| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 9-10, October 2023, pages 344-349
Improvement in Tubulointerstitial Nephritis With Glucocorticoid Therapy in an Anorexia Nervosa Patient
Kenta Torigoea, d , Yuki Yoshidaa, Ryosuke Sakamotoa, Shinichi Abea, Kumiko Mutaa, Hideyuki Araib, Hiroshi Mukaec, Tomoya Nishinoa
aDepartment of Nephrology, Nagasaki University Hospital, Nagasaki City, Nagasaki 852-8501, Japan
bKusumoto Naika Clinic, Omura City, Nagasaki 856-0817, Japan
cDepartment of Respiratory Medicine, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki City, Nagasaki 852-8501, Japan
dCorresponding Author: Kenta Torigoe, Department of Nephrology, Nagasaki University Hospital, Nagasaki City, Nagasaki 852-8501, Japan
Manuscript submitted August 29, 2023, accepted October 10, 2023, published online October 13, 2023
Short title: TIN in an Anorexia Nervosa Patient
doi: https://doi.org/10.14740/jmc4152
| Abstract | ▴Top |
Anorexia nervosa is a psychiatric disorder that is often diagnosed in adolescents and young adults. Renal-related complications of anorexia nervosa include abnormal water metabolism, electrolyte abnormalities, and nephrocalcinosis, which may lead to irreversible renal damage. Furthermore, tubulointerstitial nephritis has been reported as a renal pathological feature of anorexia nervosa. Immunosuppressive therapy, such as with glucocorticoids, has been recommended for idiopathic interstitial nephritis treatment; however, the effectiveness of immunosuppressive therapy for interstitial nephritis in patients with anorexia nervosa remains unestablished. Here, we report a case of interstitial nephritis in a patient with anorexia nervosa whose renal function was successfully improved with glucocorticoid therapy. The patient was a 38-year-old woman who was referred for renal dysfunction (estimated glomerular filtration rate: 7.6 mL/min/1.73 m2). She had anorexia nervosa and repeated episodes of vomiting. Hypokalemia (K: 2.1 mEq/L) and metabolic alkalosis (HCO3-: 54.2 mEq/L) were observed. Fluid therapy and potassium supplementation did not improve renal function; therefore, a percutaneous renal biopsy was performed. The renal pathology results revealed interstitial fibrosis, inflammatory cell infiltration in the interstitium, and tubulitis, suggesting a diagnosis of tubulointerstitial nephritis. Glucocorticoid therapy improved the patient’s renal function to an estimated glomerular filtration rate of 19.91 mL/min/1.73 m2, and the renal function remained stable thereafter. This case suggests that glucocorticoid therapy may be considered for the treatment of interstitial nephritis in patients with anorexia.
Keywords: Acute tubulointerstitial nephritis; Anorexia nervosa; Renal insufficiency
| Introduction | ▴Top |
Anorexia nervosa is a psychiatric disorder that is often diagnosed in adolescents and young adults. It is associated with high mortality owing to decreased food intake, weight loss, and metabolic abnormalities [1]. Renal-related complications of anorexia nervosa are abnormal water metabolism, electrolyte abnormalities, and nephrocalcinosis, which may lead to irreversible renal damage [2].
Furthermore, tubulointerstitial fibrosis and tubulointerstitial nephritis have been reported as renal pathological features of anorexia nervosa [3, 4]. Immunosuppressive therapy, such as glucocorticoids, has been recommended for the treatment of idiopathic interstitial nephritis. However, the effectiveness of immunosuppressive therapy for interstitial nephritis in patients with anorexia nervosa remains unestablished, and a previous report has shown that such therapy is ineffective [4]. Herein, we report a case of a patient with anorexia nervosa with tubulointerstitial nephritis whose renal function was successfully improved with glucocorticoid therapy.
| Case Report | ▴Top |
Investigations
A 38-year-old woman was referred to our hospital for renal dysfunction; for more than 20 years, the patient had decreased food intake and repeated episodes of vomiting, with persistent psychological stress. She visited the clinic once regarding the repeated episodes of vomiting but was not followed up regularly; thus, her previous renal function was unknown. She was referred to our hospital because a health examination performed at her request revealed renal dysfunction with a creatinine (Cr) level of 5.67 mg/dL and estimated glomerular filtration rate (eGFR) of 7.6 mL/min/1.73 m2. Other than episodes of vomiting, there were no other specific findings in her medical history, including use of diuretics or laxatives. At the time of referral, the patient was underweight, with a height of 156 cm, weight of 33.8 kg, and body mass index (BMI) of 13.89 kg/m2. Her vital signs were as follows: temperature 36.8 °C; pulse 76 beats/min; blood pressure 80/53 mm Hg; and oxygen saturation (SpO2) 97% (room air). Her daily urine volume was 1,100 mL, and no notable findings other than body weight loss were observed.
