| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 10, October 2024, pages 257-260
Navigating a Complex Case of Hypoplastic Right Lung With Bronchiectasis: A Ten-Year Journey
Muhammad Umer Riaz Gondala, g , Grant Gillespieb, Fawwad Ansaric, Swarup Sharma Rijala, Zainab Kiyanid, Ayushi Lalwania, Toqeer Khane, Syed Ayan Zulfiqar Bokharif, Ayushma Acharyaa, Ryan Zimmermana
aDepartment of Internal Medicine, Tower Health, Reading Hospital, West Reading, PA, USA
bDepartment of Internal Medicine, Drexel University, West Reading, PA, USA
cDepartment of Internal Medicine, Piedmont Athens Regional, Athens, USA
dDepartment of Internal Medicine, Islamabad Medical and Dental College, Islamabad, Pakistan
eDepartment of Internal Medicine, Lincoln Medical Center, New York, NY, USA
fDepartment of Internal Medicine, Foundation University, Islamabad, Pakistan
gCorresponding Author: Muhammad Umer Riaz Gondal, Department of Internal Medicine, Tower Health, Reading Hospital, West Reading, PA, USA
Manuscript submitted June 30, 2024, accepted August 14, 2024, published online September 20, 2024
Short title: Hypoplastic Right Lung
doi: https://doi.org/10.14740/jmc4283
| Abstract | ▴Top |
Unilateral pulmonary hypoplasia (UPH) is a rare congenital disorder that presents rarely in adulthood. Most patients succumb to complications at a young age, and those who survive are rare and susceptible to frequent lifelong pulmonary infections. It has a high infant mortality rate. We present the case of a 66-year-old male with rheumatoid arthritis and severe persistent asthma who first presented to our emergency department in 2013 with worsening shortness of breath. Chest imaging with a computed tomography (CT) scan revealed right hemithorax volume loss with hypoplasia, honeycomb lung formation, and right mediastinal shift. He was treated with prednisone, inhalers, and antibiotics for asthmatic bronchitis. He continued to suffer frequent hospital admissions (56 to our hospital alone) over the next decade for pneumonia and asthma exacerbations. The hypoplastic right lung was deemed to be contributing to recurrent infections/inflammation, and he is currently being re-evaluated for a right pneumonectomy, as surgical resection is an option for localized bronchiectasis associated with recurrent respiratory infections.
Keywords: Unilateral pulmonary hypoplasia; Bronchiectasis; Asthma; Pneumonia; Pneumonectomy
| Introduction | ▴Top |
Pulmonary hypoplasia is a rare congenital anomaly characterized by incomplete development of lung tissue. Incomplete lung tissue anomalies are classified as agenesis, aplasia, or hypoplasia. Agenesis defines the complete absence of the lung bronchus and pulmonary artery. Aplasia establishes the presence of a rudimentary bronchus with the absence of the pulmonary artery and lung tissue. The final category, hypoplasia, defines the underdevelopment of the pulmonary artery and bronchus with varying degrees of distal lung tissue present [1].
The incidence of pulmonary hypoplasia is estimated to be 1 in 1,000 live births. However, this figure likely underestimates the true incidence as patients with mild forms of this disease may be asymptomatic and, therefore, go undetected during the neonatal period [2]. Unilateral lung hypoplasia results in high rates of infant mortality, as much as 50%, often secondary to concurrent anomalies, and bilateral lung hypoplasia is not compatible with life [3]. As a result, pulmonary hypoplasia in adulthood is rare.
We report a case of unilateral pulmonary hypoplasia (UPH) in an elderly patient who, unfortunately, suffered from numerous pulmonary complications severely impacting his quality of life.
| Case Report | ▴Top |
A 66-year-old man with rheumatoid arthritis on prednisone and severe persistent asthma first presented to our emergency department in 2013 with worsening shortness of breath and cough. History revealed recurrent respiratory infections in childhood. The patient stated he was born with a right lung hypoplasia. He had worked as a contractor, had just recently retired, and moved from a different state into this area.
Blood pressure was 110/70 mm Hg, heart rate 78 beats per minute (bpm), afebrile and saturating 97% on room air. Physical examination revealed scattered rales and rhonchi persisting throughout the right lung. Blood work showed a white blood cell (WBC) count of 13.7 × 103/µL) and C-reactive protein (CRP) of 1.51 (mg/dL). Troponin, lactic acid, procalcitonin, and B-type natriuretic peptide (BNP) were within normal limits. Chest X-ray revealed a rightward mediastinal shift, with volume loss and reticular opacities throughout the right lung. Computed tomography (CT) scan of the chest revealed volume loss of the right hemithorax with hypoplasia, parenchymal scarring, honeycomb lung formation, right mediastinal shift, and compensatory left lung hyperinflation (Fig. 1).
