| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 6, June 2023, pages 191-195
Sarcomatoid Carcinoma of Orbit in a Patient With Xeroderma Pigmentosum
Prakash Banjadea , Asmita Itanib, Kamal Kandela, Shradha Acharyab, Munish Sharmac, f, Gulshan Bahadur Shresthad, Salim Suranie
aDepartment of Medicine, Manipal College of Medical Sciences, Pokhara, Nepal
bDepartment of Medicine, Institute of Medicine, Kathmandu, Nepal
cDivision of Pulmonary, Critical Care and Sleep Medicine, Baylor Scott and White, Temple, TX, USA
dDepartment of Ophthalmology, Maharajgunj Medical Campus, Institute of Medicine and B.P. Koirala Lions Centre for Ophthalmic Studies, Kathmandu, Nepal
ePulmonary and Critical Care, Texas A&M University, Corpus Christi, TX, USA
fCorresponding Author: Munish Sharma, Division of Pulmonary, Critical Care and Sleep Medicine, Baylor Scott and White, Temple, TX, USA
Manuscript submitted May 3, 2023, accepted May 23, 2023, published online June 29, 2023
Short title: Sarcomatoid Carcinoma of Orbit in a XP Patient
doi: https://doi.org/10.14740/jmc4110
| Abstract | ▴Top |
Spindle cell carcinoma (SpCC), also referred to as sarcomatoid carcinoma, makes up less than 3% of all head and neck squamous cell carcinomas (SCCs). It is an uncommon and unusual biphasic malignant tumor primarily affecting the upper aero-digestive tract. SpCC consists of spindled or pleomorphic tumor cells. Mostly, these tumors are seen in the fifth or sixth decades of life and are strongly associated with smoking and alcohol. We hereby report an infrequently encountered case of SpCC in a patient with xeroderma pigmentosum (XP), who was young, nonsmoker, and did not consume alcohol. The mass arose from the right orbit and involved the entire right face. The postoperative histopathological report showed SpCC. Surgical excision of the mass was performed. We aimed to add to the prevailing literature by reporting this case.
Keywords: Spindle cell carcinoma; Xeroderma pigmentosum; Head and neck cancer; Squamous cell carcinoma
| Introduction | ▴Top |
Xeroderma pigmentosum (XP) is a rare autosomal recessive genetic disease in which mutations in any of the eight genes (XP, XPA through XPG) lead to defective DNA repair, predisposing the individual to develop various cutaneous and ocular malignancies in the ultraviolet (UV)-exposed areas [1-3]. The incidence of XP in Nepal is higher than in Western countries, along with the predominance of XP-C mutation [4]. In XP patients without rigorous photoprotection, squamous cell carcinoma (SCC), basal cell carcinoma (BCC), and melanoma are common orbital tumors that primarily affect eyelids, cornea, and conjunctiva [3, 5].
Sarcomatoid (spindle cell) carcinomas, rare SCC variants, contain squamous epithelial and sarcomatous spindle cell components [6, 7]. They account for less than 3% of all SCCs of the head and neck region and are commonly reported in the larynx [6]. Significant morphological and immunohistochemical overlaps between sarcomatoid carcinoma and other spindle cell tumors make diagnosis challenging. Like SCC, the outcome of sarcomatoid carcinoma on the head and neck region depends on location and the clinical stage [7].
| Case Report | ▴Top |
Investigations
A 26-year-old man with a known case of XP presented to the Emergency Department of our hospital with a large mass over the right orbital region and right face. The mass in the right eye first appeared 4 months prior to this presentation and gradually increased in size. Another ophthalmology facility performed an excisional biopsy. About 15 days following the biopsy, the mass began to overgrow. The mass was painful, with foul-smelling whitish-yellow discharge and occasional bleeding. According to the patient, he had difficulty bearing his smell and eating. According to his mother, the patient’s history dates back to when he was 2 years old. He started having skin changes starting from the face, which the mother described as “dark spots” in the absence of an official clinical evaluation and established diagnosis. Subsequently, he developed a mass in the right eye, for which he was seen in an outside hospital and diagnosed as XP with a neoplastic mass. The mass was excised twice at around 4 years of age. In the absence of electronic medical record system, we could not obtain paper documentation regarding the type of neoplasia diagnosis and treatment received during that time. The second excision was done in our hospital. In 2003, the patient developed a whitish patch in the right eye; the biopsy report was negative for malignancy. The patient was prescribed mitomycin for 21 days in 2013, and in 2017 he underwent keratoprosthesis at an outside hospital. The patient was a nonsmoker, did not consume alcohol, had low socioeconomic status, and had no significant family history.
