| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 9, September 2024, pages 215-221
Conservative Treatment of Empyema Formation Following Intrathoracic Rib Fixation With Antibiotics and Tissue Plasminogen Activator/Dornase
Aldin Malkoca, c, Lana Mamounb, Kendall Vignarolia, Harpreet Gilla, Amira Barmanwallaa, Alexander Phana, Amanda Daouda, Alexandra Nguyena, Brandon Woodwarda
aArrowhead Regional Medical Center, Colton, CA 92324, USA
bCalifornia University of Science and Medicine, Colton, CA 92324, USA
cCorresponding Author: Aldin Malkoc, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted June 9, 2024, accepted July 16, 2024, published online August 10, 2024
Short title: Conservative Treatment of Empyema
doi: https://doi.org/10.14740/jmc4267
| Abstract | ▴Top |
Rib plating is a recommended intervention for patients with multiple rib fractures or flail chest to improve shortness of breath, significantly reduce pain, and shorten the length of hospital stay. Here, we report a unique and extremely rare finding in a patient with empyema following intrathoracic rib fixation. A 32-year-old male with a history of alcohol use disorder presented to the emergency department trauma bay after a motor vehicle accident. Computed tomography (CT) showed right hemopneumothorax and fourth to ninth rib fractures with displacement. The right fifth and sixth ribs were then plated using a titanium RibFix bridge, implanted intrathoracically along the posterior surface of the ribs. On postoperative day 11, the patient developed an empyema and a CT-guided drainage catheter was placed into the collection. The patient was given a 3-day course of tissue plasminogen activator (tPA) and DNase for the treatment of his empyema. On postoperative day 15, a repeat CT scan demonstrated significant improvement in the empyema with evidence of abscess resolution. Antibiotics were discontinued after a total of 7 days and the patient was discharged on postoperative day 20. This case report contributes information to the management of complications in intrathoracic rib fixation.
Keywords: Intrathoracic rib plating; Rib fractures; Tissue plasminogen activator and DNase
| Introduction | ▴Top |
Rib fractures occur in 10% of patients with blunt chest trauma [1]. Blunt chest trauma can result in various serious intrathoracic and extrathoracic injuries, specifically multiple rib fractures and flail chest [2]. There is a high incidence, approximately 6%, of rib fractures following blunt chest trauma such as motor vehicle accidents, bicycle accidents, and even falls from a significant height [3]. Although rib fractures are common among trauma patients, flail chest fractures are rare. Secondary complications from flail chest can be life-threatening, increasing the morbidity and mortality associated with this injury [4]. Rib fractures are often associated with shortness of breath, debilitating pain, pneumonia, and an impaired quality of life [2]. Patients with multiple rib fractures are at an even greater risk of developing complications such as pneumothorax or hemothorax and more serious acute respiratory distress syndrome (ARDS) [2, 4]. Increased concern arises from multiple rib fractures because disruption of the chest wall alters respiratory mechanics and increases respiratory effort, potentially leading to cyanosis and hypoxemia [2, 5-7].
The treatment of rib fractures is determined by the degree of injury and symptoms. Single-rib fractures are often managed conservatively with pulmonary therapy, oral pain medications, and intercostal nerve blockades as needed [8]. However, conservative management may fail for multiple rib fractures or flail chest [9]. In the case of severe rib fractures, the risk of chronic pain, empyema, prolonged respiratory insufficiency, or ventilator dependence increases [8, 9]. In recent years, there has been an increased utilization of surgical rib fracture fixation (RFF) as options have been developed ranging from bioabsorbable to permanent locking plates [9].
Although plating has been used for decades, the evolving understanding of indications and complications continues to fuel the debate between operative management and more conservative methods [2]. The most common complication after RFF is pneumonia, with an incidence as high as 90%, and the rarest complication is empyema, with an incidence of up to 5% [10]. This case report was prepared in accordance with SCARE guidelines [11]. Our case presented a rare postoperative complication after rib plating that was managed conservatively without hardware removal, contributing to the growing information on rib fixation and the management of complications, especially in intrathoracically located plates.
| Case Report | ▴Top |
A 32-year-old male with a history of alcohol use disorder presented to the emergency department trauma bay as a restrained rear-seat passenger in a motor vehicle that rear-ended a truck at a high speed. On presentation, the patient was agitated and in respiratory distress with complaints of right chest wall pain and difficulty breathing; he was subsequently intubated. Computed tomography (CT) of the chest revealed right hemopneumothorax and right fourth through ninth rib fractures with displacement (Fig. 1). A right-sided chest tube was placed with 200 mL of sanguineous output and the patient was admitted to the surgical intensive care unit (SICU) for ventilator management.