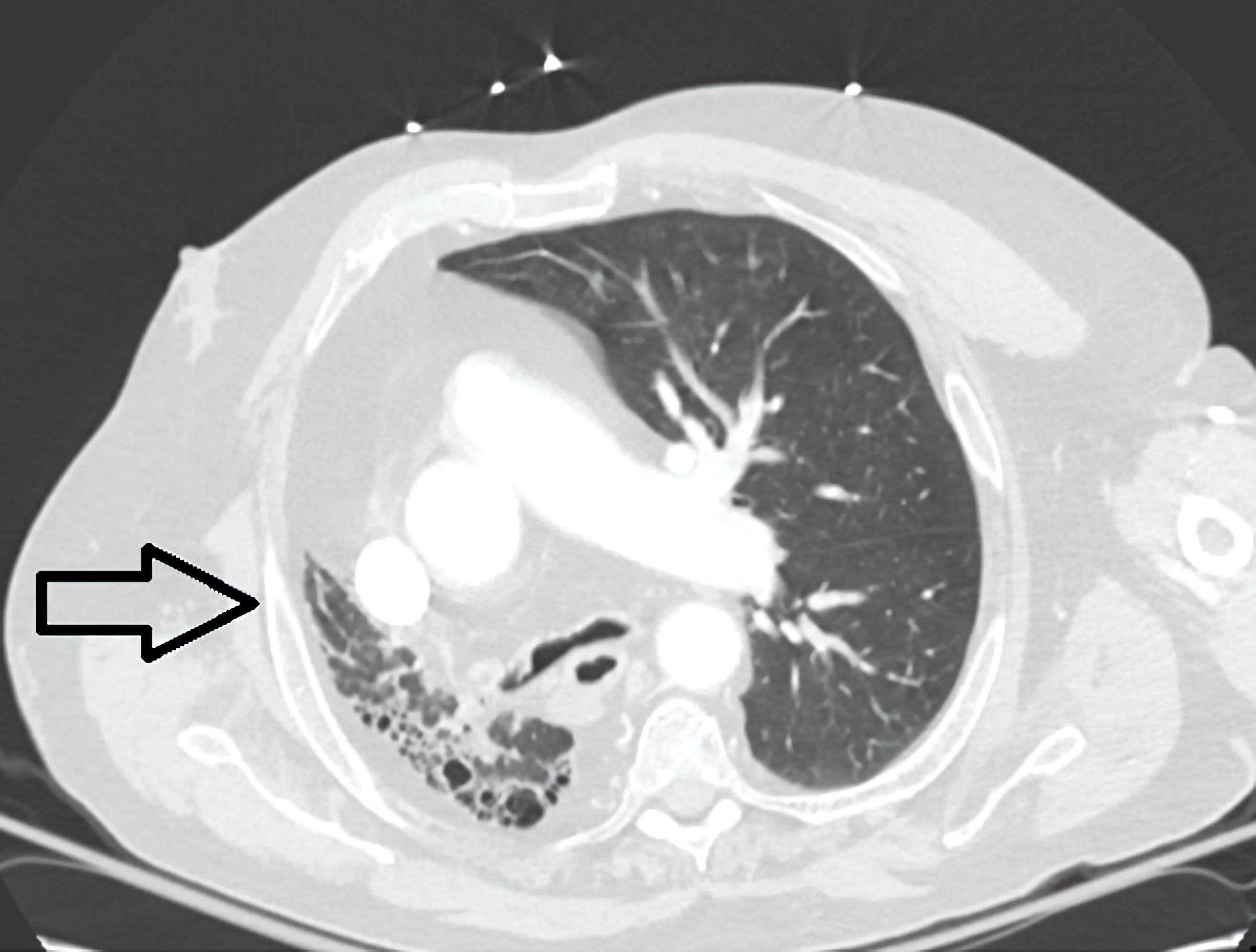 Click for large image | Figure 1. Computed tomography (CT) scan showing volume loss of the right hemithorax with hypoplasia, parenchymal scarring, honeycomb lung formation, right mediastinal shift, and compensatory left lung hyperinflation (arrow). |
A sputum sample did not reveal any bacteria. He was treated for asthmatic bronchitis with prednisone, short-acting beta-agonist/muscarinic antagonist inhalers, and moxifloxacin and discharged home.
His past medical history was reviewed from records at an outside hospital at that time. Pulmonology notes revealed that the patient had been on inhalers for his severe asthma. He had been hospitalized before at an outside hospital for pneumonia and asthma exacerbations. Imaging revealed right lung hypoplasia and bronchiectasis changes, which were attributed to congenital unilateral hypoplasia. He had been advised to get a right pneumonectomy to decrease frequent exacerbations; however, the patient had declined at the time due to elevated surgical risk.
