs), gastric carcinoma, gastric lipoma, gastric leiomyoma, and gastric schwannoma [2-6]. Hsieh et al reported in a systemic review of the relevant literature regarding gastroduodenal intussusception and found that GISTs were the most common etiology, accounting for more than half of these cases in adults [7]. Isolated duodenal intussusception is also very rare since duodenum is fixed in retroperitoneum [8]. It is caused by benign or malignant tumors of the duodenum such as adenomas, hamartomas, or stromal tumors [9], and malrotation abnormalities [10, 11]. Meckel’s diverticulum was reported as a cause as well. It is extremely rare for gastroduodenal intussusception to be caused by migration of percutaneous gastrostomy tube. Herein, we present a rare case of adult gastroduodenal intussusception due to migrated percutaneous gastrostomy tube.
| Case Report | ▴Top |
A 50-year-old woman with a past medical history of traumatic brain injury complicated by quadriplegia, spasticity on baclofen 100 mg orally daily, muscle contractures, dysphagia status post percutaneous endoscopic gastrostomy (PEG) tube (Boston scientific Endovive feeding tube 24 Fr) in October 2022, with external marking at the time of insertion of 3.5 cm and external bumper used for external fixation, seizure disorder on levetiracetam 500 mg twice daily, presented to the emergency department in January 2023 from nursing home due to nausea, vomiting and abdominal distention. Physical examination revealed that vital signs: heart rate 128 beats per minute (bpm), blood pressure 125/90 mm Hg, respiratory rate 20/min, oxygen saturation 96% on room air, weight 40.9 kg. The patient appeared to be cachectic. Muscle spasticity in upper and lower limbs was noted, and contractures noted on both lower limbs. The abdominal exam revealed distended abdomen with mild leak around PEG. The external bumper of feeding tube was loose and numerical markings of the feeding tube were absent. A short segment of PEG tube was hanging outside the anterior abdominal wall. Otherwise, the patient had a foley catheter in place. Blood tests showed: white blood cell counts 38 (4.5 - 10), hemoglobin 13.1 (reference range of 14 - 18 g/dL), platelets 308 (150 - 440 × 103/µL), and mean corpuscular volume (MCV) 86 fL (80 to 100 fL), sodium 131 (135 - 145 mEq/L), creatinine 1.2 (0.6 - 1.1 mg/dL), normal serum aminotransferases, procalcitonin 5.08 (a concentration of < 0.5 ng/mL represents a low risk of severe sepsis and/or septic shock, a concentration of more than 2 ng/mL represents a high risk of severe sepsis and/or septic shock). Arterial blood gas revealed: PCO2 30 mm Hg, PO2 96 mm Hg, oxygen saturation 98%, and serum lactic acid 4.6 mmol/L (0.7 - 2.1 mmol/L). Radiological data included computed tomography (CT) scan of the abdomen showing dilated duodenum (6 cm), and gastroduodenal intussusception within the duodenum. A swirling of the mesentery was seen, as well suggesting coexistent volvulus in the same location. The stomach was distended and full of fluids (Figs. 1, 2). There was dilation of intra and extra hepatic biliary tracts. The feeding tube was pulled back and placed with gravity, around 1,100 mL of bilious fluid was drained, and abdominal distention was improved. Repeat CT scan showed improvement of duodenal intussusception and volvulus. On the following day, the patient underwent upper endoscopy which revealed an intact gastrostomy with a patent G-tube present in the gastric body. Two non-bleeding linear duodenal ulcers with no stigmata of bleeding were seen in the second and third part of duodenum. The largest lesion was 16 mm in largest dimension (Fig. 3). There was no endoscopic evidence of stenosis, mass or deformity in the entire stomach and duodenum. An external fixation was applied using Avanos Saf-T-Pexy T-fasteners to prevent recurrence of this complication. The patient was discharged back to nursing home 2 days later.