Diagnosis
Blood tests showed renal dysfunction, with a Cr of 5.01 mg/dL, eGFR of 8.72 mL/min/1.73 m2, and hypokalemia (K: 2.1 mEq/L). A venous blood gas test showed metabolic alkalosis, with a pH of 7.479, partial pressure of carbon dioxide (pCO2) of 20.8 mm Hg, and HCO3- of 54.2 mEq/L. Immunological examination revealed antinuclear antibodies 160-fold and hypocomplementemia; however, autoantibodies such as double-stranded deoxyribonucleic acid (ds-DNA), Sjogren’s syndrome antigen A (SS-A), and Sjogren’s syndrome antigen B (SS-B) were negative. A urinary test showed a urinary β2 microglobulin level of 74105.7 µg/L, which suggested a tubulointerstitial injury (Table 1). Simple abdominal computed tomography showed no evidence of renal atrophy or kidney stones (Fig. 1). In addition to repeated vomiting and low body weight, the patient feared weight gain and amenorrhea; thus, she met the diagnostic criteria for anorexia nervosa [2]. The patient was then admitted to our department for further evaluation of renal dysfunction (Fig. 2).
 Click to view | Table 1. Laboratory Findings |
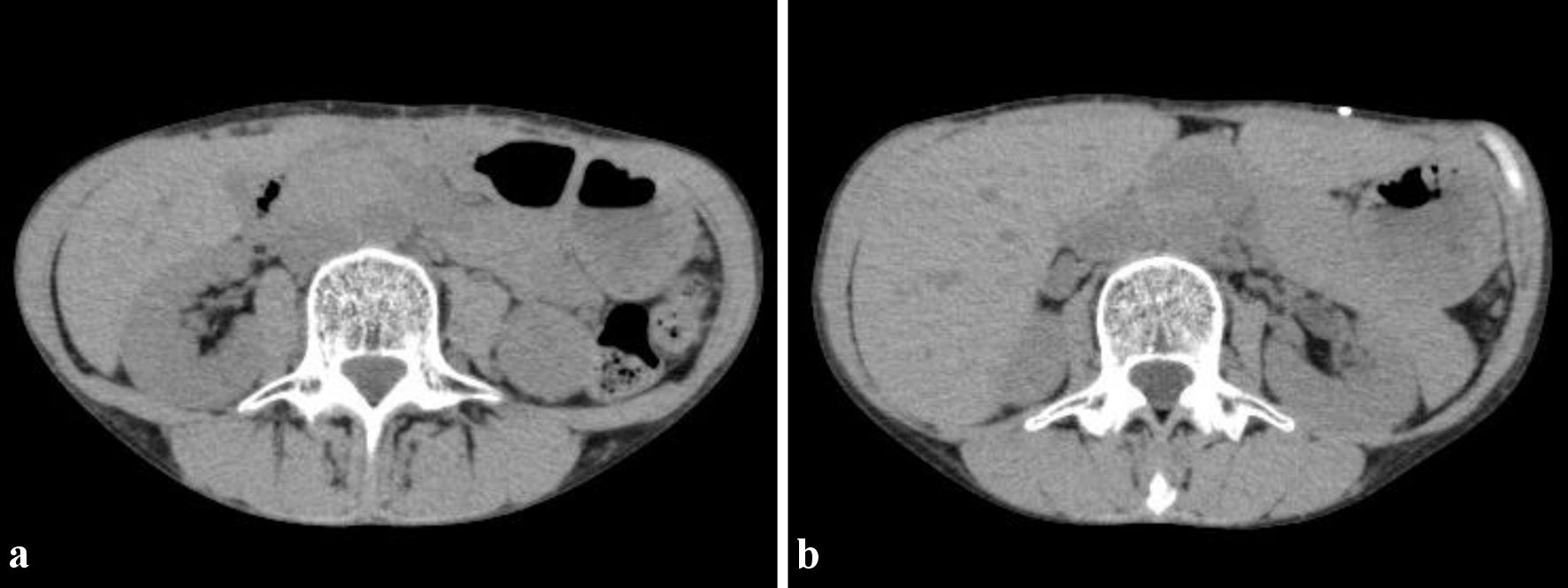 Click for large image | Figure 1. Computed tomography imaging findings. There is no renal atrophy and no kidney stones. (a) Right kidney. (b) Left kidney. |
