| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 10, October 2024, pages 283-286
Orogastric Tube Fracture and Ingestion in a Patient With Hyperacute Delirium: A Unique and Potentially Catastrophic Complication
Lefika Bathobakaea, e , Shaimaa Elshaarawya, Rammy Bashirb, Phenyo Phuuc, Gabriel Melkid, Bassam Hajjard
aInternal Medicine, St. Joseph’s University Medical Center, Paterson, NJ, USA
bInternal Medicine, Norwalk Hospital/Yale University, Norwalk, CT, USA
cInternal Medicine, St. Vincent’s Medical Center, Bridgeport, CT, USA
dGastroenterology and Hepatology, St. Joseph’s University Medical Center, Paterson, NJ, USA
eCorresponding Author: Lefika Bathobakae, Internal Medicine, St. Joseph’s University Medical Center, Paterson, NJ 07503, USA
Manuscript submitted July 11, 2024, accepted August 27, 2024, published online September 20, 2024
Short title: OGTs Fracture and Ingestion
doi: https://doi.org/10.14740/jmc4295
| Abstract | ▴Top |
Orogastric tubes (OGTs) are frequently used to administer feeds and medications to critically ill patients. They are inserted blindly, with a low first-pass success rate and frequent benign complications. OGT fractures and ingestion are exceedingly rare, with only two cases reported to date. Herein, we describe a rare case of OGT transection and ingestion in a male patient admitted for hyperacute delirium and complicated pneumonia. The OGT remnant was retrieved using an endoscope without any complications. Clinicians must be aware of this rare but potentially catastrophic complication of OGT use. OGTs must be inspected in the same manner as endotracheal tubes to ensure patient safety.
Keywords: Enteral feeding; Orogastric tube; Orogastric tube fracture; Foreign body; Endoscopic foreign body removal; Hyperacute delirium
| Introduction | ▴Top |
Feeding tubes are commonly used in emergencies, anesthesia, and critical care for the administration of feeds, medications, gastric lavage, or gastric decompression [1-6]. Blind orogastric tube (OGT) insertion is routinely performed in medical care and is associated with a low first-pass success rate and frequent benign complications [7-9]. OGT fracture and ingestion is an extremely rare event, and only two other cases have been reported to date [1, 10]. Poor storage, stomach acidity, or aggressive flushing of impacted food residue can affect the structural integrity of an OGT [1]. Herein, we report a unique case of OGT fracture and ingestion in a male patient with a history of hepatitis C and polysubstance use disorder. The OGT was successfully retrieved using an endoscopic snare. To the best of our knowledge, this is the first reported case of OGT transection and ingestion retrieved using an endoscopically.
| Case Report | ▴Top |
A 34-year-old male with a medical history of chronic hepatitis C and polysubstance use disorder presented to our emergency room (ER) for evaluation of shortness of breath and productive cough. The patient reported using crack cocaine a few hours before the ER visit and was anxious about a potential withdrawal from heroin use. In the ER, he was febrile and tachypneic and required oxygen therapy via a nasal cannula. The initial chest X-ray showed a right-sided loculated pleural effusion suggestive of complicated pneumonia. While still in the ER, the patient experienced hyperacute delirium, warranting endotracheal intubation for airway protection, and was admitted to the medical intensive care unit (ICU).
Triage bloodwork was significant for leukocytosis and hypomagnesemia, and the urine drug screen was positive for cocaine. The rest of the laboratory values, including hemoglobin level, serum electrolytes, creatine kinase, and B-type natriuretic peptide, were unremarkable. The patient was started on broad-spectrum antibiotics with vancomycin and piperacillin-tazobactam, and a chest tube was placed to evacuate the empyema. Eventually, the patient underwent right-sided video-assisted thoracoscopic surgery (VATS), which was converted to open thoracotomy. The surgeons performed decortication of the right lung and chest wall, resection of the right middle and lower wedges, and cryoablation of the intercostal nerves. Two test tubes were placed postoperatively, and the antibiotics were narrowed to ceftriaxone as the sputum culture grew Klebsiella pneumoniae. The sputum pneumonia panel tested positive for Klebsiella pneumoniae and Haemophilus influenzae.