On physical examination, the patient was thin built (body mass index (BMI) = 17.8 kg/m2), well-oriented to time, place, and person, and had normal vital parameters. Skin revealed hyperpigmented patches all over the body that resembled XP. The abdomen was flat and non-tender, with no organomegaly. The chest examination was normal. Cardiac rate and rhythm were normal. No gross neurological deficits were noted.
Examination of the face revealed a large, round mass with an irregular surface. Foul-smelling cheesy, yellowish-whitish exudate with scabs and bleeding points were noted on the surface of the mass. The size of the mass was about 15 × 12 × 10 cm, covering almost the entire right face. On palpation, the mass was firm and bled on touch. Examination of the left side of the face revealed an upper eyelid mass of size 2 × 2 × 2 cm and a mass in the left temple of size 4 × 3 × 4 cm. Both masses were irregular, with denuded skin and bleeding points attached to underlying skin and firm to touch (Fig. 1).
 Click for large image | Figure 1. Large mass with irregular surface involving the right face and left upper lid mass along with skin freckles of xeroderma pigmentosum (black arrow). |
Diagnosis
The laboratory investigation was remarkable for low hemoglobin (7.8 g/dL). Magnetic resonance imaging (MRI) of the head and neck region was done, which showed a large heterogenous fungating mass of dimension 12.3 × 8.9 × 8 cm in the right orbit, displacing the entire orbital content. Posteriorly the mass reached the superior orbital fissure and the optic canal. However, there was no intracranial extension. Erosion of medial and inferior orbital walls with mass extension into the right ethmoid and maxillary sinus was noted in MRI (Fig. 2).
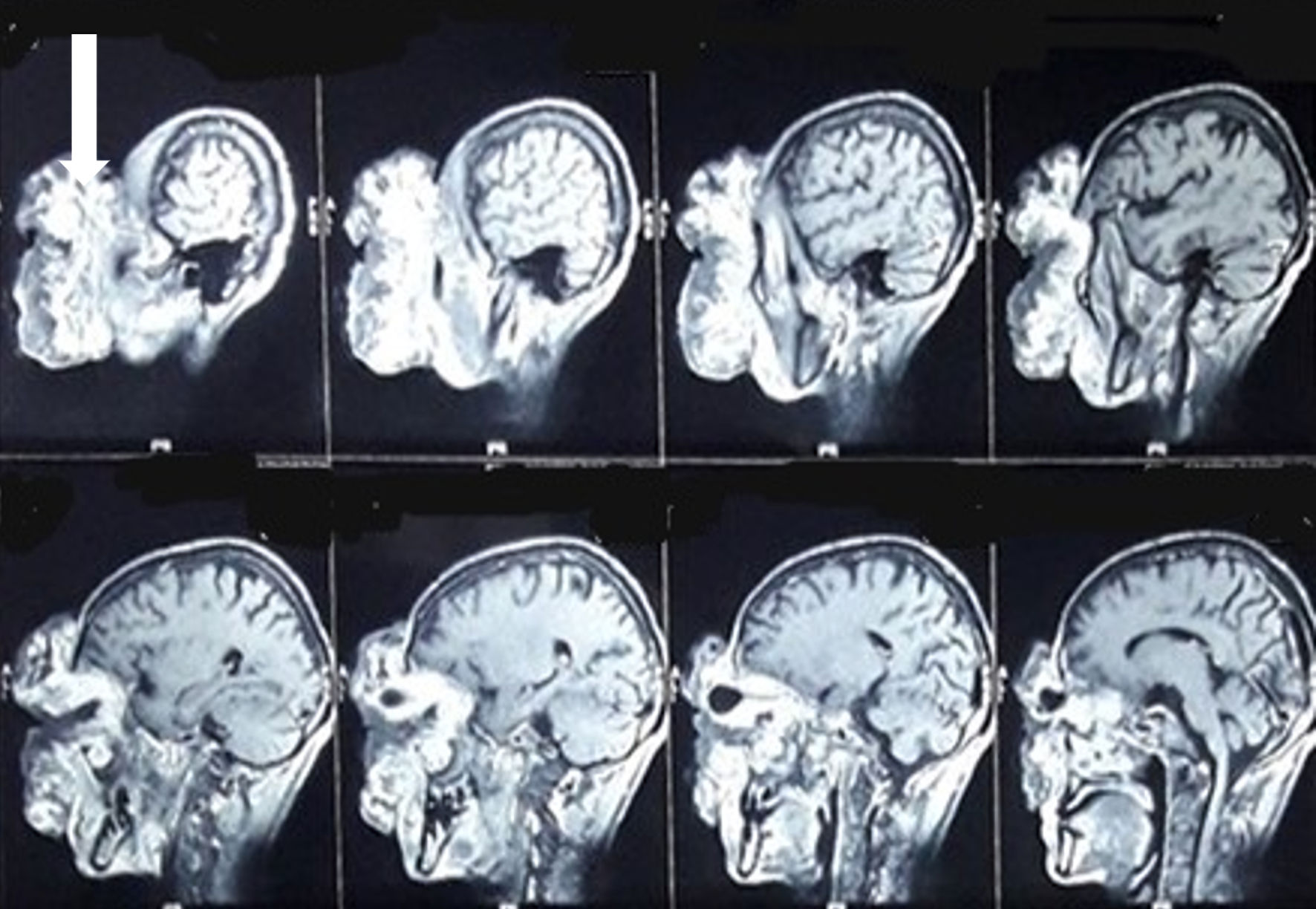 Click for large image | Figure 2. MRI head and neck. White arrow shows the large heterogenous fungating mass in the right orbit, displacing the entire orbital content. MRI: magnetic resonance imaging. |
Treatment