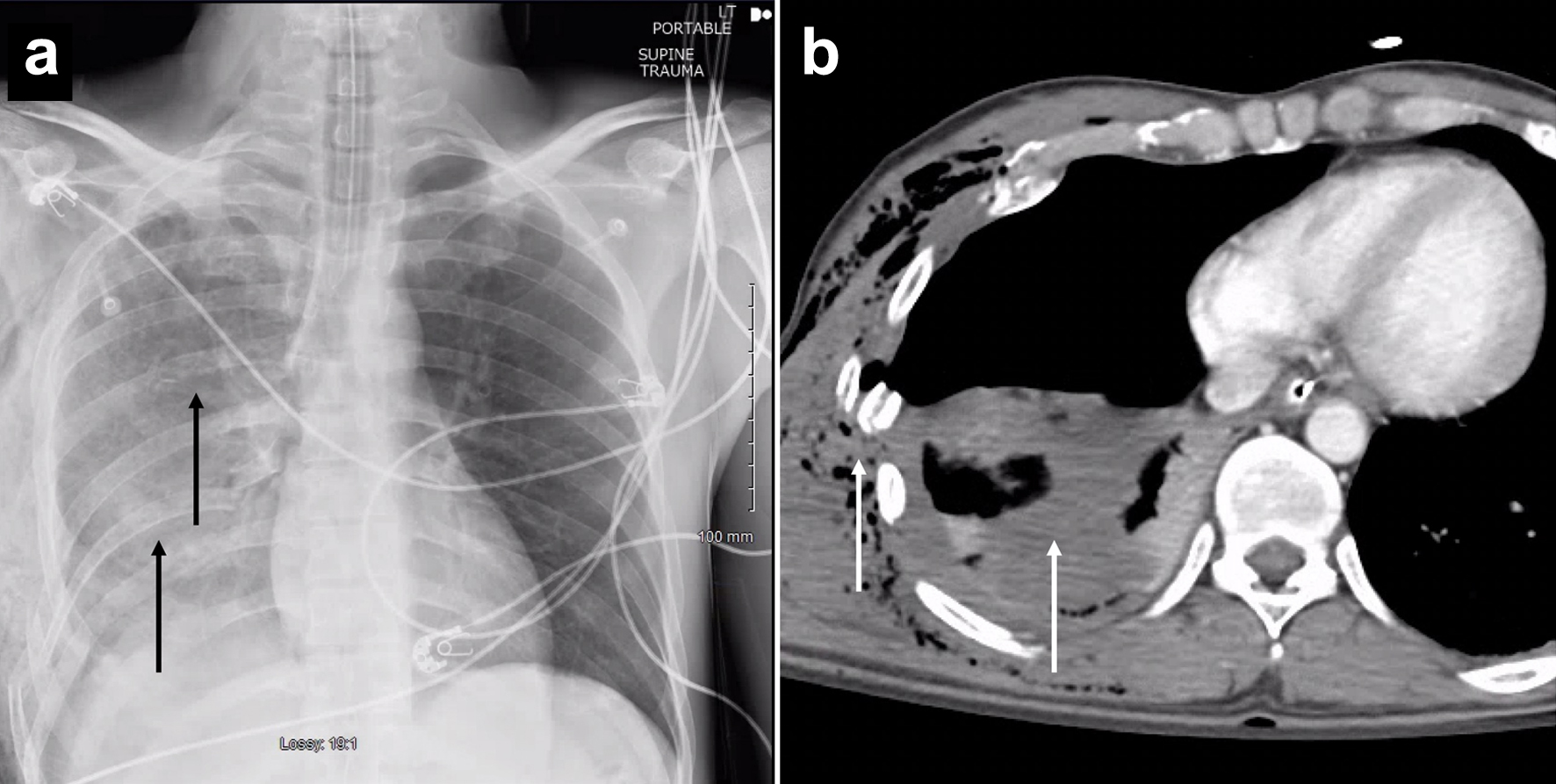 Click for large image | Figure 1. (a) Initial radiographic image of the patient’s chest. Black arrows indicate the pulmonary contusions on the initial radiographic image. (b) Computed tomography scan of the patient’s chest showing subcutaneous air along with a hemopneumothorax. White arrows indicate the rib fracture and the pulmonary contusions. |
The patient was extubated the following day with stable parameters. However, on hospital day 2, he became tachycardic, tachypneic, and hypoxic, and was subsequently re-intubated. Follow-up CT showed persistent right hemopneumothorax despite right chest tube placement with increased airspace consolidation in the right lower lung. On hospital day 4, the patient was taken to surgery for video-assisted thoracoscopy and bronchoscopy. Intraoperatively, multiple ribs were found to be fractured, with severe displacement and disruption of the parietal pleura (Fig. 2). The right fifth and sixth ribs were then plated using a titanium RibFix bridge implanted intrathoracically along the posterior surface of the ribs (Zimmer Bot; Fig. 3). The right thoracic cavity was thoroughly irrigated, and an angled inferior and straight superior chest tube was placed. On postoperative day 2, leukocytosis developed, and the patient was started on vancomycin intravenous (IV) 15 mg/kg every 8 h and piperacillin/tazobactam IV 4.5 g for empiric treatment of pneumonia. His hospital course was significant for persistent chest tube air leaks and multiple failed spontaneous breathing trials due to agitation.