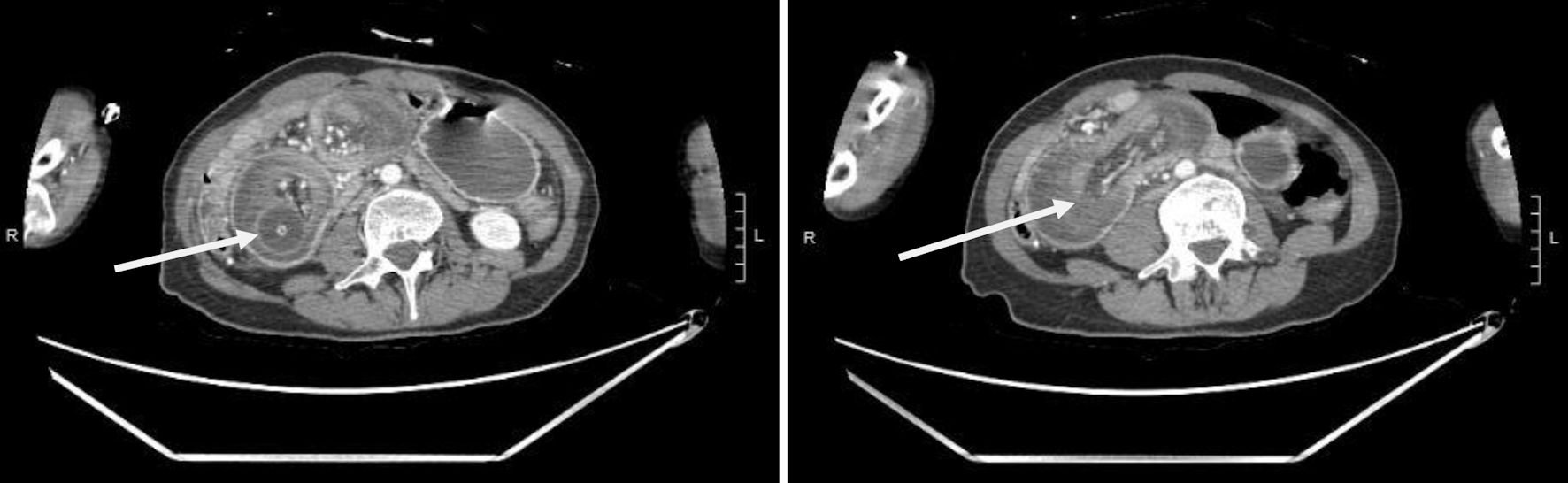 Click for large image | Figure 1. Coronal images showing duodenal intussusception and the migrating percutaneous gastrostomy tube (arrows). |
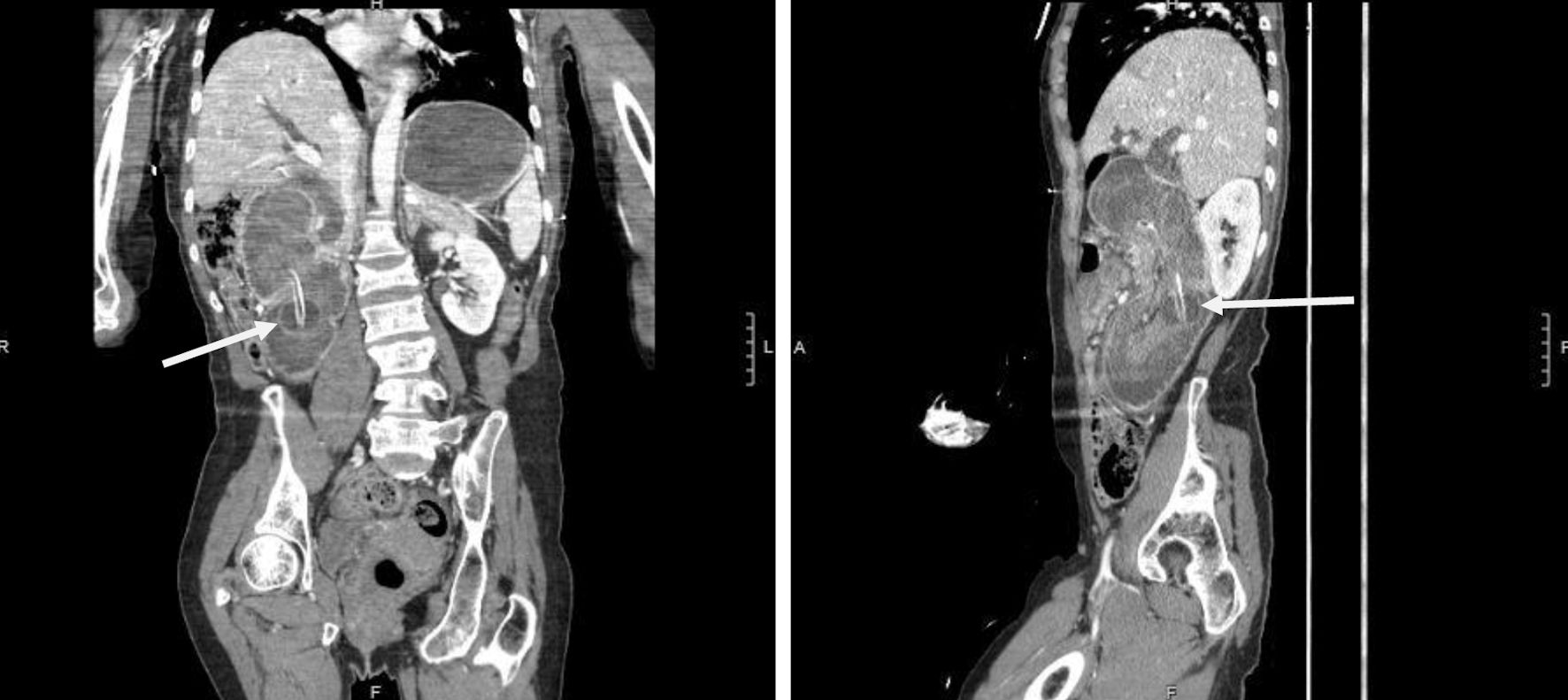 Click for large image | Figure 2. Sagittal section image showing migrating percutaneous gastrostomy tube causing duodenal obstruction and dilated stomach (arrows). |
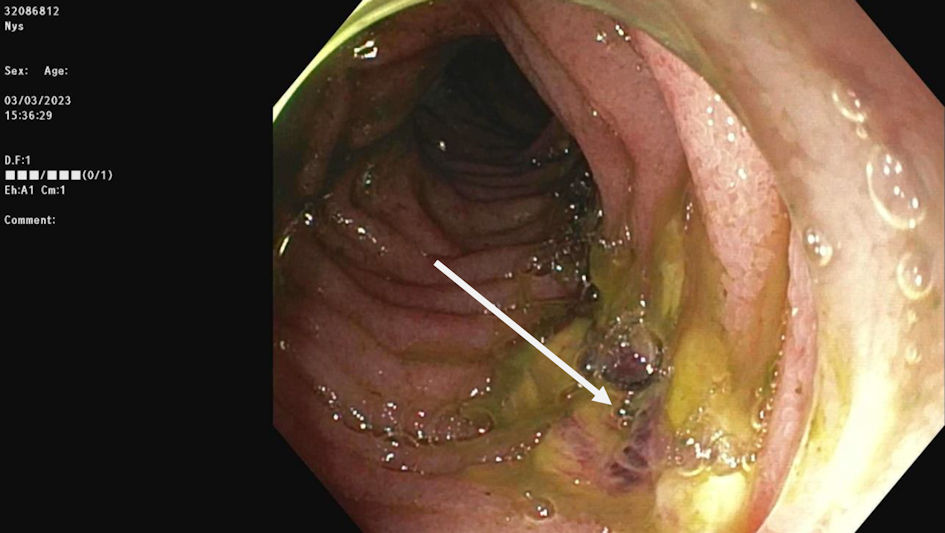 Click for large image | Figure 3. Linear nonbleeding ulcer at the third part of the duodenum caused by migrating percutaneous gastrostomy tube. |
| Discussion | ▴Top |
Gastroduodenal intussusception is an extremely rare presentation. Mostly it is caused by gastric tumors, resulting in prolapse of the tumor and subsequent invagination of a portion or the full thickness of the gastric wall into the duodenum [12, 13]. Gastric stromal tumors were reported to be the most common cause [7]. Gastroduodenal intussusception caused by migration of percutaneous feeding tube is even rarer clinical presentation. Most of reported cases were retrograde jejunogastric intussusception causing small bowel obstruction due to PEG tubes, as a result of the tube migrating forward into jejunum and acting as a leading point [14]. It is not very well understood the exact underlying mechanism of intussusception, but it was hypothesized that it is caused by a not properly fixed tube which can migrate away from abdominal wall through gastrostomy tube, as a result of normal peristalsis [15]. These further pushes stomach antrum into duodenum, resulting in antegrade intussusception [15]. Our case was an anterograde gastroduodenal intussusception. In literature review, only one case was reported by Alomari et al [16]. Our case and previously reported case are both women [16].
