| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 11, November 2024, pages 335-340
Unmasking the Rarity: A Case Report on Platypnea-Orthodeoxia Syndrome With Successful Resolution Through Patent Foramen Ovale Closure
Khurram Arshada, f, g, Rabia Latifb, f, Farman Alia, Aman Ullahc, William Limd, Mehrun Nisa Ahmede, Ahmad Munird
aDepartment of Internal Medicine, Corewell Health Dearborn Hospital, Dearborn, MI, USA
bDepartment of Internal Medicine, McLaren Flint Hospital, Flint, MI, USA
dDepartment of Cardiology, McLaren Flint Hospital, Flint, MI, USA
cDepartment of Internal Medicine, SSM Health, St. Louis University Hospital, St. Louis, MO, USA
eCMH Lahore Medical College, Lahore, Pakistan
fThese authors contributed equally to this article.
gCorresponding Author: Khurram Arshad, Department of Internal Medicine, Corewell Health Dearborn Hospital, Dearborn, MI, USA
Manuscript submitted May 31, 2024, accepted September 2, 2024, published online October 10, 2024
Short title: POS With Successful Resolution by PFO Closure
doi: https://doi.org/10.14740/jmc4257
| Abstract | ▴Top |
Platypnea-orthodeoxia syndrome (POS) is an uncommon yet clinically significant medical phenomenon characterized by dyspnea, a distressing symptom manifesting as breathlessness upon assuming an upright position, which notably improves upon reclining. In stark contrast to orthopnea, where dyspnea worsens in a supine position, POS uniquely presents with decreased blood oxygen saturation upon transitioning from lying down to standing up. This syndrome poses diagnostic challenges due to its subtle symptomatology and requires a high index of clinical suspicion for accurate identification. Herein, we present a case of a 79-year-old female with a complex medical history, notably encompassing deep vein thrombosis (DVT) and subsequent pulmonary embolism (PE) necessitating long-term anticoagulation with warfarin, a history of breast cancer status post lumpectomy and chemotherapy, hypertension, and chronic kidney disease (CKD). The patient was admitted from a living facility with persistent hypoxemia and clinical features suggestive of POS. Despite comprehensive physical examination and routine laboratory investigations, no overt abnormalities were discerned. However, echocardiography unveiled a severe patent foramen ovale (PFO) with right-to-left shunting, corroborating the diagnosis of POS. Subsequently, percutaneous closure of the PFO using the GORE CARDIOFORM septal occluder was performed, with fluoroscopy confirming successful device placement within the atrial septum. Remarkably, the patient demonstrated significant improvement in oxygenation post-procedure, prompting her discharge within 2 days. POS, though rare, holds substantial clinical significance owing to its potential to precipitate considerable morbidity and mortality. The pathophysiological basis of POS lies in the discordance between pulmonary and systemic blood flow, culminating in arterial desaturation upon assuming an upright posture. Timely recognition and intervention are imperative to mitigate symptom burden and avert the progression of associated complications. Early diagnosis facilitates the implementation of targeted therapeutic strategies, thereby alleviating dyspnea and forestalling adverse sequelae stemming from this syndrome. As such, heightened awareness among healthcare practitioners regarding the nuanced presentation of POS is paramount to expedite appropriate management and optimize patient outcomes.
Keywords: Platypnea-orthodeoxia syndrome; Dyspnea; GORE CARDIOFORM septal occluder; Orthopnea
| Introduction | ▴Top |
Platypnea-orthodeoxia syndrome (POS) is a rare medical condition characterized by dyspnea that worsens when standing or sitting and improves upon lying down, contrasting orthopnea. POS is marked by decreased blood oxygen saturation upon transitioning from supine to upright positions [1]. Identifying its causes is crucial for diagnosing and managing cardiac ailments, broadly categorized into intracardiac shunting, pulmonary shunting, ventilation-perfusion mismatch, or their combination [2].