On postoperative day 1, the patient became agitated, and a midazolam infusion was initiated for agitation. Later in the day, a nurse tried to replace the OGT (16 French Covidien Salem Sump Dual Lumen Stomach Tube) but noticed that it was shorter than usual. A chest X-ray showed an OGT terminating within the mid-esophagus (Fig. 1). A relook chest X-ray showed that the distal remnant of the OGT had advanced into the stomach. It was thought that the patient bit on the OGT while agitated and severed it.
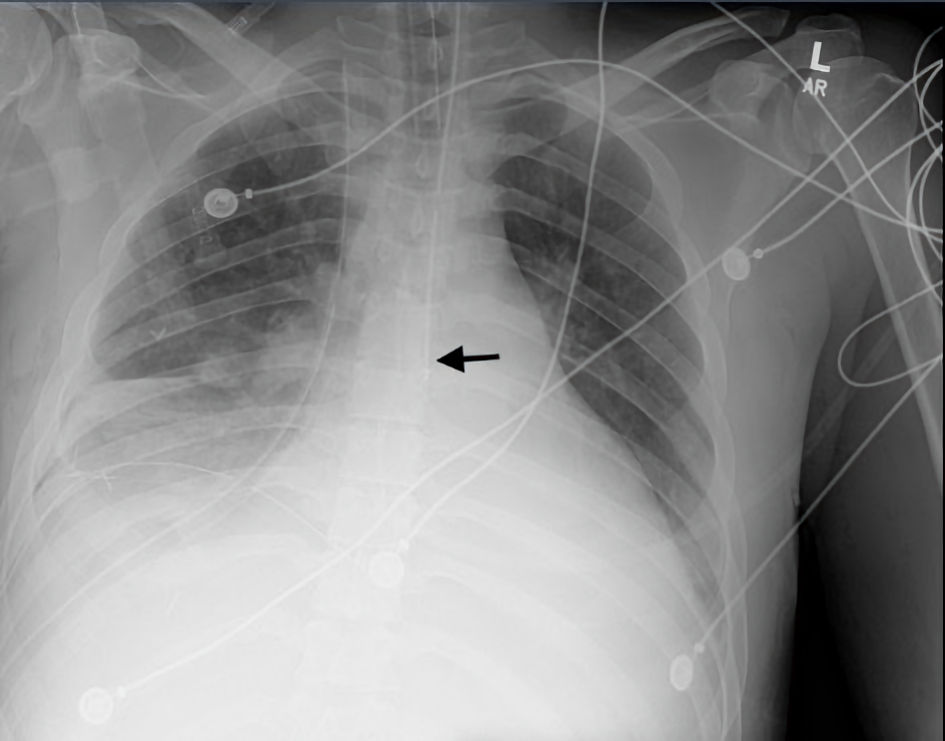 Click for large image | Figure 1. Frontal chest X-ray showing life support and monitoring devices: an orogastric tube terminates within the mid-esophagus (black arrow). |
Given that the OGT remnant had already advanced into the stomach, glucagon was not used for foreign body retrieval in this case. Upper endoscopy showed a broken OGT piece in the gastric body and antrum, extending into the esophagus (Fig. 2). The OGT remnant was retrieved using an endoscopic snare. The patient was successfully extubated on postoperative day 6, optimized on regular medical floors, and later discharged to a rehabilitation facility. The patient was seen in the cardiothoracic clinic 2 weeks later, and he had no acute complaints.