Endoscopic insertion of a gastrostomy tube was first introduced in 1980 by Gauderer et al [17]. It has increasingly become the method of choice to obtain long-term gastric access. Approximately 10% of the institutionalized elderly depend on PEG tubes for feeding [18], with an annual estimate of 100,000 to 125,000 PEG tubes being placed in the United States [19]. It is important to be aware of complications related to PEG tube while caring for those patients. Serious complications include tube migration, perforation, bleeding, and infections. To this date only one case was previously reported of gastroduodenal intussusception caused by feeding tube migration.
Clinical presentation of gastroduodenal intussusception is usually nonspecific, and symptoms can be acute or chronic or intermittent intestinal obstruction [20]. Most common presentation includes blood in stool, anemia, low-grade fever, weight loss, or abdominal lumps [20]. In acute settings it can present as bowel obstruction with nausea and vomiting. Obstructive jaundice and chronic pancreatitis can occur when hepatopancreatic ampulla is involved [10]. In this patient presentation was acute onset of abdominal pain, nausea, vomiting and abdominal distention. Hepatopancreatic ampulla was involved evidenced by dilation of intra and extra hepatic biliary tracts. No jaundice or abnormal liver functions in this patient was probably due to rapid onset and rapid improvement after pulling the feeding tube back.
Most accurate test to diagnose gastroduodenal intussusception is CT abdomen [21]. Classic symptoms seen in CT include “target”, “doughnut”, or “sausage-shaped” signs [22]. The role of endoscopy is to aid diagnosis in case of intra luminal lesions (polyps, tumors ulcers, adenomas) and to rule out any gastroduodenal cancer. In this case endoscopy was performed after pulling feeding tube back. Two linear nonbleeding ulcers were seen which were believed to be caused by the migrating feeding tube. No polyps, masses or hamartomas were seen in the stomach or duodenum.
Adult gastroduodenal intussusception is an urgent condition and should be treated by surgery without delay [3]. Treatment includes endoscopic resection of any intra luminal lesion that maybe cause it, and laparotomy or laparoscopy. Mucosal resection should be done in lesions confined to mucosal layers and less than 2 cm in size. Surgical resection is recommended in lesions more than 2 cm in size [22]. In this case complete resolution was achieved by pulling back the feeding tube. Early diagnosis, pulling and repositioning tube was important in preventing late complications such as bowel ischemia and perforation in this case.
It is important to emphasize the relevance of external fixation to prevent this complication from recurrence. We used Avanos Saf-T-Pexy T-fasteners. It is a T-fastener with absorbable suture designed to secure the position of the stomach against the anterior abdominal wall.
Conclusions
Gastroduodenal intussusception in adults is an extremely rare condition with nonspecific clinical manifestation. Most common reason is GISTs. It is even rarer to be caused by migration of percutaneous feeding tube. Poor external fixation can result in this complication. Most common presentation is nausea and vomiting. CT abdomen is the most accurate test, and upper endoscopy is needed to rule out any intra luminal causes. Treatment of choice is either endoscopic resection or surgical resection depending on the size and depth of extension of lesion into luminal wall. Proper external fixation of percutaneous feeding tube is essential to prevent recurrence.
Acknowledgments
We would like to thank our library staff at the Cabell Huntington Hospital for supplying us with articles to complete this manuscript.
Financial Disclosure
This project was not supported by any grant or funding agency.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Informed Consent
The patient described in the case report had given informed consent for the case report to be published.
Author Contributions
Each author has individually been involved and participated in drafting the manuscript and revising it critically for important intellectual content and has given final approval of the version to be published. Each has agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. WF and PC encouraged MM, AE, and MH to learn about duodenal intussusception. All authors discussed the medical literature. MM and AE presented the idea, MH, and AE wrote the manuscript with input from all authors.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg. 1970;172(2):306-310.
doi pubmed pmc - Hobbs WH, Cohen SE. Gastroduodenal invagination due to a submucous lipoma of the stomach. Am J Surg. 1946;71:505-518.
doi pubmed - Crowther KS, Wyld L, Yamani Q, Jacob G. Case report: gastroduodenal intussusception of a gastrointestinal stromal tumour. Br J Radiol. 2002;75(900):987-989.