Intracardiac shunting involves abnormal blood passage between heart chambers, often through defects like patent foramen ovale (PFO) or atrial septal defect (ASD). Pulmonary shunting occurs when blood bypasses the alveolar capillary interface, seen in conditions like pulmonary arteriovenous malformations (PAVMs) or hepatopulmonary syndrome (HPS). Ventilation-perfusion mismatch arises from disorders disrupting airflow and blood flow balance in the lungs, like chronic obstructive pulmonary disease (COPD) or pulmonary embolism (PE) [2].
Despite its rarity, POS warrants clinical suspicion due to its subtle presentation. Comprehensive evaluation, including patient history and advanced diagnostic tools like echocardiography, is essential for accurate diagnosis and management [2].
| Case Report | ▴Top |
We present a case of a 79-year-old female presenting to the hospital from her living facility with symptoms of persistent hypoxemia and POS. Her past medical history included deep vein thrombosis (DVT) with subsequent PE for which she was on long-term anticoagulation with warfarin, a history of breast cancer status post lumpectomy and chemotherapy, hypertension, and chronic kidney disease (CKD).
Upon arrival, the patient’s vital signs were: temperature of 36 °C, respiratory rate of 13 breaths per minute, blood pressure of 149/54 mm Hg, heart rate of 105 beats per minute, and oxygen saturation of 98% on 10 - 15 L/min of high-flow nasal cannula (HFNC).
A thorough physical examination revealed normal first and second heart sounds without any murmurs, rubs, or gallops. The lung examination showed bilateral vesicular breath sounds without any wheezes, crackles, or additional sounds. The abdominal examination was unremarkable, and no peripheral edema was noted.
Initial laboratory tests are presented in Table 1. Arterial blood gas analysis demonstrated a pH of 7.394, a partial pressure of carbon dioxide (PaCO2) of 44.8 mm Hg, a partial pressure of oxygen (PaO2) of 71 mm Hg, and bicarbonate (HCO3) of 27.4 mmol/L, indicating mild respiratory acidosis.
 Click to view | Table 1. Laboratory Results |
An echocardiogram with bubble study was performed, revealing a severe PFO with a right-to-left shunt, as shown in Figure 1. Given the severity of the shunt and the patient’s symptoms, a decision was made to close the PFO. The procedure was performed using the GORE CARDIOFORM septal occluder, as depicted in Figure 2. Post-procedure fluoroscopy confirmed the placement of the closure device in the atrial septum, as shown in Figure 3.