Outpatient management included rescue inhalers, long-acting beta-agonists, inhaled corticosteroids, oral corticosteroids, and omalizumab. He continued to suffer frequent hospital admissions (56 to our hospital alone) over the next decade for pneumonia and asthma exacerbations. The patient had frequent cases of pneumonia due to Pseudomonas aeruginosa (pansensitive) and was trialed on tobramycin inhalers for a few months, followed by doxycycline suppressive therapy as prophylaxis.
The patient has been seen in our office regularly over the years. His pulmonary function tests revealed moderate obstruction on spirometry (Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2), no bronchodilator response, and mild restrictive lung volumes: forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) 61%, FEV1 53% (actual 1.50, predicted 2.82), FVC 63% (actual 2.46, predicted 3.91), and diffusing capacity of the lungs for carbon monoxide (DLCO) 65% predicted. He was on chronic oral prednisone for long periods for his severe asthma and frequent exacerbations and bronchiectasis.
The hypoplastic right lung was deemed to be contributing to recurrent infections/inflammation, and he is currently being re-evaluated for a right pneumonectomy at an advanced medical center. He is presently on dupilumab for his severe asthma, which has significantly improved his symptoms.
The patient continues to follow up with our office. His asthma is under better control, and he has had no further hospital admissions.
| Discussion | ▴Top |
UPH is a rare congenital disorder rarely seen in adulthood. A decrease in the number or size of airways, vessels, and alveoli characterizes it. Most patients succumb to complications at a young age, and those who survive are rare and susceptible to frequent lifelong pulmonary infections.
The pathogenesis of pulmonary hypoplasia is broad and can be divided into primary and secondary hypoplasia. Primary hypoplasia has no identifiable cause. In contrast, secondary pulmonary hypoplasia can be attributed to a known maternal-fetal abnormality that impedes normal lung development, such as chest wall deformities, space-occupying lesions, diaphragmatic hernias, or neuromuscular disorders. Prolonged preterm rupture of membranes or urogenital abnormalities resulting in oligohydramnios may also lead to secondary hypoplasia [4]. Lung agenesis may also present with vertebral, anorectal, cardiac, tracheoesophageal, renal, and limb anomalies (VACTERL association) [5].
During the neonatal period, the presentation of UPH is variable and depends on the extent of hypoplasia. Neonates with severe disease may initially have respiratory distress and require endotracheal intubation. Others may have normal APGAR (appearance, pulse, grimace, activity, and respiration) scores at birth and may continue to be asymptomatic, in which pulmonary hypoplasia is diagnosed later in childhood or even as an adult, as seen with our patient [6]. In some adults, UPH may be asymptomatic and be diagnosed incidentally based on imaging done for other reasons [7]. Symptomatic adults may suffer from chronic cough, dyspnea, and recurrent lower respiratory tract infections. Blind-ending bronchi and dysfunctional mucociliary clearance lead to the pooling of secretions and are thought to contribute to increased susceptibility to infections in patients with pulmonary hypoplasia [4, 8].
Chest X-ray is often the initial imaging study of choice for patients with nonspecific respiratory complaints. However, diagnosis of pulmonary hypoplasia with chest X-ray is difficult, as X-ray findings may be mistaken for other respiratory pathologies, including lobar collapse, pleural effusion, hydatid disease, or post-tuberculosis lung disease, and lead to misdiagnosis. As a result, contrast-enhanced CT is the preferred imaging modality for diagnosing pulmonary hypoplasia [7]. CT imaging will show volume loss on the affected side with compensatory hyperinflation of the contralateral lung and mediastinal shift towards the affected side. The herniation of abdominal organs into the affected hemithorax was also observed. Additional studies such as bronchoscopy, bronchography, magnetic resonance imaging (MRI), and ventilation-perfusion scintigraphy can also play a role in disease evaluation [9].
In fetuses with pulmonary hypoplasia, interventions can be done prenatally. After delivery, cases that require surgical intervention are significant cystic lung malformations and congenital diaphragmatic hernias.
Management of adults with UPH is conservative, and asymptomatic patients may be observed without additional medical therapy for pulmonary hypoplasia. Patients such as the one in this case who have dyspnea or recurrent infections should be treated symptomatically. Dyspnea, secondary to obstructive disease, may be treated with bronchodilators, steroids, or biologic agents to improve pulmonary function. Patients with recurrent infections should be managed with regular vaccination against respiratory pathogens and appropriate antibiotics. Surgical resection of hypoplastic lung tissue has also been used to treat symptoms of chronic infections [4, 8, 9]. Another essential treatment modality is airway clearance with patients undergoing pulmonary rehabilitation and getting regular exercise. Mechanical modes of airway clearance include chest physiotherapy with postural drainage, autogenic drainage, active cycle of breathing techniques, and huff/forced cough maneuvers. Airway clearance can also be augmented using devices such as oscillating positive expiratory pressure (PEP) devices and high-frequency chest wall oscillatory “vests”. Although little scientific evidence supports their routine use, pharmacologic therapies are also available to improve mucociliary transport [10].