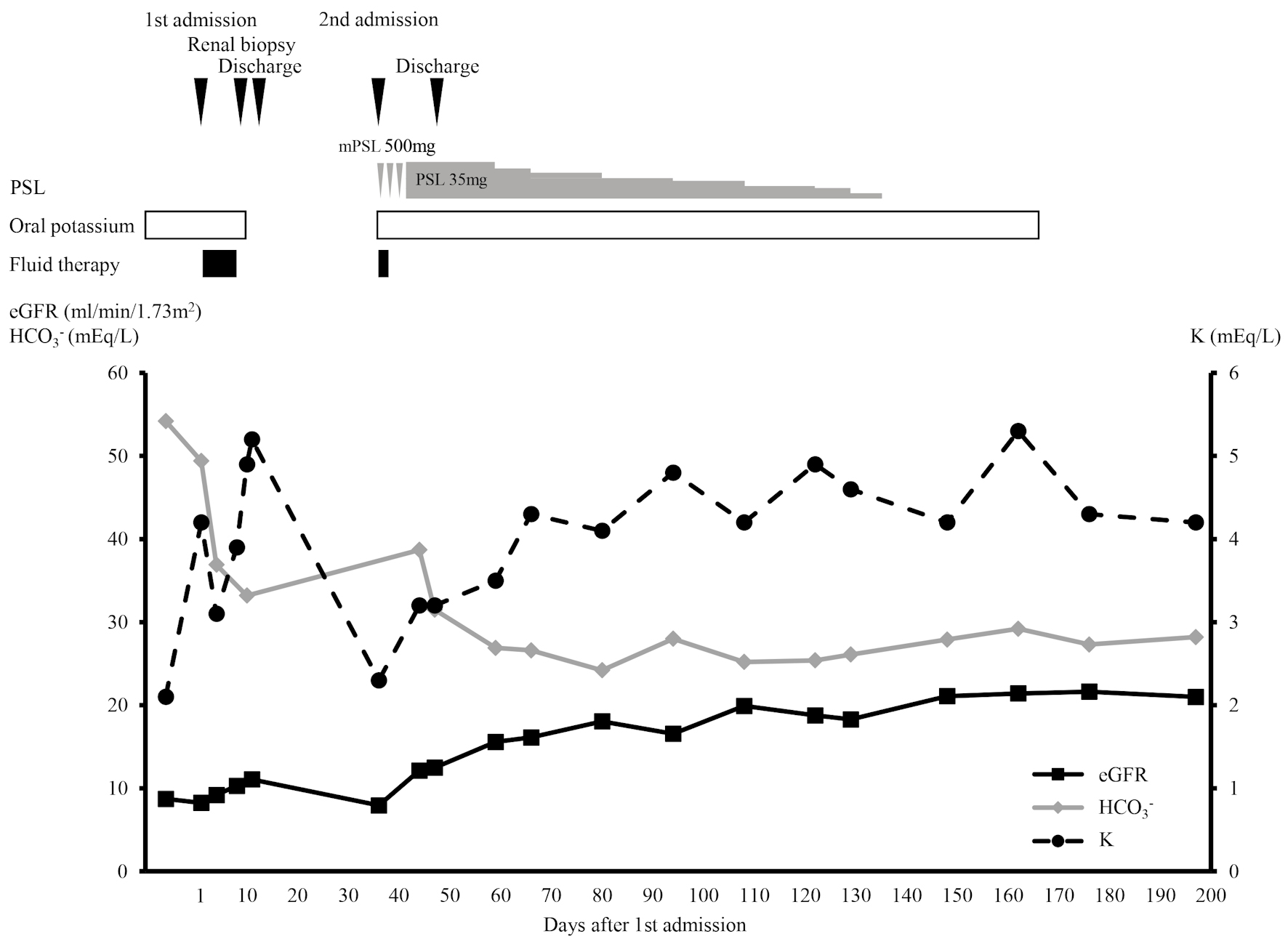 Click for large image | Figure 2. The clinical course of the patient. eGFR: estimated glomerular filtration rate, HCO3-: bicarbonate, K: potassium, mPSL: methylprednisolone, PSL: prednisolone. |
Volume depletion due to vomiting was suspected as the cause of the renal dysfunction; thus, fluid therapy was initiated, resulting in increased body weight to 36 kg. Potassium supplementation was also initiated for hypokalemia, leading to improvement in hypokalemia and alkalosis; however, the renal dysfunction persisted. Therefore, a percutaneous renal biopsy was performed on day 9 of admission. Light microscopy revealed tubulointerstitial fibrosis. In contrast, inflammatory cells had infiltrated the interstitium, and tubulitis was observed, suggesting interstitial nephritis. The glomerulus showed no cellular lesions or global sclerosis (Fig. 3). Immunofluorescence was negative for immunoglobulin (Ig)A, IgG, IgM, complement component 3 (C3), and C1q. After renal biopsy, the patient was discharged from our hospital and re-admitted to our department on day 36 of the first admission for the treatment of interstitial nephritis.
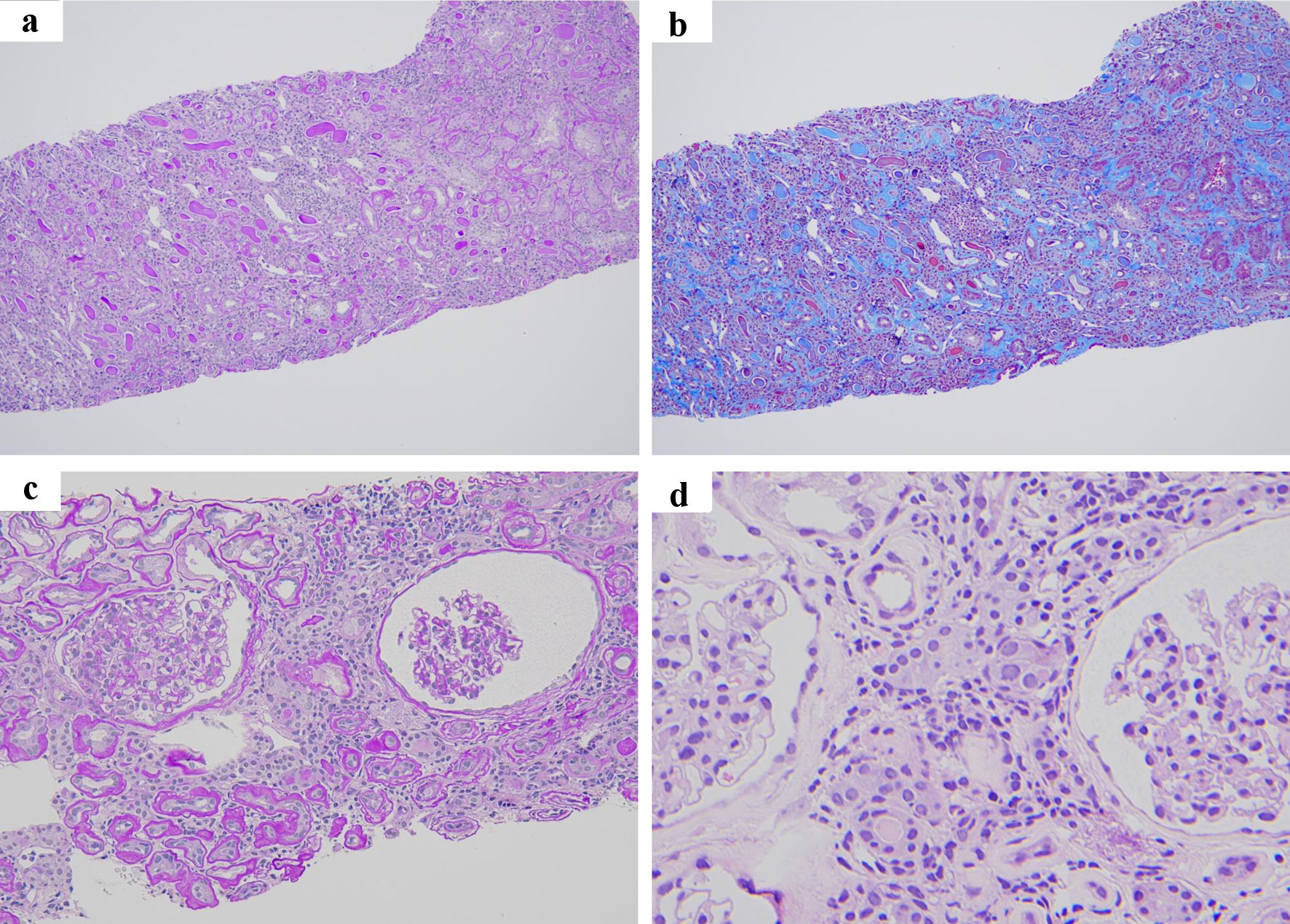 Click for large image | Figure 3. Renal pathology findings. (a, b) The tubulointerstitium showed diffuse inflammatory cell infiltration and fibrocellular change. (a) Periodic acid-Schiff staining × 100. (b) Masson’s