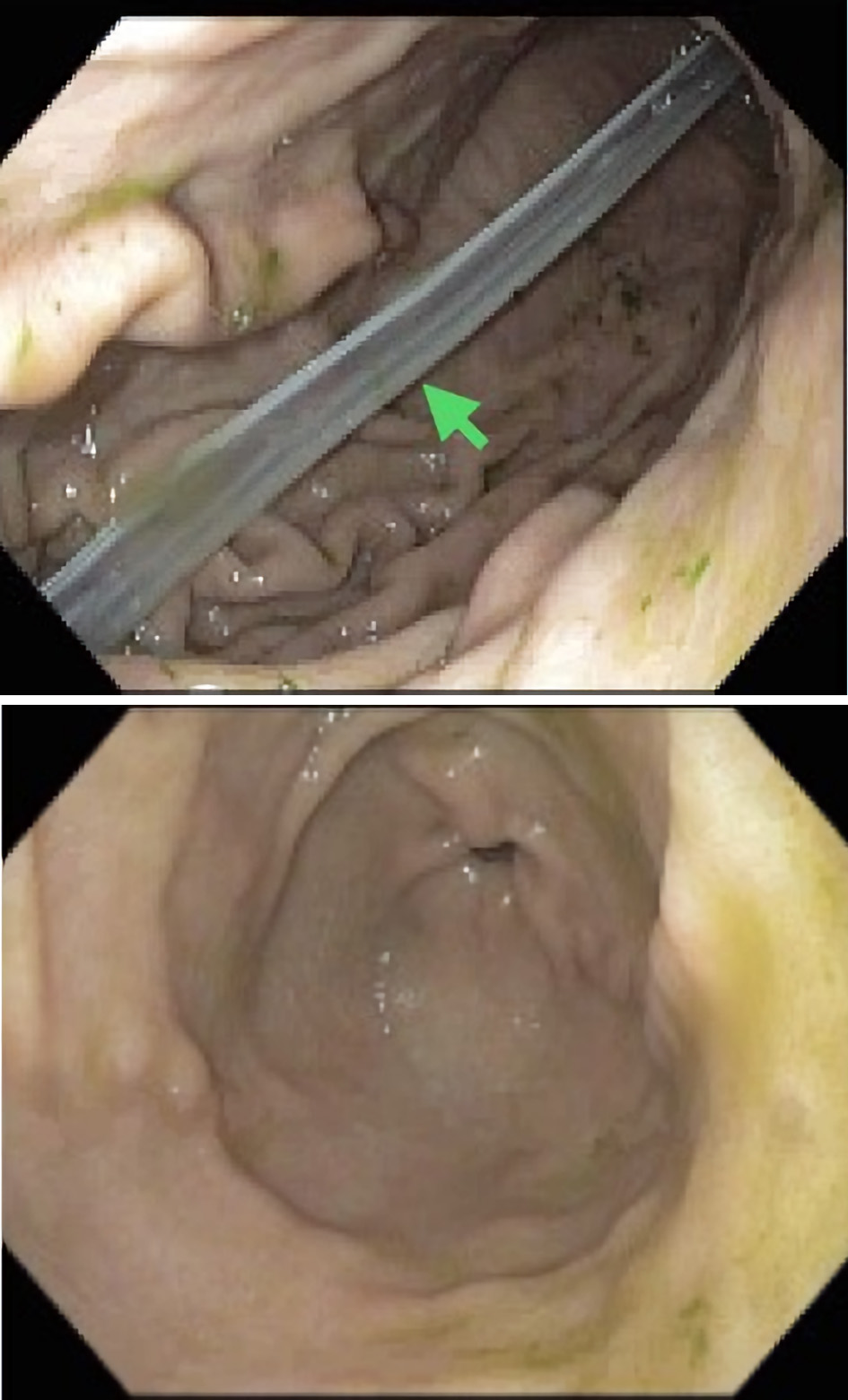 Click for large image | Figure 2. An endoscopic view shows a remnant of the orogastric tube in the gastric body (green arrow). The esophagus, pylorus, and duodenum were normal. |
| Discussion | ▴Top |
Defined as tubes inserted through the oral cavity into the stomach, OGTs have wide-ranging applications in critical care settings. The choice of OGT size is vital and often depends on patient-specific factors and the intended use. OGTs are commonly used for enteral feeding and to administer medications [4]. The insertion of OGTs is a common procedure in clinical practice, but it is not without risks. Most complications are benign and include esophageal mucosal irritation, tube clogging, kinking, knotting, and misplacement [1, 2, 8]. Flushing the OGT before and after use or using an OGT guide during insertion can minimize some of these complications [1, 7, 8]. Esophageal perforation, pneumothorax, bronchopleural fistula, cranial intubation, endotracheal tube obstruction or entanglement, and OGT stapling during sleeve gastrectomy are less common but serious complications of OGT use [2-4, 6, 8, 11-14].