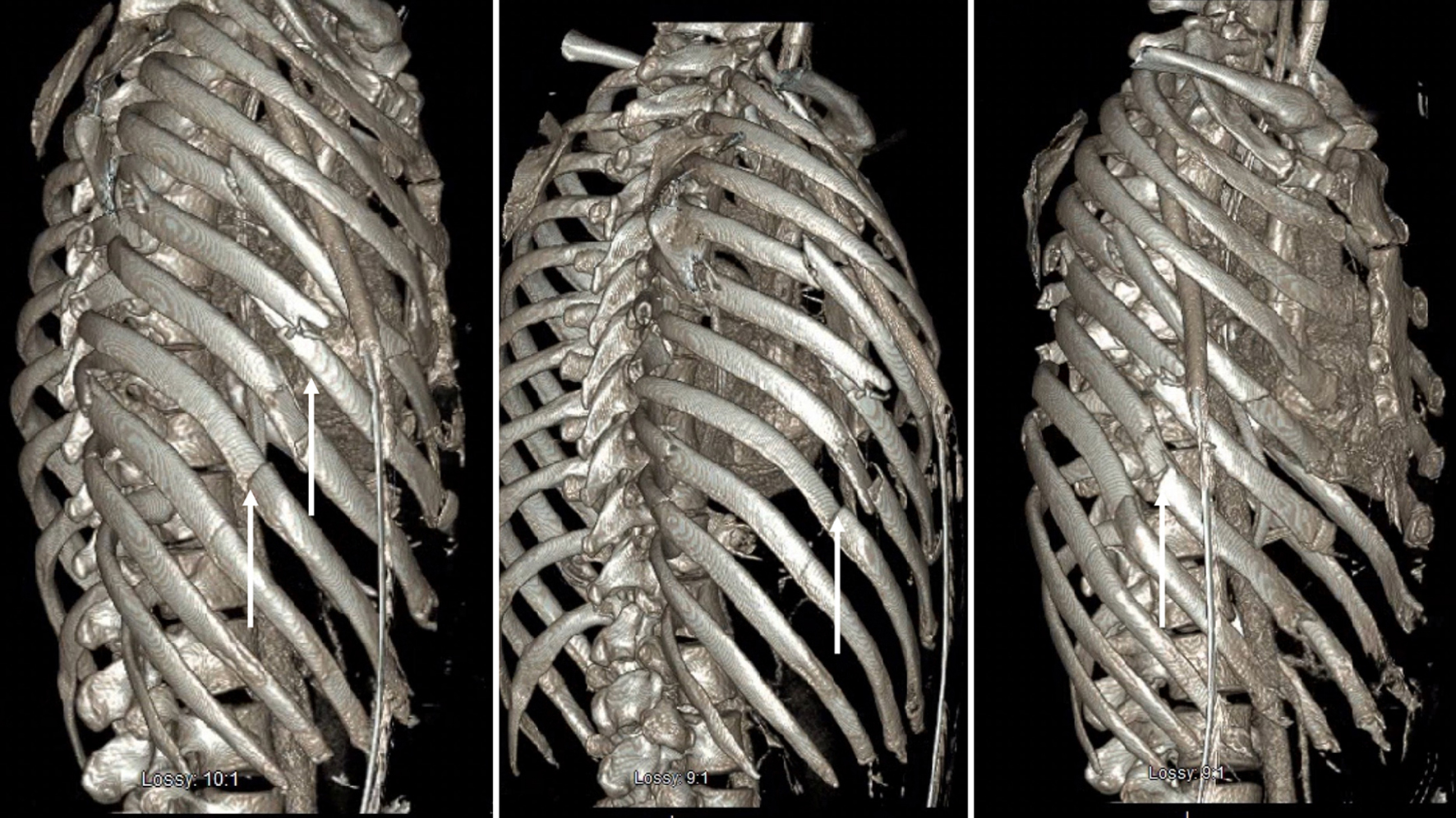 Click for large image | Figure 2. Computed tomography of three-dimensional reconstruction of the patient’s rib fractures. White arrows indicate the displaced rib fractures. |
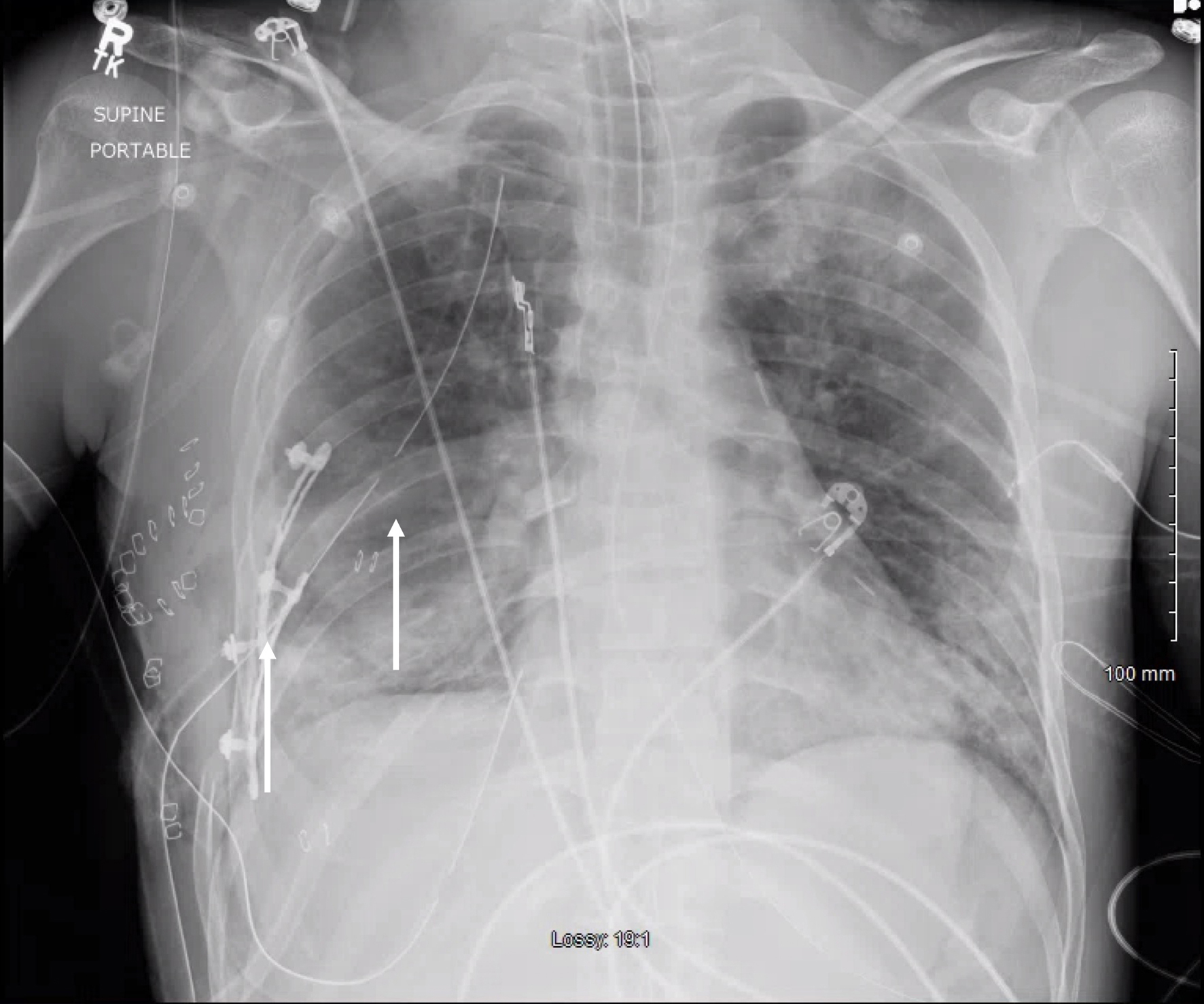 Click for large image | Figure 3. Radiographic image of the right fifth and sixth ribs plated using titanium RibFix bridge implanted intrathoracically along the posterior surface of the ribs. Lateral white arrow indicates the titanium RibFix bridge and the medial white arrow indicates the improved pleural effusion. |
On postoperative day 11, the patient became tachycardic and febrile with increasing leukocytosis. A CT scan was ordered due to concern for sepsis, which showed a loculated anterior right pleural fluid collection suspicious for loculated empyema secondary to infected hardware (Fig. 4a). Due to the patient showing signs of septic shock conservative management was initiated instead of operative treatment. A right-pigtail CT-guided chest tube with purulent output was placed in the right chest. Bacterial cultures were sent and noted to grow Acinetobacter baumannii which was sensitive to antibiotics. The pigtail output was sent for culture, and antibiotics were appropriately de-escalated to unα-syn. The patient was started on a 3-day course of tissue plasminogen activator (tPA) and DNase to treat his empyema. Three days later, on postoperative day 14, the patient was extubated, and on postoperative day 15, a repeat CT demonstrated significant improvement in the loculated empyema with evidence of abscess resolution (Fig. 4b). The patient was downgraded from the SICU on postoperative day 16. On postoperative day 20, the right pigtail was removed and the patient was discharged from the hospital. He followed up in the outpatient clinic after 2 weeks; he was saturating well on room air and had no issues performing any of his activities of daily living.