Our patient received long-term inhaled corticosteroid and beta-agonist inhalers, remained on chronic steroids for many years, was trialed on antibiotic suppressive therapy for frequent Pseudomonas infections, and received biologic treatment for his severe asthma.
A case report by Ramesh et al [11] described a 72-year-old male with a history of right lung hypoplasia and pulmonary artery agenesis, with a history of lifelong pulmonary infections, similar to our patient. His condition was complicated by Aspergillus infection and thus underwent a right pneumonectomy with intraoperative findings revealing extensive cystic disease with purulence. The authors described their case to be one of the oldest reported to have undergone definitive surgical resection for their hypoplastic lung [11].
In adults, surgical resection is indicated in cases of severe cystic changes and intense symptomatology. There are no clear guidelines about the role of surgical resection in adults with UPH. While older age is generally thought to be a risk factor for postoperative morbidity and mortality, studies have suggested that age itself should not be a contraindication for pneumonectomy. Instead, they should be one component of a comprehensive risk-assessment approach [10].
Conclusions
This case report identified clinical gaps in the care and management of a patient with UPH. Based on our patient experience, clinicians should counsel patients on the risk of frequent exacerbations. Optimal medical management is crucial, and surgical resection should be offered for those with frequent complications. The role of surgical intervention should be clearly defined in universal guidelines, which requires further research.
Learning points
UPH is a rare congenital disorder with a high infant mortality rate. Thus, adult survivors are rare and suffer from a lifetime of frequent pulmonary infections. Surgical resection is recommended in patients with severe symptoms.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Patient consent has been obtained.
Author Contributions
Muhammad Umer Riaz Gondal: writing - original draft and writing - review and editing, conceptualization, data curation, formal analysis, and investigation. Grant Gillespie: writing - review and editing and conceptualization. Fawwad Ansari: writing - review and editing, and conceptualization. Zainab Kiyani: writing - review and editing, and conceptualization. Ayushi Lalwani: writing - review and editing, and conceptualization. Toqeer Khan: writing - review and editing, and conceptualization. Swarup Sharma Rijal: supervision, validation, and visualization. Syed Ayan Zulfiqar Bokhari: writing - review and editing, and conceptualization. Ryan Zimmerman: supervision, validation, and visualization. Ayushma Acharya: review, editing, and conceptualization.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Boyden EA. Developmental anomalies of the lungs. Am J Surg. 1955;89(1):79-89.
doi pubmed - Knox WF, Barson AJ. Pulmonary hypoplasia in a regional perinatal unit. Early Hum Dev. 1986;14(1):33-42.
doi pubmed - Thacker PG, Rao AG, Hill JG, Lee EY. Congenital lung anomalies in children and adults: current concepts and imaging findings. Radiol Clin North Am. 2014;52(1):155-181.
doi pubmed - Kurkcuoglu IC, Eroglu A, Karaoglanoglu N, Polat P. Pulmonary hypoplasia in a 52-year-old woman. Ann Thorac Surg. 2005;79(2):689-691.
doi pubmed - Knowles S, Thomas RM, Lindenbaum RH, Keeling JW, Winter RM. Pulmonary agenesis as part of the VACTERL sequence. Arch Dis Child. 1988;63(7 Spec No):723-726.
doi pubmed pmc - Pathania M, Lali BS, Rathaur VK. Unilateral pulmonary hypoplasia: a rare clinical presentation. BMJ Case Rep. 2013;2013:bcr2012008098.
doi pubmed pmc - Komolafe F, Dahniya MH, Al-Ali Y, Al-Zaabi L, Aziz F. Asymptomatic unilateral pulmonary hypoplasia/ agenesis in adults: a report of six cases. West Afr J Radiol. 2017;24:99-103.
- Papadopoulos D, Misthos P, Chorti M, Skopas V, Nakou A, Karagianidis N, Lioulias A, et al. Unilateral pulmonary hypoplasia in an adult patient. Monaldi Arch Chest Dis. 2018;88(1):829.
doi pubmed - Cherian SV, Kumar A, Ocazionez D, Estrada YMRM, Restrepo CS. Developmental lung anomalies in adults: A pictorial review. Respir Med. 2019;155:86-96.
doi pubmed - O'Donnell AE. Medical management of bronchiectasis. J Thorac Dis. 2018;10(Suppl 28):S3428-S3435.
doi pubmed pmc - Ramesh N, Velotta JB. Pneumonectomy in an elderly patient with congenital unilateral lung hypoplasia and recurrent Aspergillus: a case report. AME Case Rep. 2023;7:9.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


