| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 7, July 2024, pages 117-119
Prompt Identification and Intervention for Ischemic Monomelic Neuropathy in Preventing Major Patient Disability
Raja GnanaDeva, b, Aldin Malkoca, b, c, Jeffrey Hsua, Iden Andacheha
aKaiser Fontana Medical Center, Fontana, CA, USA
bArrowhead Regional Medical Center, Colton, CA, USA
cCorresponding Author: Aldin Malkoc, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted March 25, 2024, accepted May 15, 2024, published online June 19, 2024
Short title: Prompt Identification of IMN
doi: https://doi.org/10.14740/jmc4206
| Abstract | ▴Top |
Ischemic monomelic neuropathy (IMN) is a rare complication of arteriovenous fistulas (AVFs) and arteriovenous grafts (AVGs). Diagnosis of the condition is often delayed, with debilitating outcomes for patients. We present two cases of IMN in which prompt identification and intervention prevented major disability. The first case involved an 84-year-old female who underwent a left upper extremity brachioaxillary AVG. The procedure was performed under local anesthesia and a 4 - 7 mm tapered PTFE Propaten graft was used. At the conclusion of the case, a palpable radial artery pulse was noted. In the post-anesthesia care unit (PACU), the patient had ipsilateral increasing arm and hand pain. On exam, the patient had a cool left hand with a 2+ radial pulse. The patient was taken back to the operating room and the AVG was ligated with repair of the brachial artery. The second case involved a 64-year-old male who underwent a single-staged right brachiobasilic AVF with transposition. Surgery was performed with local and regional block. At case completion, the patient was noted to have a palpable radial pulse. In the PACU, patient had increased pain and paralysis to the right hand. Patient’s right hand had complete paralysis of the fingers and reported severe forearm pain. Within 10 min of fistula ligation under local anesthesia, his symptoms resolved. We present two cases involving different arteriovenous access conduits. The time from procedure completion to reported onset of symptoms was approximately 260 min, and time from symptoms onset to surgical incision was 70 min. Early recognition, diagnosis, and management of IMN in these cases protected patients from major long-term morbidity. Owing to this pathology, post-op observation protocols and even re-admission protocols should be set after hemodialysis access creation in order to avoid delays in diagnosis and patient disability.
Keywords: Ischemic monomelic neuropathy; AV fistula; Steal syndrome
| Introduction | ▴Top |
Ischemic monomelic neuropathy (IMN) is a rare complication of both arteriovenous graft (AVG) as well as arteriovenous fistula (AVF) creation. A rare complication of dialysis access creation, IMN has an estimated prevalence of 0.5% in all arteriovenous (AV) access creations [1]. The pathology was first described by Bolton et al in 1979 following the creation of radial-cephalic graft using bovine carotid artery as conduit [2]. Signs and symptoms of IMN include arm or hand weakness and pain shortly after surgery. These symptoms can be seen occurring immediately after surgery and are often diagnosed in the post-acute care unit. Diagnosis of the condition is often delayed, with debilitating outcomes for patients. There are few reports of IMN associated with the lower extremities; most cases are associated with AV access with the brachial artery used as inflow. Older patients with pre-existing peripheral neuropathy from long standing diabetes mellitus are the group at highest risk [3-5]. There is no clearly defined time to interventions for symptoms of IMN; however, immediate diagnosis means more time for adequate treatment. In most cases, once this diagnosis is made, immediate exploration in the operating room is warranted. We present two cases of IMN which developed after creation of AV access at our institution. Prompt identification and intervention prevented major disability in these patients.
| Case Reports | ▴Top |
Case 1
The first case involved an 84-year-old female with chronic kidney disease (stage 4), diabetes mellitus, and atrial fibrillation who underwent a left upper extremity brachioaxillary AVG. The procedure was performed under local anesthesia and a 4 - 7 mm tapered PTFE Propaten graft was used. At the conclusion of the case, a palpable radial artery pulse was noted. In the pos-anesthesia care unit (PACU), the patient had ipsilateral increasing arm and hand pain. On review of the patient’s vitals, there was no signs of tachycardia or hypotension. Time from procedure completion to documentation of symptoms was 103 min. On exam, the patient had a cool left hand with a 2+ radial pulse. Due to the emergent probable diagnosis, this patient was taken emergently to the operating room. The patient was taken back to the operating room and the AVG was ligated with repair of the brachial artery.
Case 2
The second case involved a 64-year-old male with end-stage renal disease, coronary artery disease, heart failure with an ejection fraction of 15-20%, and chronic lymphocytic leukemia (CLL). He had a prior right radiocephalic AVF which thrombosed; fistulogram demonstrated a diseased radial artery (Fig. 1). Patient underwent a single-staged right brachiobasilic AVF with transposition; single-stage was performed to expedite patient’s chemotherapy treatments for CLL. Surgery was performed with local and regional block. At case completion, the patient was noted to have a palpable radial pulse with an excellent thrill through the transposed basilic vein. Similarly like case 1, there was no signs of tachycardia or hypotension. In the PACU, patient had increased pain and paralysis to the right hand. Time from procedure completion to documentation of symptoms was 217 min. Patient’s right hand was warm with a 2+ radial pulse; however, patient had complete paralysis of his fingers and reported severe forearm pain. Within 10 min of fistula ligation under local anesthesia, his symptoms resolved.