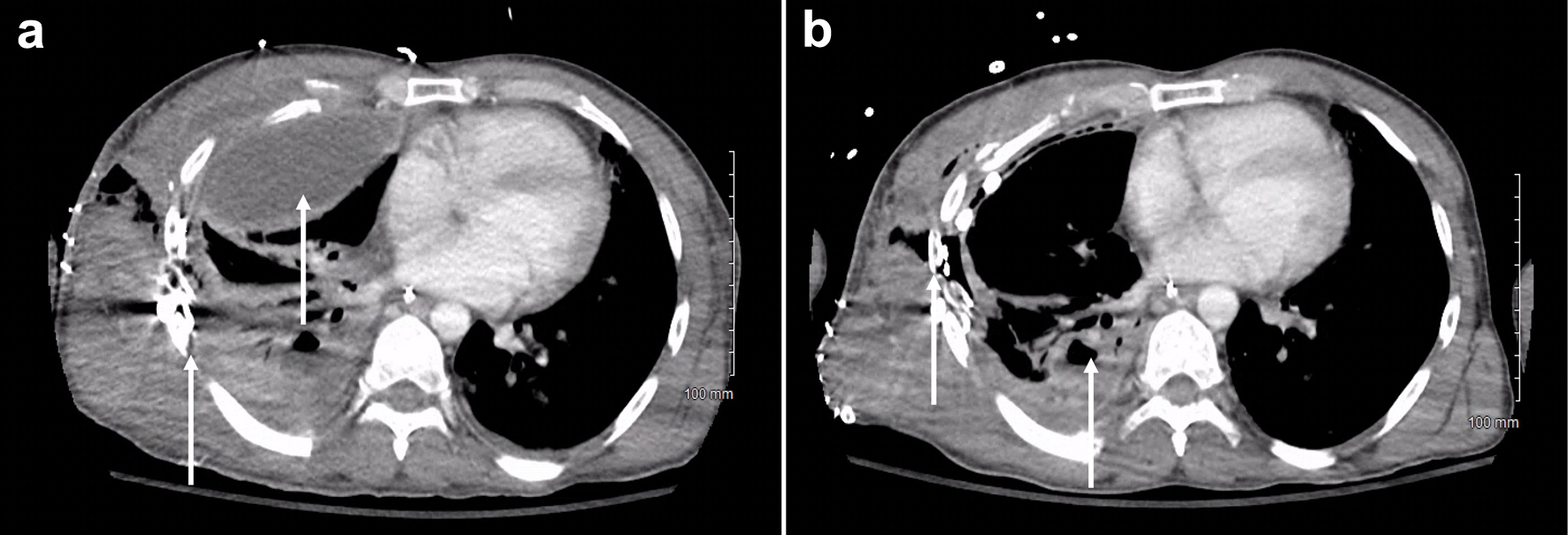 Click for large image | Figure 4. (a) Computed tomography with a loculated anterior right pleural fluid collection suspicious for loculated empyema secondary to infected hardware (indicated by the white arrow). (b) Significant improvement in the loculated empyema after treatment with tissue plasminogen activator (tPA) and DNase (indicated by the white arrow with only small residual effusion on the posterior). |
| Discussion | ▴Top |
We present a unique clinical finding of postoperative empyema after intrathoracic rib fixation to contribute to the growing information on outcomes after RFF. Empyema is an extremely rare complication of RFF [12]. In Table 1 [13-19], we summarize a variety of clinical cases from 2019 to 2023 to compare our literature findings on commonly reported outcomes of RFF. In agreement with the literature, most of these cases demonstrated an uncomplicated recovery period, and the most common postoperative complication was pneumonia (Table 1). Similarly, in a retrospective study of patients with flail chest or multiple rib fractures who underwent RFF, Beks et al found that the most common postoperative complications in both groups were pneumonia (39%, 32%), excess pleural fluid (4.5%, 3%), and implant-related infection (3%, 3%), and approximately 10% of patients removed hardware due to implant-related irritation [20].