Three units of whole blood and one unit of packed red blood cell transfusion were given preoperatively over a period of 12 days. The patient then underwent debulking surgery of the right facial, right maxillary sinus, and right nasal cavity mass, with right orbital exenteration, was done (Figs. 3, 4). The left temporal and upper eyelid mass were excised. The uninvolved skin margin of 2 mm was included in both resections. The samples from six sites (right: orbital, cheek, nasal cavity, maxillary antrum; left: upper eyelid and temporal region) were sent for histopathological examination. Postoperative management was done with intravenous antibiotics (ceftriaxone, metronidazole) and analgesics (ibuprofen). On the fifth postoperative day, the compressive bandage was removed, and the patient was discharged on oral ampicillin plus cloxacillin and topical ciprofloxacin.
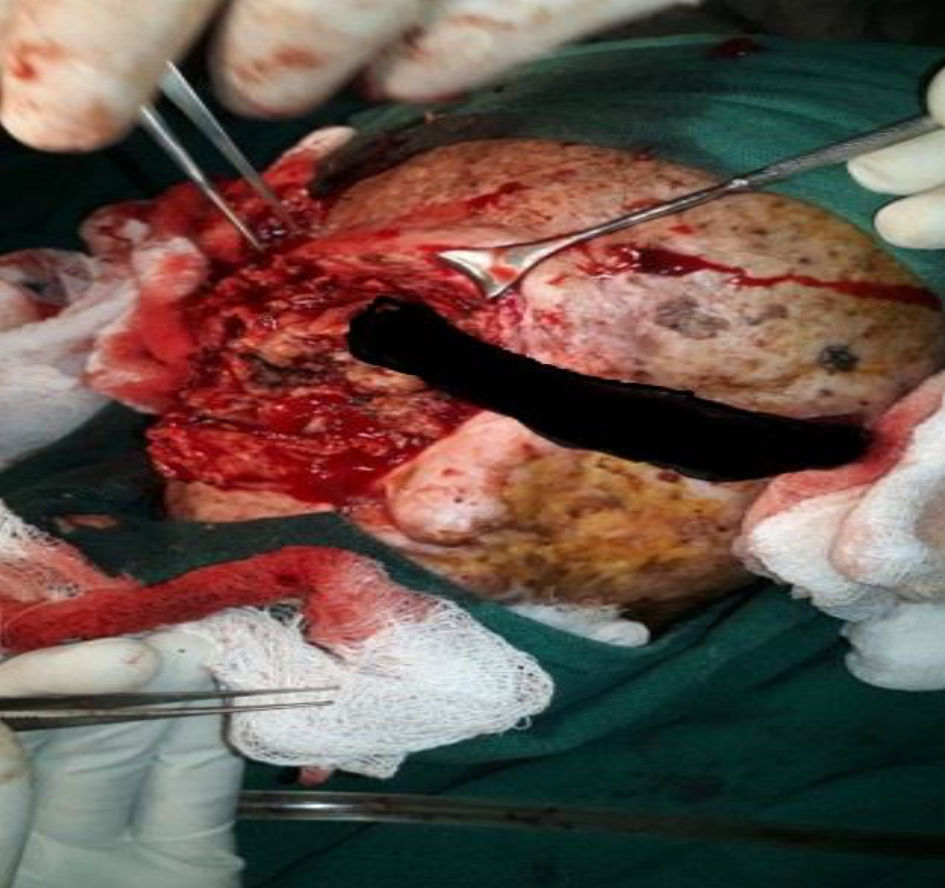 Click for large image | Figure 3. Excision of right-sided mass in pieces (image corrected - decreased stretching). |
 Click for large image | Figure 4. Final picture after excision of both right- and left-sided masses. |
A histopathological examination report showed that the mass on the right side consisted of tumor cells arranged in an arborizing vascular pattern, fascicles, and bundles, had a moderate amount of cytoplasm, epithelioid to spindled nuclei, vesicular chromatin and prominent nucleoli. Hyperplastic low-differentiated stratified squamous epithelium with moderate to marked pleomorphism was seen. Numerous mitotic figures constituting 10/high-power field (HPF) in mitotically active areas with large areas of necrosis and hemorrhage were seen. Poorly differentiated spindle-shaped cells were noted. On immunohistochemistry, tumor cells were focally positive for CD34. The diagnosis of malignant spindle cell neoplasm, cutaneous origin was made. The left-sided masses were found to be SCC. The patient was referred to a cancer center for advice regarding chemotherapy/radiotherapy.
Follow-up and outcomes
A follow-up 1 month later showed no recurrence/new mass. The patient’s hemodynamic status was stable. He was safely discharged home with a follow-up in 3 months.