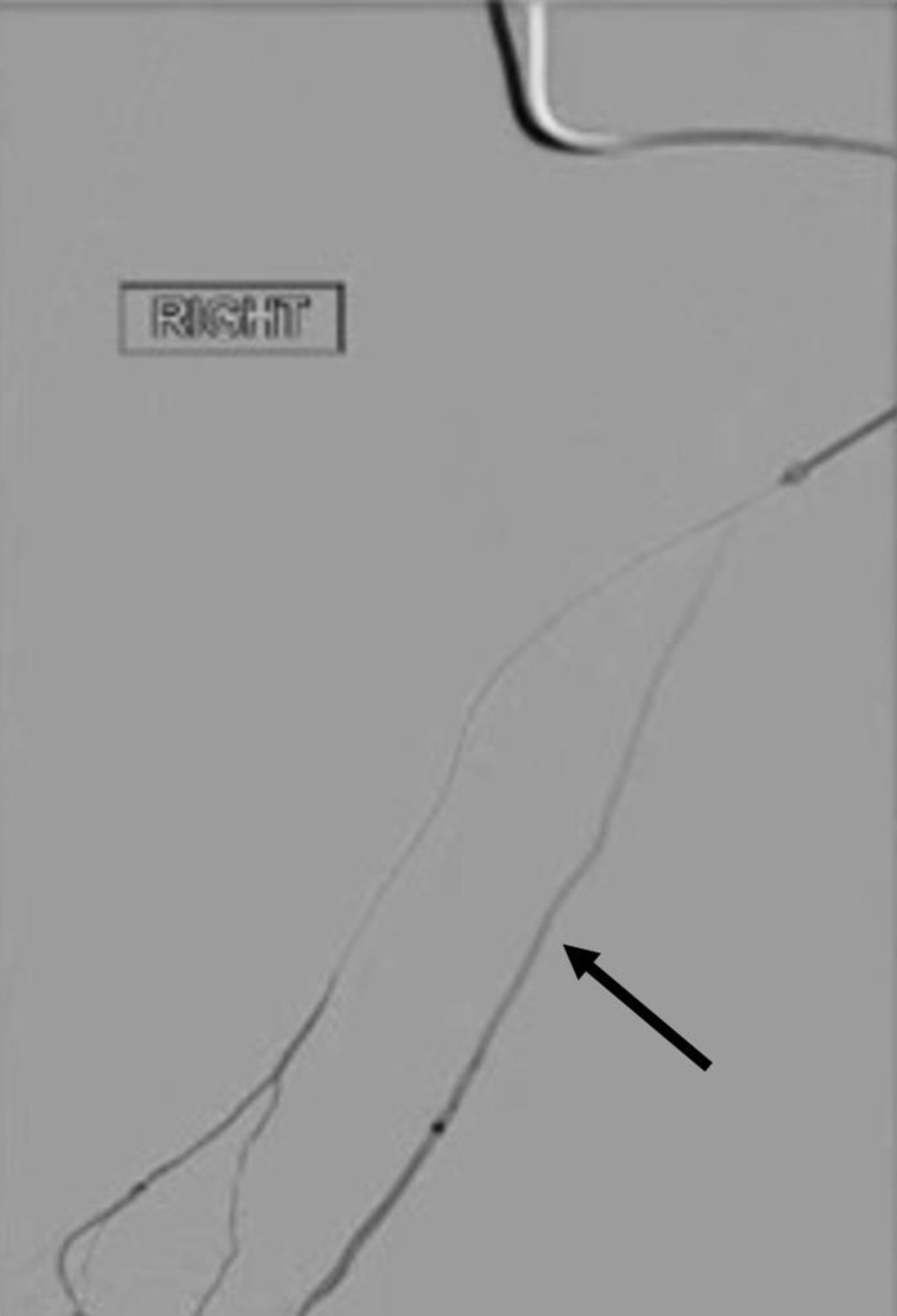 Click for large image | Figure 1. The right below elbow radial artery and ulnar artery. The black arrow shows the radial artery that was noted to be diseased. This was noted on fistulogram performed to evaluate failed radio-cephalic arteriovenous fistula. |
| Discussion | ▴Top |
The patholophysiology of IMN is thought to be due directly to acute on chronic changes in perfusion. Chronic microvascular destruction of perineural vessels lowers the ischemic threshold of associated nerves. These nerves therefore cannot tolerate a further decrease in perfusion [6]. In particular, the antecubital fossa is considered a watershed region for the vasovasorum of the median, ulnar, and radial nerves [7]. This underlying physiology perhaps explains why IMN has not been observed in access distal to the brachial artery [7, 8]. While our two cases had uniquely different fistulas, both fistulas were proximal to the brachial artery. There is no clear suggestion that the use of graft results in high incidence of IMN but clearly being proximal to the brachial artery was a common factor.