 Click to view | Table 1. Literature Review of Case Reports on Complications Found in Patients With Rib Fracture Fixation |
Empyema remains an extremely rare outcome, with an incidence of hardware infection in less than 3% of patients [10]. In support of this claim, Mouton et al conducted a prospective follow-up study from 1990 to 1996 at a level-1 trauma center, and one patient developed postoperative empyema, pneumonia, ARDS, and multiorgan failure within a 3-week length of stay (LOS) [21]. Similarly, a prospective study at a university hospital compared conservative and surgical management of flail chests and only one patient with RFF developed empyema [22]. Additionally, Wijffels et al (2020) conducted a comparative study of 70 flail chest patients at a level-1 trauma center, and empyema was only found in the non-operative group [23]. To our knowledge, Fawzy et al (2022) are the most recent group to report a patient with RFF who developed empyema and was subsequently managed with antibiotics, drainage, and dornase alfa [13]. In 1975, Nirula et al reported that only 0.3% of RFFs had empyema [12]. There remains very little information about patients with empyema and RFF, especially fixation considered intrathoracic along the posterior surface of the ribs.
With regard to the outcomes of RFF versus nonsurgical intervention, various reported clinical cases show rib fixation as advantageous, with little to no postoperative complications in adults and children [13, 14, 24] (Table 1). Multiple studies have shown that patients who undergo surgical intervention in the form of fixation experience significantly fewer days on a ventilator, reduced pain, improved quality of life, and better respiratory function than those who only choose conservative measures [25-28]. In their retrospective analysis, Beks et al reported the long-term outcomes of 166 patients who underwent rib fixation and found that only one patient developed ARDS postoperatively [20]. Additionally, Gauger et al reported that most patients with RFF returned to their daily activities without limitations, and only one patient had a wound infection [29]. Galos et al stated that fixation has significant advantages such as improvement in quality of life, reduction in pain, and LOS [8]. This is supported by studies that showed a decrease in pain and usage of narcotic medication after RFF when compared to patients managed with conservative measures [28, 30-32]. Drahos et al supported a surgical approach for the treatment of rib fractures after reporting no long-term complications in their retrospective analysis of 156 patients between 2009 and 2017 [33].
Opposing arguments against RFF highlight the serious issues associated with RFF. Taghavi et al compared patients who had nonoperative and operative measures for rib fractures in 2016 through the National Trauma Data Bank and patients with RFF had a significantly longer duration of stay (13 vs. 5 days) and higher incidence of complications (40.6% vs. 19.5%), but interestingly, RFF showed a significantly lower mortality rate [34]. In a retrospective analysis, patients who received titanium plates for chest wall reconstruction had a variety of complications including infection, plate fracture, and impaired wound healing [35]. Similarly, Farquhar et al conducted a retrospective study and found no significant benefit of surgical fixation, and patients with flail chests who received that treatment had significantly higher rates of pneumonia [36].
A limitation of this study is that this is a case report and more research is needed on the different treatment methods for severe rib fractures, their outcomes, and complications. In our case, we successfully managed an empyema conservatively in a patient with RFF and, more importantly, a fixation where the plates were placed in an intrathoracic position. Although the trend for treating multiple rib fractures is towards the operative approach, there is a lack of data on rare outcomes, such as empyema. The possibility of conservative management in cases of empyema formation after rib fixation should be considered on a case-by-case basis.
Learning points
Blunt chest trauma is one of the most common etiologies of rib fractures, and 10% of patients with blunt chest trauma have rib fractures. Rib fractures are associated with various complications including, but not limited to, pneumothorax, hemothorax, pulmonary contusions, and respiratory failure requiring mechanical ventilation. Rib fractures can also be accompanied by significant pain, shortness of breath, and in more severe cases, empyema, pneumonia, and ARDS. There are a range of treatment modalities for rib fractures and sequelae, ranging from conservative medical management to invasive surgical treatments. As the application of rib plating increases, successfully identifying candidates for conservative management of rare complications, such as empyema, will be beneficial.