trichrome stain × 100. (c) The glomerulus showed no cellular lesion or global sclerosis (periodic acid-Schiff staining × 200). (d) Inflammatory cells in the tubulointerstitium were mainly lymphocytes and plasma cells, and tubulitis was observed (hematoxylin and eosin stain × 400). |
Treatment
After admission, methylprednisolone 500 mg/day and prednisolone (PSL) 35 mg/day were initiated. Renal function gradually improved after treatment, and the patient was discharged on day 48 of the first admission, and glucocorticoid therapy was continued on an outpatient basis.
Follow-up and outcomes
On day 108 of the first admission, her eGFR and Cr improved to 19.91 mL/min/1.73 m2 and 2.34 mg/dL respectively. PSL treatment was administered for 100 days and terminated on day 136 of the first admission, and her renal function remained stable. At the time of diagnosis, investigations for the underlying cause of interstitial nephritis yielded no obvious results including drug history. Uveitis was diagnosed by an ophthalmologist during a routine follow-up of the side effects of glucocorticoids. The combination of interstitial nephritis and uveitis indicated tubulointerstitial nephritis and uveitis (TINU) syndrome. The patient’s mental status was regularly monitored in our department. After the patient was referred to our department, the frequency of vomiting gradually decreased, and potassium supplements and fluid therapy were discontinued. During the outpatient follow-up, her weight was maintained at approximately 34 kg, and she was not obviously dehydrated. Regarding uveitis, no active lesions were present at the time of diagnosis, and no exacerbations were observed in subsequent follow-up.
| Discussion | ▴Top |
This case involved a patient with anorexia nervosa and interstitial nephritis. A previous report has shown that glucocorticoid therapy is ineffective for tubulointerstitial nephritis complicated by anorexia nervosa [4]. However, in this case, renal function improved with glucocorticoid therapy. Our case suggests that immunosuppressive therapy may be a treatment option for interstitial nephritis complicated by anorexia nervosa.
The causes of renal dysfunction in anorexia nervosa vary, and fluid volume depletion and electrolyte abnormalities are important causes [2, 5]. Volume depletion is caused by repeated vomiting and abuse of diuretics and laxatives, leading to chronic renal ischemia and renal dysfunction [4]. In this case, the patient had repeated episodes of vomiting before referral to our hospital. Therefore, we considered the possibility of renal dysfunction due to volume depletion and initiated fluid infusion therapy; however, the renal function did not improve.