IMN presents within hours of AV access creation. Signs and symptoms of IMN include weakness, pain, and paralysis with dysesthesias of hand and forearm muscles. IMN can be differentiated from classical vascular steal syndrome in that the hand is typically warm, with palpable pulses, without other signs of vascular compromise [5, 9, 10]. In patients for whom IMN is suspected, the extremity should be evaluated for hematoma or direct nerve damage; in their absence, IMN should be considered and managed as soon as recognized [6]. No clear evidence suggests gender influence the development of IMN.
Significant morbidities, contractures and loss of extremity function, were avoided in the patients presented in this series due to rapid identification and intervention. Accomplishing this required prompt recognition by the patient’s care team in the PACU, vascular surgeon, and anesthesia. In our first case, onset of symptoms was less than 2 h after cessation of surgery; in the second case, onset of symptoms was over 3 h after surgery completion. The role of local-regional block may have blunted in the onset of symptoms in the latter case.
A review of the literature failed to demonstrate a recommended length of time for which patients should be observed in the PACU following AV access creation. This is likely due to high variability amongst centers where AV access procedures are performed, ranging from ambulatory surgery centers to tertiary acute care hospitals like ours. We propose that patients may benefit from more standardized PACU protocols ensuring safe discharges home. Similarly, re-admission strategies directly to the PACU may avoid potentially excessive wait times in the emergency department that could increase morbidity in postoperative patients.
In the case of these two patients, emergency department admission, intake, workup, would inevitably have led to several hours of delay in diagnosis and treatment. Establishment of PACU and re-admission protocols for AV access patients are therefore imperative to prevent major disability in IMN patients.
Learning points
In this series, we present two cases of IMN. Each case was performed by a different vascular surgery attending. Additionally, one case was an AVG and the other a brachiobasilic AVF. Given the rarity of the diagnosis, it is important that all cases of IMN are reported. For each of our patients, early identification and management prevented significant morbidity.
Acknowledgments
None to declare.
Financial Disclosure
The authors have no financial or funding disclosures.
Conflict of Interest
The authors declare there is no conflict of interest.
Informed Consent
Informed consent was obtained for use of de-identified information for publication per our Institutional Review Board policy.
Author Contributions
RG performed the initial manuscript write-up, literature review, and editing of the manuscript. AM assisted with the manuscript write-up, literature review, and editing of the manuscript. JH assisted with the manuscript write-up, literature review, and editing of the manuscript. IA attended on the case and contributed to decision-making, management of the patient, literature review as well as editing of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
AV: arteriovenous; AVFs: arteriovenous fistulas; AVGs: arteriovenous grafts; IMN: ischemic monomelic neuropathy; PACU: post-anesthesia care unit
| References | ▴Top |
- Ballard JL, Bunt TJ, Malone JM. Major complications of angioaccess surgery. Am J Surg. 1992;164(3):229-232.
doi pubmed - Bolton CF, Driedger AA, Lindsay RM. Ischaemic neuropathy in uraemic patients caused by bovine arteriovenous shunt. J Neurol Neurosurg Psychiatry. 1979;42(9):810-814.
doi pubmed pmc - Wilbourn AJ, Furlan AJ, Hulley W, Ruschhaupt W. Ischemic monomelic neuropathy. Neurology. 1983;33(4):447-451.
doi pubmed - Honet JC, Wajszczuk WJ, Rubenfire M, Kantrowitz A, Raikes JA. Neurological abnormalities in the leg(s) after use of intraaortic balloon pump: report of six cases. Arch Phys Med Rehabil. 1975;56(8):346-352.
pubmed - Miles AM. Vascular steal syndrome and ischaemic monomelic neuropathy: two variants of upper limb ischaemia after haemodialysis vascular access surgery. Nephrol Dial Transplant. 1999;14(2):297-300.
doi pubmed - Hye RJ, Wolf YG. Ischemic monomelic neuropathy: an under-recognized complication of hemodialysis access. Ann Vasc Surg. 1994;8(6):578-582.
doi pubmed - Dyck PJ, Conn DL, Okazaki H. Necrotizing angiopathic neuropathy. Three-dimensional morphology of fiber degeneration related to sites of occluded vessels. Mayo Clin Proc. 1972;47(7):461-475.
pubmed - Miles AM. Upper limb ischemia after vascular access surgery: differential diagnosis and management. Semin Dial. 2000;13(5):312-315.
doi pubmed - Duncan H, Ferguson L, Faris I. Incidence of the radial steal syndrome in patients with Brescia fistula for hemodialysis: its clinical significance. J Vasc Surg. 1986;4(2):144-147.
pubmed - Wytrzes L, Markley HG, Fisher M, Alfred HJ. Brachial neuropathy after brachial artery-antecubital vein shunts for chronic hemodialysis. Neurology. 1987;37(8):1398-1400.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