Acknowledgments
None to declare.
Financial Disclosure
The research presented in this manuscript had no specific funding from any agency in the public, commercial or not-for-profit sectors.
Conflict of Interest
The authors declare there is no conflict of interest.
Informed Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. Ethical approval was obtained from our institutional review board (IRB #23-22).
Author Contributions
Aldin Malkoc, Lana Mamoun, and Brandon Woodward: conceptualization, methodology, writing - original draft. Harpreet Gill, Amira Barmanwalla, Amanda Daoud, Alexander Phan, Kendall Vignaroli, and Alexandra Nguyen: writing - review and editing. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
ARDS: acute respiratory distress syndrome; CT: computed tomography; IV: intravenous; RFF: rib fracture fixation; SICU: surgical intensive care unit; tPA: tissue plasminogen activator
| References | ▴Top |
- Serfin J, Guo WA. Rib fractures. The American Association for the Surgery of Trauma. 2020. https://www.aast.org/resources-detail/rib-fractures#:∼:text=Approximately%2010%25%20of%20all%20patients,one%20or%20more%20rib%20fractures.
- Peek J, Beks RB, Hietbrink F, Heng M, De Jong MB, Beeres FJP, Leenen LPH, et al. Complications and outcome after rib fracture fixation: A systematic review. J Trauma Acute Care Surg. 2020;89(2):411-418.
doi pubmed - Peek J, Beks RB, Hietbrink F, De Jong MB, Heng M, Beeres FJP, FFA IJ, et al. Epidemiology and outcome of rib fractures: a nationwide study in the Netherlands. Eur J Trauma Emerg Surg. 2022;48(1):265-271.
doi pubmed pmc - Dehghan N, de Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76(2):462-468.
doi pubmed - Keen G. Chest injuries. Ann R Coll Surg Engl. 1974;54(3):124-131.
pubmed pmc - Marro A, Chan V, Haas B, Ditkofsky N. Blunt chest trauma: classification and management. Emerg Radiol. 2019;26(5):557-566.
doi pubmed - DiMaggio C, Ayoung-Chee P, Shinseki M, Wilson C, Marshall G, Lee DC, Wall S, et al. Traumatic injury in the United States: In-patient epidemiology 2000-2011. Injury. 2016;47(7):1393-1403.
doi pubmed pmc - Galos D, Taylor B, McLaurin T. Operative fixation of rib fractures indications, techniques, and outcomes. Bull Hosp Jt Dis (2013). 2017;75(1):15-20.
pubmed - Fowler TT, Taylor BC, Bellino MJ, Althausen PL. Surgical treatment of flail chest and rib fractures. J Am Acad Orthop Surg. 2014;22(12):751-760.
doi pubmed - Adereti C, Fabien J, Adereti J, Pierre-Louis M, Chacon D, Adereti V. Rib plating as an effective approach to managing traumatic rib injuries: a review of the literature. Cureus. 2022;14(9):e29664.
doi pubmed pmc - Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A, SCARE Group. The SCARE 2020 guideline: updating consensus surgical case report (SCARE) Guidelines. Int J Surg. 2020;84:226-230.
doi pubmed - Nirula R, Mayberry JC. Rib fracture fixation: controversies and technical challenges. Am Surg. 2010;76(8):793-802.
pubmed - Fawzy Y, Hindin D, Faliks B, Tung J, Forrester JD. Rib fracture fixation in a patient on veno-venous extracorporeal membrane oxygenation following a motor vehicle collision. Trauma Surg Acute Care Open. 2022;7(1):e001004.
doi pubmed pmc - Zhou XT, Zhang DS, Yang Y, Zhang GL, Xie ZX, Chen MH, Liang Z. Analysis of the advantages of 3D printing in the surgical treatment of multiple rib fractures: 5 cases report. J Cardiothorac Surg. 2019;14(1):105.
doi pubmed pmc - Abidali M, Faliks B, Najafi K, Bauer F. Chest wall stabilization in a patient with severe TBI: a case report. Int J Surg Case Rep. 2023;105:108095.
doi pubmed pmc - Allen R, Estroff J, Sarani B. Surgical stabilization of rib fractures in a patient with empyema: a case report. JBJS Case Connect. 2019;9(4):e0202.
doi pubmed - DeGenova DT, Schmitz NP, Lin JB, Jones TJ, Taylor BC. Outpatient Surgery for Rib Fracture Fixation: A Report of Three Cases. Cureus. 2022;14(11):e31890.