| Discussion | ▴Top |
XP is a rare genetic disease caused by defective DNA repair. It shows an autosomal recessive pattern with a worldwide prevalence of 1:250,000. It is characterized by extreme photosensitivity and an increased risk of skin cancers. People with XP have a 10,000-fold higher risk of developing non-melanoma skin cancer and a 2,000-fold higher risk of developing melanoma before age 20 [8]. In addition to this, people with XP have an increased risk of internal neoplasms and ocular abnormalities.
SCC appears in various forms. sarcomatoid (spindle cell carcinoma (SpCC)) is a rare variant of SCC. In the head and neck region, sarcomatoid carcinomas make up about 1% of all SCCs [9]. Viswanathan et al studied 103 confirmed cases of sarcomatoid (SpCC). The ratio of men to women was 3.7:1. The most common site was the oral cavity (63.1%), followed by the larynx (17.5%), oropharynx/hypopharynx (10.7%), maxilla (5.8%), and metastatic nodes (1.9%). However, our patient had SpCC of orbit, which is a very rare case [7]. Oral-pharyngeal SCC most commonly occurs in the fifth and sixth decades and is strongly associated with smoking and alcohol consumption. On the other hand, cutaneous SCC is related to extreme photosensitivity to UV-rays, as in our patient, who was young, a nonsmoker, and did not consume alcohol.
Histopathologically speaking, sarcomatoid carcinoma is a hybrid of sarcoma and carcinoma. It consists of differential mesenchymal tissues. Clinically, most tumors are T3 or T4 at the time of presentation, which means they frequently present at locally advanced stages [10]. Biopsy and histopathological examination are the diagnostic modalities of choice. Studies suggest various immunohistochemical staining is helpful for diagnosis. Literature suggests that, if needed, sarcomatoid (spindle cell) carcinoma can be managed with wide local excision and chemotherapy/radiotherapy. We performed an excision of the mass with 2 mm uninvolved skin margin [11].