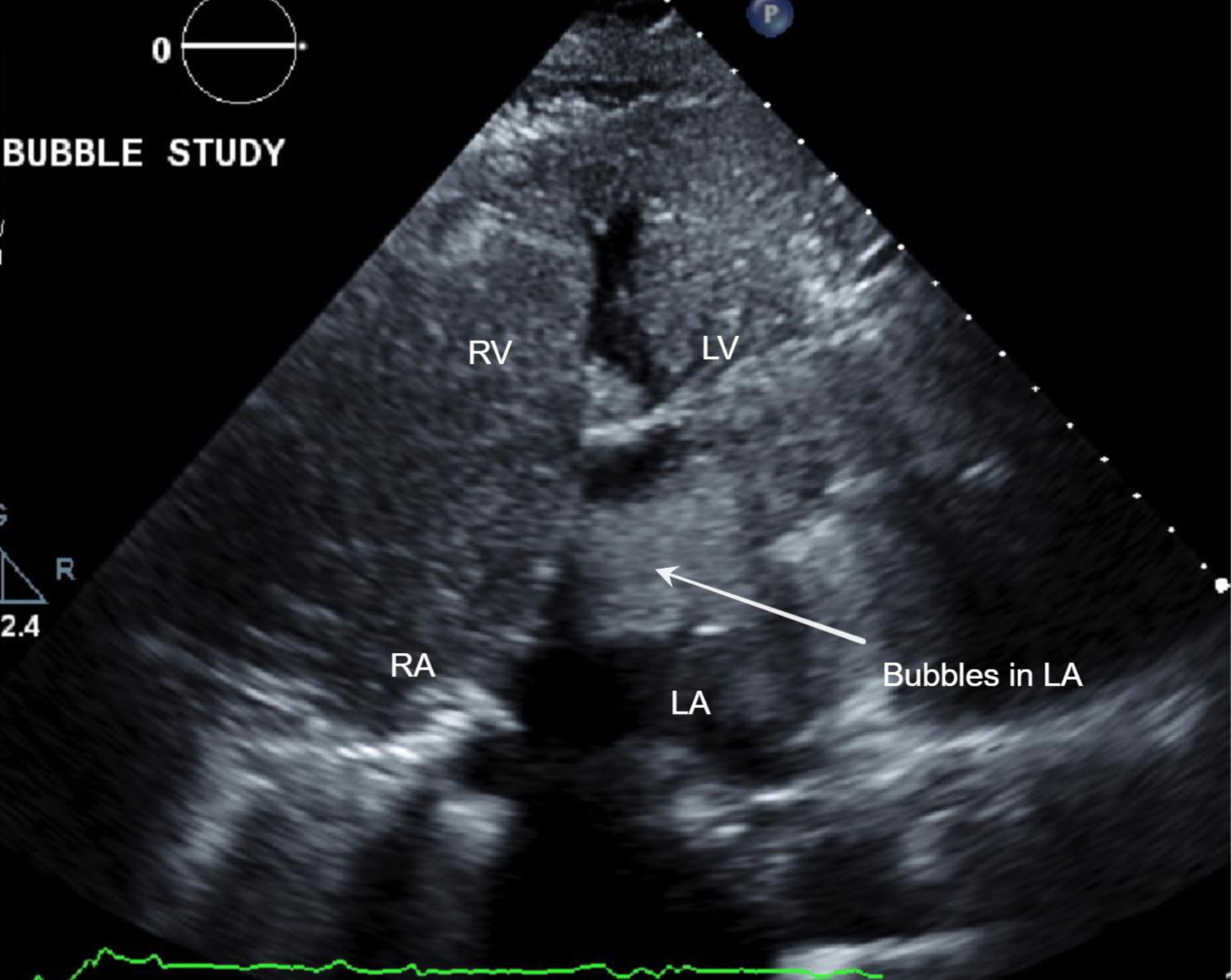 Click for large image | Figure 1. Echo with bubble studies showing bubbles across the patent foramen ovale (white arrow). LA: left atrium; LV: left ventricle; RA: right atrium; RV: right ventricle. |
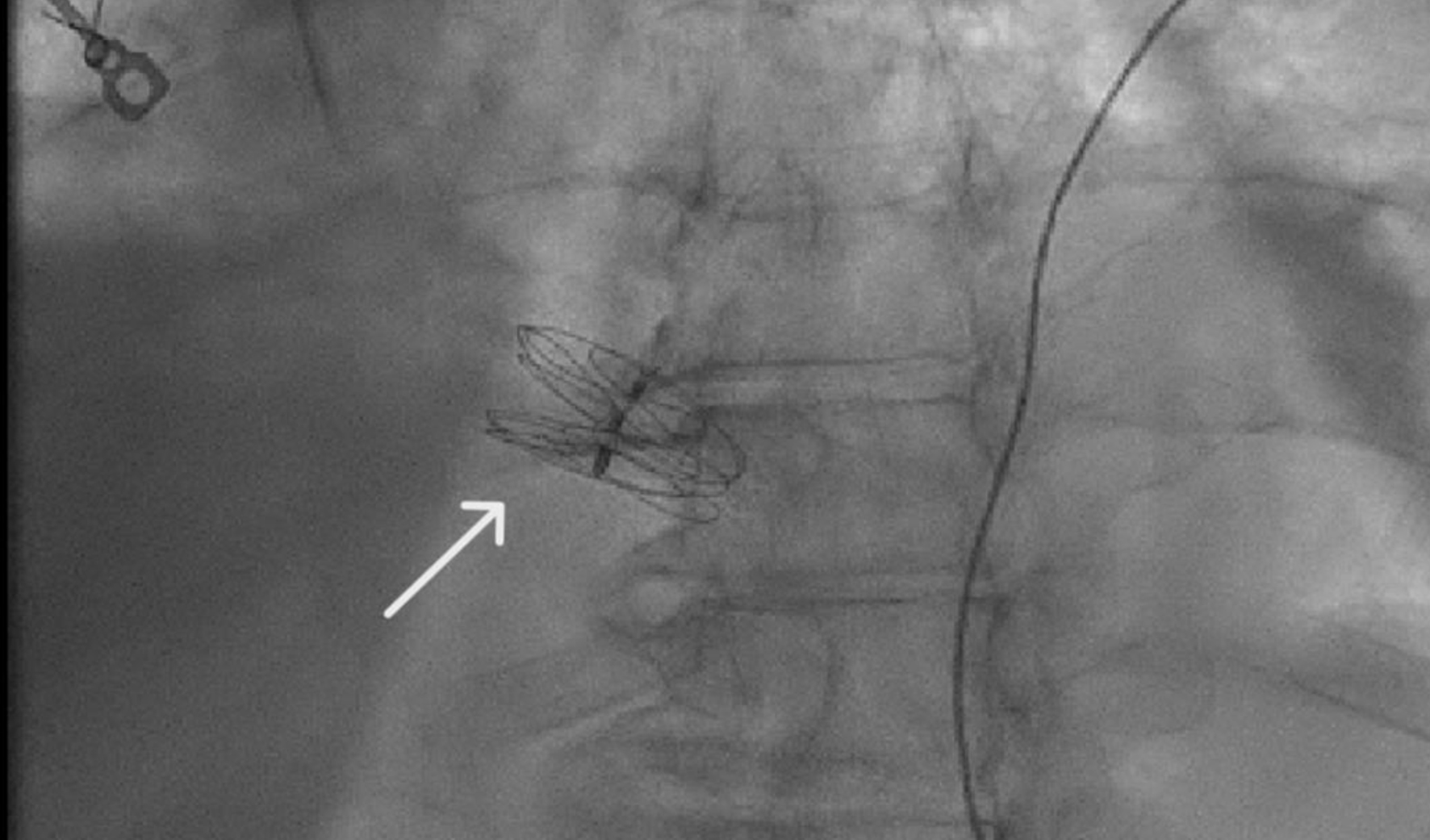 Click for large image | Figure 2. Fluoroscopy showing GORE CARDIOFORM septal occluder in place (white arrow). |
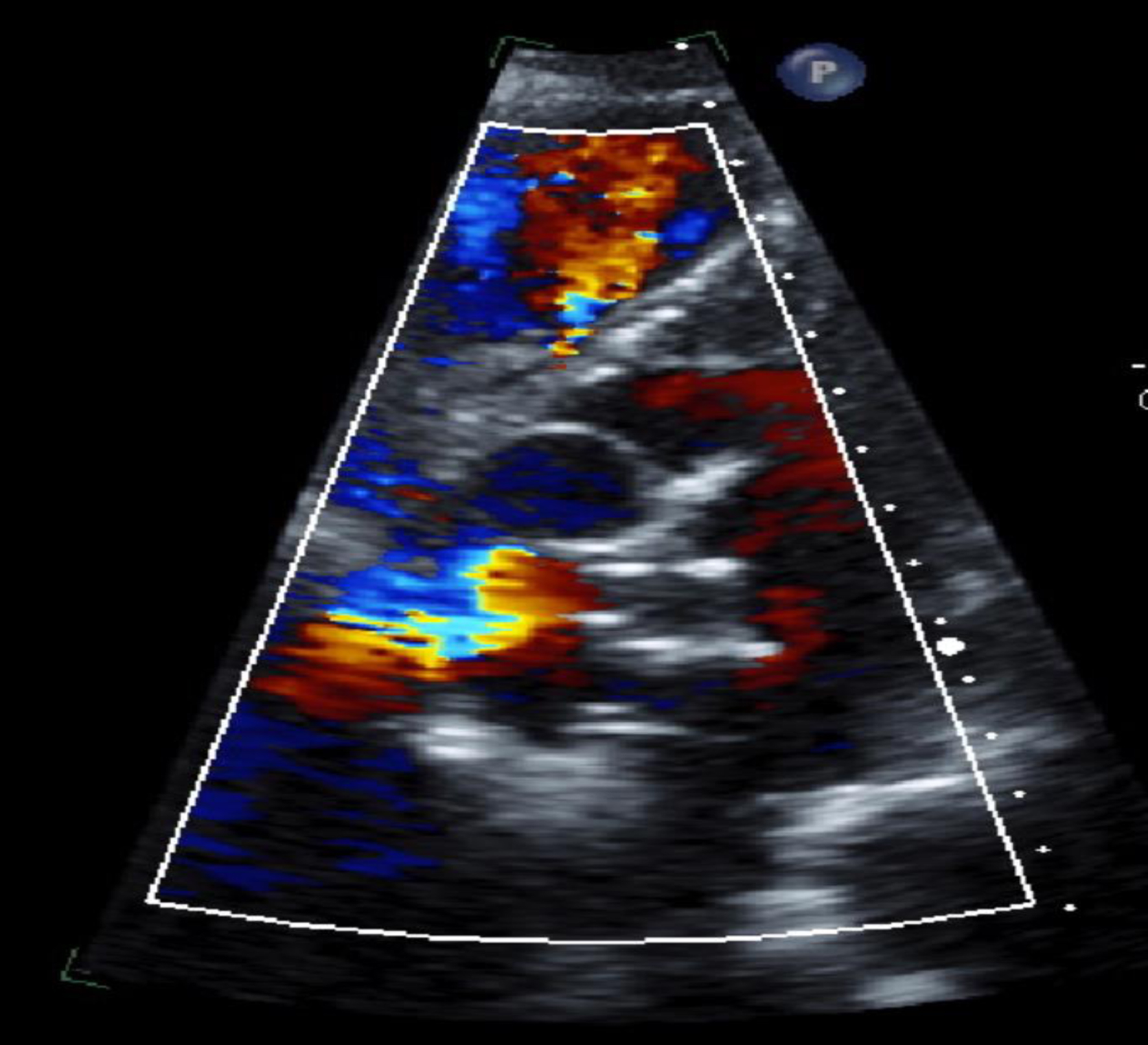 Click for large image | Figure 3. Echo showing closure device in the atrial septum. |
The patient’s oxygenation improved significantly following the procedure, with her oxygen saturation levels stabilizing on room air. She experienced substantial relief from her symptoms of dyspnea and was subsequently discharged 2 days later in a stable condition.
| Discussion | ▴Top |
This case report presents a rare and compelling instance of POS in a 79-year-old female, uniquely characterized by its successful resolution through the percutaneous closure of a PFO. The rarity of POS, coupled with its complex pathophysiology involving intracardiac shunting, underscores the significance of early recognition and intervention. This case adds to the limited literature on POS by demonstrating how timely PFO closure can lead to marked improvement in symptoms and oxygenation, emphasizing the importance of heightened clinical suspicion in similar presentations. PFO is a frequently occurring entity that is usually considered benign. However, isolated cases of POS through a PFO have been described, which can be highly symptomatic and difficult to identify [3]. This report not only reinforces the clinical relevance of POS but also highlights the critical role of tailored therapeutic interventions in optimizing patient outcomes.
POS is a rare condition characterized by dyspnea, or difficulty breathing, which occurs specifically when the patient is in an upright position. This is accompanied by a drop in arterial oxygen saturation, known as desaturation. Patients with POS may find it particularly challenging to perform everyday activities, as transitioning to a standing or sitting position can provoke significant breathlessness and oxygen desaturation. The condition is typically triggered by abnormalities in the heart or lungs, such as an ASD, PFO, or HPS. Unfortunately, POS is often underreported, primarily because it requires a high degree of clinical suspicion for diagnosis [4].
