| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 10, October 2024, pages 297-303
Double Segmental Femoral Fracture: A Rare Injury Following High-Energy Trauma
Athanasios Galanisa, Michail Vavourakisa, b, Spyridon Karampitianisa, Panagiotis Karampinasa, Evangelos Sakellarioua, Georgios Tsalimasa, Iordanis Varsamosa, Angelos Kaspirisa, Elias Vasiliadisa
aThird Department of Orthopaedic Surgery, National and Kapodistrian University of Athens, KAT General Hospital, Athens, Greece
bCorresponding Author: Michail Vavourakis, Third Department of Orthopaedic Surgery, National and Kapodistrian University of Athens, KAT General Hospital, Athens, Greece
Manuscript submitted July 4, 2024, accepted September 5, 2024, published online September 20, 2024
Short title: Double SFF Following High-Energy Trauma
doi: https://doi.org/10.14740/jmc4298
| Abstract | ▴Top |
Femoral fractures are indubitably common injuries that can occur either from high-energy trauma in young patients or due to fragility in the geriatric population. Femoral fractures affecting two or more regions of the femur are exceedingly infrequent injuries, ordinarily caused by high-energy trauma and are considered segmental femoral fractures. We present a rare case of a 33-year-old male patient presented to our Emergency Department with multiple femoral fractures at the subtrochanteric, diaphyseal and supracondylar femoral regions, a condition regarded as double segmental femoral fracture. After assiduous consideration of treatment options, intramedullary nailing was employed for osteosynthesis. Fracture reduction was laborious, as an entirely separated femoral fragment was present between the fracture lines. The reaming process required paramount attentiveness as the middle femoral fragment was prone to rotational displacement by the reamer. Finally, the intramedullary nail was successfully placed, and the patient was discharged without complications after 11 days of hospitalization. Currently, the patient is capable of full weight-bearing without crutches. This paper underlines the challenges that double-segmental femoral fractures’ treatment can bring on to the orthopedic surgeon.
Keywords: Double segmental fracture; Femoral fracture; High-energy trauma; Segmental fracture; Segmental; Trauma; Intramedullary nailing; Nailing
| Introduction | ▴Top |
Femoral shaft fractures are a relatively common type of injury with an annual incidence ranging from 10 to 21 fractures per 100,000 patients and a 1-year mortality of 21% [1]. They are caused either by high-energy trauma in young patients or low-energy mechanism in elderly patients with osteoporosis [1]. Femoral fractures occurring at two or more sites are considered segmental femoral fractures (SFFs) and are usually triggered by high-energy trauma, such as road traffic accidents, falls from height, and crush injuries [2].
Management of SFFs is regarded as distinctly exigent due to the copious treatment options available, the uniqueness of each case, and the comparatively high complication rates [3]. Possible treatment options include intramedullary nailing (IMN), plate and screw fixation, external fixation, or a combination [4].
We present a rare case of a double SFF, a femoral fracture with three different fracture sites, which we treated at our institution. The aim of this paper is to accentuate the arduousness our team coped with regarding the management and treatment of this complex case.
| Case Report | ▴Top |
Investigations
A 33-year-old male patient presented to our Emergency Department after being transferred from a rural community hospital due to a road traffic accident. Past medical history was negligible. Initial clinical evaluation revealed acute right limb pain and extensive thigh edema, with evident deformity and no skin lacerations. No neurovascular impairment was observed.
Diagnosis
Routine radiological workup was carried out involving computed tomography (CT) scans of the head, chest, abdomen and spine. Plain radiographs of the pelvis and right femur revealed multiple femoral fractures at the subtrochanteric, diaphyseal, and supracondylar regions (Fig. 1, lateral radiographs were not performed). In particular, the subtrochanteric fracture was oblique with an anterolateral displacement of the proximal bone segment. Also, in the diaphyseal region, an oblique fracture was discerned. Finally, a transverse fracture line in the supracondylar femoral region with an anterolateral displacement of the proximal fragment was also described. It is crucial to highlight that all fractures completely affected both cortical bone regions. Taking into account all these conspicuous findings, a 6.5-kg proximal tibia skeletal traction was promptly applied to the patient. Additionally, X-rays of his right hand demonstrated a scaphoid fracture, which was treated non-operatively. The patient also presented right humeral subluxation and traumatic scalp wounds, which were managed accordingly. Neurosurgical and oral maxillofacial consultations revealed no abnormalities. Thoracic surgical consultation demonstrated pulmonary contusions. The Injury Severity Score (ISS) calculated at the Emergency Department was 24. Forthwith after admission, a urinary catheter was utilized in order to monitor the patient’s fluid balance and hemodynamic status during the hospitalization. Vital signs were stable; hematocrit (HCT) on admission was 30.2%, with hemoglobin (Hb) 10.2 g/dL. On the second day of hospitalization, the patient was transfused with one packed red blood cells (RBCs) due to HCT dropping to 27.3% (Hb = 9.3 g/dL).