doi pubmed pmc - Stefani A, Tormen F, Scamporlino A, Natali P, Cavallesco G, Morandi U. Surgical stabilization of severe flail chest with Judet and Sanchez-Lloret plates. A case report. Int J Surg Case Rep. 2021;81:105805.
doi pubmed pmc - Whittaker D, Edmunds C, Scott I, Khalil M, Stevenson I. Rib fracture fixation in a patient on veno-venous ECMO for severe blunt thoracic trauma. Ann R Coll Surg Engl. 2021;103(9):e269-e271.
doi pubmed pmc - Beks RB, de Jong MB, Houwert RM, Sweet AAR, De Bruin I, Govaert GAM, Wessem KJP, et al. Long-term follow-up after rib fixation for flail chest and multiple rib fractures. Eur J Trauma Emerg Surg. 2019;45(4):645-654.
doi pubmed pmc - Mouton W, Lardinois D, Furrer M, Regli B, Ris HB. Long-term follow-up of patients with operative stabilisation of a flail chest. Thorac Cardiovasc Surg. 1997;45(5):242-244.
doi pubmed - Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4(6):583-587.
doi pubmed - Wijffels MME, Hagenaars T, Latifi D, Van Lieshout EMM, Verhofstad MHJ. Early results after operatively versus non-operatively treated flail chest: a retrospective study focusing on outcome and complications. Eur J Trauma Emerg Surg. 2020;46(3):539-547.
doi pubmed pmc - Leenstra BS, Stolwijk A, Poeze M. Surgical stabilisation in a 13-year-old boy with traumatic flail chest. BMJ Case Rep. 2015;2015:bcr2015209371.
doi pubmed pmc - Farley P, Mullen PR, Taylor CN, Lee YL, Butts CC, Simmons JD, Brevard SB, et al. The treatment of rib fractures: a single-center comparison. Am Surg. 2020;86(9):1144-1147.
doi pubmed - Doben AR, Eriksson EA, Denlinger CE, Leon SM, Couillard DJ, Fakhry SM, Minshall CT. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care. 2014;29(1):139-143.
doi pubmed - Girsowicz E, Falcoz PE, Santelmo N, Massard G. Does surgical stabilization improve outcomes in patients with isolated multiple distracted and painful non-flail rib fractures? Interact Cardiovasc Thorac Surg. 2012;14(3):312-315.
doi pubmed pmc - Khandelwal G, Mathur RK, Shukla S, Maheshwari A. A prospective single center study to assess the impact of surgical stabilization in patients with rib fracture. Int J Surg. 2011;9(6):478-481.
doi pubmed - Gauger EM, Hill BW, Lafferty PM, Cole PA. Outcomes after operative management of symptomatic rib nonunion. J Orthop Trauma. 2015;29(6):283-289.
doi pubmed - Van Wijck SFM, Van Lieshout EMM, Prins JTH, Verhofstad MHJ, Van Huijstee PJ, Vermeulen J, Wijffels MME. Outcome after surgical stabilization of symptomatic rib fracture nonunion: a multicenter retrospective case series. Eur J Trauma Emerg Surg. 2022;48(4):2783-2793.
doi pubmed pmc - DeGenova DT, Miller KB, McClure TT, Schuette HB, French BG, Taylor BC. Operative fixation of rib fracture nonunions. Arch Orthop Trauma Surg. 2023;143(6):3047-3054.
doi pubmed - Hori S, Miyahara N, Hiratsuka M. [Fixation of flail chest with bioabsorbable plate]. Kyobu Geka. 2022;75(8):602-605.
pubmed - Drahos A, Nowack T, Fitzgerald M, Christie DB. Longterm postoperative hardware complications after open rib fixation. Am Surg. 2018;84(8):e317-e319.
pubmed - Taghavi S, Ali A, Green E, Schmitt K, Jackson-Weaver O, Tatum D, Harris C, et al. Surgical stabilization of rib fractures is associated with improved survival but increased acute respiratory distress syndrome. Surgery. 2021;169(6):1525-1531.
doi pubmed pmc - Bergovec M, Smolle M, Lindenmann J, Fediuk M, Leithner A, Smolle-Juttner FM. High complication rate with titanium plates for chest wall reconstruction following tumour resection. Eur J Cardiothorac Surg. 2022;62(6):ezac534.
doi pubmed - Farquhar J, Almarhabi Y, Slobogean G, Slobogean B, Garraway N, Simons RK, Hameed SM. No benefit to surgical fixation of flail chest injuries compared with modern comprehensive management: results of a retrospective cohort study. Can J Surg. 2016;59(5):299-303.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