Chronic hypokalemia due to vomiting, diuretics, and laxatives is an important cause of renal dysfunction in anorexia nervosa [6]. Persistent hypokalemia causes vacuolar degeneration in proximal tubular cells [7-9]. If hypokalemia persists for a short period, the effects on tubular cells are reversible. However, if prolonged, it causes irreversible changes, such as interstitial fibrosis, tubular atrophy, and medullary cyst formation [10]. Tubulointerstitial nephritis has also been reported as a complication of persistent hypokalemia in patients with anorexia nervosa [4, 11, 12]. The mechanism of tubulointerstitial nephritis in hypokalemia has not been established; however, the production of monocyte chemotactic protein 1 (MCP-1), a mediator of macrophage infiltration, is reportedly increased in the kidneys of rats with hypokalemia. In addition, hypokalemic rats showed an increased expression of tumor necrosis factor-α (TNF-α) and infiltration of macrophages in the interstitium [13]. Therefore, inflammatory cytokines, such as MCP-1 and TNF-α, may induce tubulointerstitial nephritis in patients with anorexia nervosa with hypokalemia. However, a previous case showed that glucocorticoid therapy was ineffective for anorexia-associated tubulointerstitial nephritis [4].
In this case, the patient had hypokalemia, and treatment with potassium supplementation was initiated; however, renal function did not improve, and a renal biopsy was performed to investigate the underlying cause. Renal pathology showed interstitial fibrosis, tubular atrophy, and infiltration of inflammatory cells in the interstitium, suggesting tubulointerstitial nephritis. Unlike in previous reports, the patient’s renal function improved after glucocorticoid therapy.
Although glucocorticoid therapy may have been effective for the treatment of anorexia-induced interstitial nephritis in this case, we could not exclude the possibility that it may have also been effective for treating TINU syndrome. In this case, we searched for autoimmune diseases and other causes of interstitial nephritis when the patient was diagnosed with interstitial nephritis; however, no cause was found. Drugs are usually the most common cause of interstitial nephritis, accounting for > 75% of cases [14]. Furthermore, some drugs (diuretics, laxatives, etc.) are also important causes of hypokalemia [15]. Therefore, in this case, drug-related pathogenesis should be the first differential diagnosis; however, the possibility that the interstitial nephritis and hypokalemia were drug-related was ruled out because the patient had no history of the suspected drugs use. The patient developed uveitis 5 months after glucocorticoid therapy was initiated, suggesting the possibility of TINU syndrome. Uveitis often develops after interstitial nephritis in TINU syndrome, which was observed in the present case [16]. Usually, interstitial nephritis, unrelated to anorexia nervosa, is complicated by hypokalemia and renal tubular acidosis [17]. Although hypokalemia is also present in anorexia, metabolic alkalosis occurs because of vomiting. Therefore, interstitial nephritis not caused by anorexia nervosa should be suspected when metabolic acidosis is a complication. In this case, the patient had hypokalemia and metabolic alkalosis, which were attributed to be acid-base imbalance abnormalities associated with vomiting. In addition, TINU syndrome requires the exclusion of other causes of interstitial nephritis. However, anorexia nervosa may have caused interstitial nephritis in this case [18]. Furthermore, glucocorticoids did not completely restore renal function in this patient. We speculate that chronic renal ischemia and chronic renal tubular disorder due to low potassium associated with anorexia nervosa may have contributed to this.
Usually, renal biopsies are not performed in patients with anorexia because repeated volume depletion and electrolyte abnormalities have been clinically determined to cause renal dysfunction. However, when the renal dysfunction does not improve after volume and electrolyte correction, interstitial nephritis may be a differential diagnosis, and a renal biopsy is indicated.
Another reason why the renal function remained stable in this patient was the stabilization of serum potassium levels. After the patient was referred to our hospital, the episodes of vomiting decreased, and the serum potassium levels remained within the normal range. Hypokalemia is often intractable due to repeated vomiting and abuse of laxatives and diuretics. However, the patient’s mental status did not deteriorate after glucocorticoid therapy was initiated, and she remained stable.
In summary, a patient with anorexia with severe renal dysfunction was diagnosed with interstitial nephritis in this case. Unlike in previous studies, the renal function improved with glucocorticoid therapy. Although renal biopsies are rarely performed in patients with anorexia, they are useful in cases of unexplained renal dysfunction. Glucocorticoid therapy for the treatment of interstitial nephritis in patients with anorexia may improve renal function; however, its efficacy has not yet been established.