To date, only two cases of OGT fracture and swallowing have been reported in the literature [1, 10]. In a case reported by Ranier et al, the patient coughed up the broken piece of the OGT while in the post-anesthesia care unit [9, 10]. In the second case, a laryngoscope was used for retrieval given the patient’s impaired swallowing mechanism in the setting of a recent stroke [1]. To the best of our knowledge, this is the first documented case in which an endoscope was used to retrieve the swallowed OGT remnant. Clinicians must be aware of this rare but potentially catastrophic complication of OGT use. To ensure patient safety, OGTs must be inspected after removal in the same fashion as the central lines and endotracheal tubes.
Fractured OGTs are incidentally detected during exchanges or routine care. Depending on the location of the displaced piece, patients can develop a cough, emesis, oropharyngeal irritation, or acute hypoxic respiratory failure [1, 8, 15]. In the case of upper aerodigestive tract perforation, patients may experience subcutaneous emphysema, odynophagia, hoarseness, or chest tightness [16]. Prompt surgical intervention is imperative to prevent life-threatening consequences. When OGT displacement or malfunction is suspected, a chest radiograph or CT scan can be performed to confirm positioning. The radiolucent nature of the OGT makes it difficult to visualize and ascertain its exact location within the esophagus [17]. As a result, transected distal remnants are most likely to be missed on imaging, predisposing patients to more complications [17]. In any case, chest radiographs remain the most accurate test for confirming OGT or nasogastric tube (NGT) positioning after insertion [18, 19].
Although soft and pliable, OGTs have a rigid and pointed end that can cause esophageal or gastric irritation or even perforation. Swallowed OGT remnants are managed as foreign bodies with emergent endoscopy as per the American Society for Gastrointestinal Endoscopy (ASGE) and European Society of Gastrointestinal Endoscopy (ESGE) clinical guidelines [1, 20, 21]. This is the first documented case of OGT transection and ingestion successfully retrieved using an endoscope.
OGT fractures and ingestions are extremely rare, with only two cases reported to date. This case report presents a rare instance of OGT transection and ingestion in a patient with hyperactive delirium and complicated pneumonia, which was successfully retrieved endoscopically. We aim to highlight the importance of inspecting feeding tubes in the same fashion as endotracheal tubes to ensure patient safety.
Learning points
Feeding tubes are routinely used in emergency situations, anesthesia, and critical care to administer feeds and medications. OGT insertion is performed blindly and can cause mild complications such as oropharyngeal irritation. OGT fractures and ingestion are extremely rare, with only two other cases documented in the literature. However, this is the first case where an endoscopic snare was used to retrieve a swallowed OGT remnant. Although rare, clinicians must be aware of this potential complication as it can have catastrophic implications.
Acknowledgments
We are grateful to the patient for allowing us to share this interesting case report with the rest of the medical community.
Financial Disclosure
No funding was obtained for the writing or submission of this case report.
Conflict of Interest
There is no conflict of interest to declare.
Informed Consent
The patient consented to the publication of this case report.
Author Contributions
LB conceptualized the idea of this case report. SE, RB, and PP helped with data curation, collection of pertinent patient information, and writing of the case report. GM and BH edited, fact-checked, and proofread the final version of the case report.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
OGT: orogastric tube; ER: emergency room; ICU: intensive care unit; VATS: video-assisted thoracoscopic surgery; NGT: nasogastric tube; ASGE: American Society for Gastrointestinal Endoscopy; ESGE: European Society of Gastrointestinal Endoscopy
| References | ▴Top |
- Khanal S, Shrestha S, Khadayat R, Adhikari A, Poddar E, Kharel S, Regmi PR. Breakage of an orogastric tube in a critically ill patient: a case report. Ann Med Surg (Lond). 2023;85(7):3714-3716.