Conclusions
Sarcomatoid (spindle cell) carcinoma is an uncommon but aggressive malignancy with an unfavorable prognosis. Patients typically arrive at advanced stages. Due to overlapping histological characteristics with other spindle cell tumors, the diagnosis is difficult. Though commonly encountered in patients in their fifth and sixth decades of life and history of alcohol and smoking, it can be seen in younger patients without such a predisposing history. Our patient had XP and did not have rigorous photoprotection. There are no established treatment methods in the literature. According to our experience, the surgical removal of such a tumor should be followed by radiotherapy or chemotherapy, if necessary, for complete treatment and to prevent a recurrence.
Learning points
SpCC is a rare entity, with only a few cases reported in the literature. It mainly occurs in an older age group with significant smoking and alcohol history. However, it can occur in younger individuals as well. Most patients present at an advanced stage, so management is often challenging. Surgical excision and histopathological examination should be performed.
Acknowledgments
We would like to thank Dr. Sumit Pandey, lecturer, Department of Ophthalmology, College of Medical Sciences, Nepal, for reviewing and correcting the manuscript.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
The patient’s written informed consent was obtained for the publication of this case report and associated images.
Author Contributions
Prakash Banjade and Kamal Kandel: manuscript writing. Asmita Itani and Shradha Acharya: data collection. Munish Sharma and Salim Surani: review, final corrections and approval of the manuscript. Gulshan Bahadur Shrestha: supervising article writing and the lead surgeon of the case.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Kalamkar C, Radke N, Mukherjee A, Radke S. Xeroderma pigmentosum with bilateral ocular surface squamous neoplasia and review of the literature. BMJ Case Rep. 2016;2016:bcr2016215364
doi pubmed pmc - Lehmann AR, McGibbon D, Stefanini M. Xeroderma pigmentosum. Orphanet J Rare Dis. 2011;6:70.
doi pubmed pmc - Yuksel D, Kosker M, Reddy JC, Celik T. Management of cataracts and oculo-cutaneous malignancy in xeroderma pigmentosum. Semin Ophthalmol. 2013;28(2):55-57.
doi pubmed - Espi P, Parajuli S, Benfodda M, Lebre AS, Paudel U, Grange A, Grybek V, et al. Clinical and genetic characteristics of xeroderma pigmentosum in Nepal. J Eur Acad Dermatol Venereol. 2018;32(5):832-839.
doi pubmed - Ramkumar HL, Brooks BP, Cao X, Tamura D, Digiovanna JJ, Kraemer KH, Chan CC. Ophthalmic manifestations and histopathology of xeroderma pigmentosum: two clinicopathological cases and a review of the literature. Surv Ophthalmol. 2011;56(4):348-361.
doi pubmed pmc - Altinay S, Altinok A, Altinok Sut P, Taskin U, Bilici A. Spindle cell carcinoma (sarcomatoid carcinoma) of maxillary sinus and nasal cavity with orbital involvement: a rare case report and brief review of literature. Dent Oral Craniofac Res. 2018;4(5):1-4.
- Viswanathan S, Rahman K, Pallavi S, Sachin J, Patil A, Chaturvedi P, D'Cruz A, et al. Sarcomatoid (spindle cell) carcinoma of the head and neck mucosal region: a clinicopathologic review of 103 cases from a tertiary referral cancer centre. Head Neck Pathol. 2010;4(4):265-275.
doi pubmed pmc - Bradford PT, Goldstein AM, Tamura D, Khan SG, Ueda T, Boyle J, Oh KS, et al. Cancer and neurologic degeneration in xeroderma pigmentosum: long term follow-up characterises the role of DNA repair. J Med Genet. 2011;48(3):168-176.
doi pubmed pmc - Thompson LD, Wieneke JA, Miettinen M, Heffner DK. Spindle cell (sarcomatoid) carcinomas of the larynx: a clinicopathologic study of 187 cases. Am J Surg Pathol. 2002;26(2):153-170.
doi pubmed - Howard SN, Bond WR, Hong IS, Foss RD. Right maxillary sinus sarcomatoid carcinoma (sarcomatoid/spindle cell carcinoma). Otolaryngol Head Neck Surg. 2007;137(2):355-357.
doi pubmed - Mistry P, Mittal A, Nagpal T. Spindle cell carcinoma of nasal cavity- a case report. J Clin Diagn Res. 2016;10(4):MD01-02.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