doi pubmed - Suda T, Hodo Y, Shirota Y. Gastroduodenal intussusception of a gastric carcinoma. Dig Endosc. 2019;31(2):e38-e39.
doi pubmed - Vinces FY, Ciacci J, Sperling DC, Epstein S. Gastroduodenal intussusception secondary to a gastric lipoma. Can J Gastroenterol. 2005;19(2):107-108.
doi pubmed - Yang JH, Zhang M, Zhao ZH, Shu Y, Hong J, Cao YJ. Gastroduodenal intussusception due to gastric schwannoma treated by Billroth II distal gastrectomy: one case report. World J Gastroenterol. 2015;21(7):2225-2228.
doi pubmed pmc - Hsieh YL, Hsu WH, Lee CC, Wu CC, Wu DC, Wu JY. Gastroduodenal intussusception caused by gastric gastrointestinal stromal tumor: A case report and review of the literature. World J Clin Cases. 2021;9(4):838-846.
doi pubmed pmc - Hirata M, Shirakata Y, Yamanaka K. Duodenal intussusception secondary to ampullary adenoma: A case report. World J Clin Cases. 2019;7(14):1857-1864.
doi pubmed pmc - Watanabe F, Noda H, Okamura J, Toyama N, Konishi F. Acute pancreatitis secondary to duodenoduodenal intussusception in duodenal adenoma. Case Rep Gastroenterol. 2012;6(1):143-149.
doi pubmed pmc - Gardner-Thorpe J, Hardwick RH, Carroll NR, Gibbs P, Jamieson NV, Praseedom RK. Adult duodenal intussusception associated with congenital malrotation. World J Gastroenterol. 2007;13(28):3892-3894.
doi pubmed pmc - Meshikhes AW, Al-Momen SA, Al Talaq FT, Al-Jaroof AH. Adult intussusception caused by a lipoma in the small bowel: report of a case. Surg Today. 2005;35(2):161-165.
doi pubmed - Meyers MA. Gastroduodenal intussusception. Am J Med Sci. 1967;254(3):347-356.
doi pubmed - Pekanan P, Supromajak W, Suchato C, Suwanvilai C, Nirapathapongporn S. Gastroduodenal intussusception: a case report and literature review. J Med Assoc Thai. 1988;71(3):167-169.
pubmed - Govednik C, Cover J, Regner JL. Preventing retrograde jejunoduodenogastric intussusception as a complication of a long-term indwelling gastrostomy tube. Proc (Bayl Univ Med Cent). 2015;28(1):34-37.
doi pubmed pmc - Akashi T, Takahashi S, Yodoe K, Yamada M, Yoshimura D, Ochiai T, Tsuchida O, et al. [Gastric outlet obstruction caused by gastrostomy tube balloon in 3 cases]. Nihon Shokakibyo Gakkai Zasshi. 2012;109(4):600-605.
pubmed - Alomari M, Alomari A, Hitawala A, Khazaaleh S, Al Momani LA. Anterograde gastroduodenal intussusception: a rare but lethal complication of percutaneous endoscopic gastrostomy tube placement. Cureus. 2019;11(3):e4347.
doi pubmed pmc - Gauderer MW, Ponsky JL, Izant RJ, Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
doi pubmed - Mitchell SL, Tetroe JM. Survival after percutaneous endoscopic gastrostomy placement in older persons. J Gerontol A Biol Sci Med Sci. 2000;55(12):M735-739.
doi pubmed - Duszak R, Jr., Mabry MR. National trends in gastrointestinal access procedures: an analysis of Medicare services provided by radiologists and other specialists. J Vasc Interv Radiol. 2003;14(8):1031-1036.
doi pubmed - Singhal M, Kang M, Narayanan S, Gupta R, Wig JD, Bal A. Duodenoduodenal intussusception. J Gastrointest Surg. 2009;13(2):386-388.
doi pubmed - Loo GH, Mohamad Abu Zeid WM, Lim SL, Ismail AM. Rare presentation of idiopathic duodenoduodenal intussusception. Ann R Coll Surg Engl. 2017;99(6):e188-e190.
doi pubmed pmc - Limi L, Liew NC, Badrul RH, Faisal MJ, Daniel YP. Duodenal intussusception of Brunner's gland adenoma mimicking a pancreatic tumour. Med J Malaysia. 2010;65(4):311-312.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