Central to the pathophysiology of POS is the aberrant mixing of deoxygenated venous blood with oxygen-rich arterial blood, precipitated by two primary mechanisms: intracardiac and intrapulmonary. The intracardiac pathway entails the transfer of deoxygenated blood from the right to the left atrium via defects such as PFO, ASD, or a fenestrated atrial septal aneurysm (ASA) [5, 6]. These anomalies circumvent the pulmonary circulation, leading to systemic desaturation upon assuming an upright posture. Intrapulmonary abnormalities encompass vascular anomalies within the lung parenchyma, exemplified by conditions like PAVMs, HPS, and various pulmonary parenchymal disorders [5, 6]. These pathologies engender a mismatch between ventilation and perfusion, allowing deoxygenated blood to bypass pulmonary gas exchange and enter systemic circulation.
For PFO to cause POS, there must have been a change in the position of the interatrial septum (IAS) to facilitate the direction of flow from the inferior vena cava towards the septum and the passage of deoxygenated blood from the right to the left atrium [3]. In further elaboration, intracardiac shunting is primarily facilitated by the persistence of fetal structures like the foramen ovale, which normally closes after birth. However, in cases where this closure is incomplete, as seen in PFO or ASD, the integrity of the atrial septum is compromised, permitting the right-to-left shunting of blood. This results in the admixture of poorly oxygenated venous blood with oxygenated arterial blood, leading to systemic hypoxemia. In contrast, intrapulmonary shunting arises from vascular malformations or abnormalities within the pulmonary circulation. Conditions such as PAVMs or HPS disrupt the normal distribution of blood flow within the lungs, creating areas of ventilation-perfusion mismatch. Consequently, deoxygenated blood bypasses regions of gas exchange and directly enters the systemic circulation, further exacerbating hypoxemia [5, 6].
The intricate interplay between these mechanisms underscores the multifaceted nature of POS pathophysiology. While intracardiac defects contribute to direct right-to-left shunting of blood, intrapulmonary abnormalities exacerbate hypoxemia through ventilation-perfusion mismatch. This comprehensive understanding of the underlying pathophysiological processes is pivotal in guiding diagnostic and therapeutic interventions aimed at mitigating symptoms and improving patient outcomes.
In this particular case, the diagnosis of POS was supported by the presence of a PFO, as evidenced by a bubble study that revealed significant right-to-left shunting. The patient experienced a marked improvement in both symptoms and oxygenation following the percutaneous closure of the PFO. This case underscores the pivotal role that intracardiac defects, such as PFO, can play in the pathogenesis of POS. PFOs are relatively common, occurring in approximately 25% of adults. Typically, the foramen ovale, a small opening between the right and left atria, closes after birth as pulmonary resistance and right-sided heart pressures decrease. However, in some individuals, this opening remains patent, potentially leading to complications such as cerebrovascular accidents and, in rare cases, conditions like POS [7].
The management of POS, particularly when associated with a PFO, is guided by established clinical guidelines and evidence from the literature. The Society for Cardiovascular Angiography and Interventions (SCAI) recommends the closure of PFO in patients with POS when no other explainable cause of the syndrome is identified [8]. This recommendation is backed by studies that demonstrate significant clinical improvements following percutaneous closure of PFOs in affected patients [7]. For instance, a study titled “Percutaneous intervention to treat platypnea-orthodeoxia syndrome” reported on 52 patients who underwent percutaneous closure of an interatrial communication between January 1997 and July 2015. The study concluded that patients with POS could be effectively treated with percutaneous interventions, which may involve various types of closure devices, leading to substantial improvements in symptoms and oxygenation levels [9].
This case highlights the critical importance of considering POS in the differential diagnosis of unexplained dyspnea and hypoxemia, especially in patients with known risk factors for intracardiac shunts or pulmonary vascular abnormalities. Early recognition and diagnosis are vital, as they allow for timely intervention that can dramatically improve patient outcomes. The patient’s positive response to the PFO closure in this case demonstrates the efficacy of percutaneous interventions in managing POS and emphasizes the need for increased clinical awareness of this syndrome.
Learning points
POS presents a diagnostic challenge due to its rarity and diverse etiologies. However, prompt recognition and understanding of its underlying mechanisms are imperative for effective management. This case report underscores the successful resolution of POS through percutaneous closure of a PFO, demonstrating the pivotal role of tailored interventions in improving patient outcomes.