Learning points
Interstitial nephritis is a differential diagnosis for renal dysfunction in patients with anorexia. Our findings suggest that glucocorticoid therapy may be considered for the treatment of interstitial nephritis in patients with anorexia; however, further investigation of its efficacy should be a priority in future studies on the treatment of interstitial nephritis in anorexia nervosa.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
All authors participated in patient care. Kenta Torigoe was responsible for drafting the manuscript. All authors read and approved the final version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Resmark G, Herpertz S, Herpertz-Dahlmann B, Zeeck A. Treatment of anorexia nervosa-new evidence-based guidelines. J Clin Med. 2019;8(2):153.
doi pubmed pmc - Bouquegneau A, Dubois BE, Krzesinski JM, Delanaye P. Anorexia nervosa and the kidney. Am J Kidney Dis. 2012;60(2):299-307.
doi pubmed - Choi JW, Kwon SK, Kim SM, Cho H, Lee HC, Kim HY. Interstitial nephritis caused by anorexia nervosa in young male; A case report and literature review. Electrolyte Blood Press. 2018;16(1):15-17.
doi pubmed pmc - Marumoto H, Sasaki T, Tsuboi N, Ito T, Ishikawa M, Ogura M, Ikeda M, et al. Kidney disease associated with anorexia nervosa: a case series with kidney biopsies. Kidney Med. 2020;2(4):418-424.
doi pubmed pmc - Puckett L. Renal and electrolyte complications in eating disorders: a comprehensive review. J Eat Disord. 2023;11(1):26.
doi pubmed pmc - Takakura S, Nozaki T, Nomura Y, Koreeda C, Urabe H, Kawai K, Takii M, et al. Factors related to renal dysfunction in patients with anorexia nervosa. Eat Weight Disord. 2006;11(2):73-77.
doi pubmed - Yalamanchili HB, Calp-Inal S, Zhou XJ, Choudhury D. Hypokalemic nephropathy. Kidney Int Rep. 2018;3(6):1482-1488.
doi pubmed pmc - Schwartz WB, Relman AS. Effects of electrolyte disorders on renal structure and function. N Engl J Med. 1967;276(7):383-389.
doi pubmed - Lee EY, Yoon H, Yi JH, Jung WY, Han SW, Kim HJ. Does hypokalemia contribute to acute kidney injury in chronic laxative abuse? Kidney Res Clin Pract. 2015;34(2):109-112.
doi pubmed pmc - Torres VE, Young WF, Jr., Offord KP, Hattery RR. Association of hypokalemia, aldosteronism, and renal cysts. N Engl J Med. 1990;322(6):345-351.
doi pubmed - Arimura Y, Tanaka H, Yoshida T, Shinozaki M, Yanagida T, Ando T, Hirakata H, et al. Anorexia nervosa: an important cause of chronic tubulointerstitial nephropathy. Nephrol Dial Transplant. 1999;14(4):957-959.
doi pubmed - Hasegawa S, Shibata M, Mochizuki M, Katsuki T, Tada M, Hinoshita F. Non-uniform progression of chronic tubulointerstitial nephritis and widespread nephrocalcification in a patient with anorexia nervosa. Intern Med. 2017;56(5):545-549.
doi pubmed pmc - Reungjui S, Roncal CA, Sato W, Glushakova OY, Croker BP, Suga S, Ouyang X, et al. Hypokalemic nephropathy is associated with impaired angiogenesis. J Am Soc Nephrol. 2008;19(1):125-134.
doi pubmed pmc - Praga M, Gonzalez E. Acute interstitial nephritis. Kidney Int. 2010;77(11):956-961.
doi pubmed - Veltri KT, Mason C. Medication-induced hypokalemia. P T. 2015;40(3):185-190.
pubmed pmc - Sinnamon KT, Courtney AE, Harron C, O'Rourke DM, Mullan RN. Tubulointerstitial nephritis and uveitis (TINU) syndrome: epidemiology, diagnosis and management. NDT Plus. 2008;1(2):112-116.
doi pubmed pmc - Braden GL, O'Shea MH, Mulhern JG. Tubulointerstitial diseases. Am J Kidney Dis. 2005;46(3):560-572.
doi pubmed - Mandeville JT, Levinson RD, Holland GN. The tubulointerstitial nephritis and uveitis syndrome. Surv Ophthalmol. 2001;46(3):195-208.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