doi pubmed pmc - Subedi Y, Adhikari B, Pokharel A, Poudel K, Sharma S. A case report of esophageal perforation: complications of orogastric tube placement. Cureus. 2023;15(1):e33535.
doi pubmed pmc - Jain S, Baksi A, Kumar A, Aggarwal S. Inclusion of orogastric tube in the staple line during laparoscopic Roux-en-Y gastric bypass: an avoidable complication. Obes Surg. 2021;31(6):2835-2836.
doi pubmed - O'Connell F, Ong J, Donelan C, Pourmand A. Emergency department approach to gastric tube complications and review of the literature. Am J Emerg Med. 2021;39:259.e255-259.e257.
doi pubmed - Higa G, Szomstein S, Rosenthal R. Stapling of orogastric tube during gastrojejunal anastomosis: an unusual complication after conversion of sleeve gastrectomy to laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2012;8(1):116-118.
doi pubmed - Calikoglu I, Ozgen G, Yerdel MA. Inadvertent stapling of the orogastric tube during bariatric surgery: Report of 3 cases and a systematic review. Medicine (Baltimore). 2021;100(2):e24144.
doi pubmed pmc - Alflen C, Kriege M, Schmidtmann I, Noppens RR, Piepho T. Orogastric tube insertion using the new gastric tube guide: first experiences from a manikin study. BMC Anesthesiol. 2017;17(1):54.
doi pubmed pmc - Kriege M, Heid F, Alflen C, Schmidtmann I, Dette F, Noppens R, Piepho T. The Orogastric Tube Guide(R) as a novel strategy for gastric tube insertion: a prospective, randomized controlled clinical trial. Minerva Anestesiol. 2020;86(4):416-422.
doi pubmed - Long M, Machan M, Tollinche L. Intraoperative gastric tube intubation: a summary of case studies and review of the literature. Open J Anesthesiol. 2017;7(3):43-62.
doi pubmed pmc - Ranier G, Costello K. Fractured OG tip: a case report. W V Med J. 2013;109(5):38-39.
pubmed - Baker RA, Baker S. Orogastric tube placement during trauma arrest. J Am Coll Emerg Physicians Open. 2020;1(4):642-644.
doi pubmed pmc - Pousman RM, Koch SM. Endotracheal tube obstruction after orogastric tube placement. Anesthesiology. 1997;87(5):1247-1248.
doi pubmed - Young MJ, Ehrenfeld JM. Knotting of an orogastric tube around an endotracheal tube. J Clin Anesth. 2012;24(3):254-255.
doi pubmed - Rizk S, El Hajj Moussa W, Assaker N, Makhoul E, Chelala E. Case report about the management of a late Gastro-Gastric Fistula after Laparoscopic Gastric Bypass, with the finding of an unexpected foreign body. Int J Surg Case Rep. 2020;67:117-119.
doi pubmed pmc - Burad J, Deoskar S, Bhakta P, Date R, Sharma P. Avoidance of laryngeal injuries during gastric intubation. Sultan Qaboos Univ Med J. 2014;14(3):e405-408.
pubmed pmc - Wang MY, Huang CK, Chang PC. Hypopharyngeal perforation with mediastinal dissection during orogastric tube placement: a rare complication of bariatric surgery. Surg Obes Relat Dis. 2016;12(2):e17-19.
doi pubmed - Guelfguat M, Kaplinskiy V, Reddy SH, DiPoce J. Clinical guidelines for imaging and reporting ingested foreign bodies. AJR Am J Roentgenol. 2014;203(1):37-53.
doi pubmed - Metheny NA, Krieger MM, Healey F, Meert KL. A review of guidelines to distinguish between gastric and pulmonary placement of nasogastric tubes. Heart Lung. 2019;48(3):226-235.
doi pubmed - Halloran O, Grecu B, Sinha A. Methods and complications of nasoenteral intubation. JPEN J Parenter Enteral Nutr. 2011;35(1):61-66.
doi pubmed - Birk M, Bauerfeind P, Deprez PH, Hafner M, Hartmann D, Hassan C, Hucl T, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(5):489-496.
doi pubmed - Committee ASoP, Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73(6):1085-1091.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