The complexity of POS lies in its diverse pathophysiological mechanisms, including intracardiac shunting and intrapulmonary vascular abnormalities, leading to dyspnea and arterial desaturation, particularly in the upright position. Despite its rarity, POS warrants consideration in patients presenting with unexplained dyspnea and hypoxemia, especially in those with predisposing conditions such as intracardiac defects or pulmonary vascular abnormalities.
In this case, the patient’s symptoms of persistent hypoxemia and POS were effectively addressed through the closure of a severe PFO. Following the procedure, the patient experienced significant improvements in oxygenation and symptom relief, leading to her discharge in a stable condition. This outcome underscores the efficacy of percutaneous interventions in managing POS and highlights the importance of early diagnosis and appropriate treatment.
Moving forward, increased clinical awareness and interdisciplinary collaboration are essential for enhancing the recognition and management of POS. By fostering a better understanding of this rare syndrome among healthcare providers, we can ensure timely intervention and improved outcomes for affected individuals. This case serves as a testament to the potential for significant improvement in patient quality of life through targeted interventions in the management of POS.
In conclusion, while POS remains a diagnostic challenge, advancements in diagnostic modalities and therapeutic interventions offer hope for improved patient care. Continued research and clinical vigilance are essential for unraveling the complexities of POS and optimizing management strategies, ultimately enhancing the prognosis and well-being of affected individuals.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from all subjects involved in the study.
Author Contributions
Khurram Arshad and Rabia Latif: research, manuscript development, data collection, interpretation, and conception and design; Farman Ali, Aman Ullah, William Lim, Mehrun Nisa Ahmed, and Ahmad Munir: research, manuscript development, data collection, and interpretation.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Henkin S, Negrotto S, Pollak PM, Cullen MW, O’Cochlain DF, Wright RS. Platypnea-orthodeoxia syndrome: diagnostic challenge and the importance of heightened clinical suspicion. Tex Heart Inst J. 2015;42(5):498-501.
doi pubmed pmc - De Vecchis R, Baldi C, Ariano C. Platypnea-orthodeoxia syndrome: multiple pathophysiological interpretations of a clinical picture primarily consisting of orthostatic dyspnea. J Clin Med. 2016;5(10):85.
doi pubmed pmc - Casanovas-Marba N, Feijoo-Masso C, Guillamon-Toran L, Guillaumet-Gasa E, Blanco BG, Martinez-Rubio A. Patent foramen ovale causing severe hypoxemia due to right-to-left shunting in patients without pulmonary hypertension. Clinical suspicion clues for diagnosis and treatment. Rev Esp Cardiol (Engl Ed). 2014;67(4):324-325.
doi pubmed - Gadre A, Highland KB, Mehta A. Reversible platypnea-orthodeoxia syndrome from ventilation-perfusion mismatch in interstitial lung disease: a novel etiology. Ann Am Thorac Soc. 2016;13(1):137-138.
doi pubmed - Rodrigues P, Palma P, Sousa-Pereira L. Platypnea-orthodeoxia syndrome in review: defining a new disease? Cardiology. 2012;123(1):15-23.
doi pubmed - Lopez Gaston OD. [Platypnea-orthodeoxia syndrome]. Medicina (B Aires). 2005;65(3):268-272.
pubmed - Homma S, Messe SR, Rundek T, Sun YP, Franke J, Davidson K, Sievert H, et al. Patent foramen ovale. Nat Rev Dis Primers. 2016;2:15086.
doi pubmed - Horlick E, Kavinsky CJ, Amin Z, Boudoulas KD, Carroll JD, Hijazi ZM, Leifer D, et al. SCAI expert consensus statement on operator and institutional requirements for PFO closure for secondary prevention of paradoxical embolic stroke: The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Catheter Cardiovasc Interv. 2019;93(5):859-874.
doi pubmed - Shah AH, Osten M, Leventhal A, Bach Y, Yoo D, Mansour D, Benson L, et al. Percutaneous intervention to treat platypnea-orthodeoxia syndrome: The Toronto experience. JACC Cardiovasc Interv. 2016;9(18):1928-1938.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