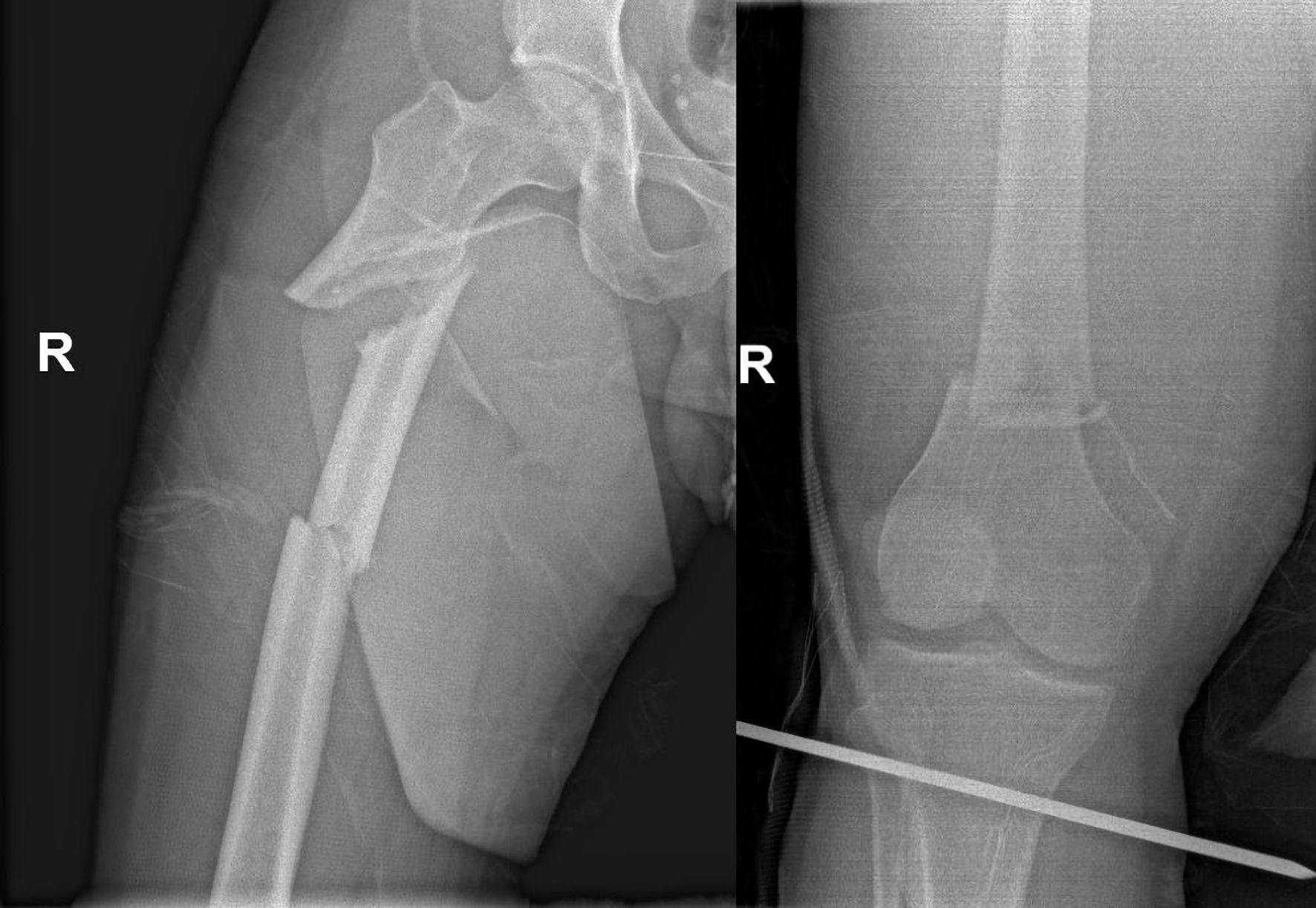 Click for large image | Figure 1. Admission X-rays showing femoral fractures at the subtrochanteric, diaphyseal, and supracondylar regions. |
Treatment
During his hospitalization prior to the operation, the patient’s affected lower limb was neurovascularly examined meticulously four times per day, and no signs of impairment were observed. Also, before surgery, the patient was fully immobilized with the right lower limb constantly elevated, and ice was applied six times per day in order to diminish the extensive thigh edema. Regarding pain management, high doses of paracetamol and tramadol were administered intravenously, while vital signs were checked by the nursing staff once every hour. Fracture fixation was conducted on the third day of hospitalization, as thigh edema was considerably reduced, and soft tissue allowed the operation, whilst hemodynamic status was definitely stable after a series of essential re-examinations (such as abdomen ultrasounds) demanded by our colleagues of other specialties were performed. After punctiliously considering treatment options, we concluded that IMN was the most appropriate treatment approach. Surgery was performed with the patient lying supine on an orthopedic fracture table under general anesthesia, whilst the tibia skeletal traction was removed before the beginning of the operation. TRIGEN TAN® trochanteric antegrade nail (Smith & Nephew, Watford, UK) was used for osteosynthesis. Intraoperatively, the necessary traction was provided and controlled with the aid of the typical orthopedic fracture table. After standard aseptic skin preparation and with the continuous aid of an image intensifier, a typical lateral incision was made above the level of the greater trochanter for standardized awl insertion into the tip of the greater trochanter. Following awl insertion and subsequent typical placement of the intramedullary guidewire, it was advanced until the level of the lesser trochanter. Afterwards, the femur was reamed until the level of the first fracture line in order to expedite the insertion of the company’s specified intramedullary reducer tool. Since advancing the guidewire through the proximal diaphyseal small free segment was unattainable, a second lateral incision was made at the area where the typical approach for lag-screw insertion would be, and was extended both proximally and distally. After cutting the fascia lata and while being extremely attentive regarding soft tissue preservation, four big bone holding forceps were utilized. Two of them were placed under the level of the lesser trochanter proximally and the other two at the level of the second fracture distally. This step enabled us to acceptably reduce the first small bony free segment. Following that, with arduous manipulations, the guidewire was advanced through that first free bony segment. With constant image intensifier assistance, the guidewire was advanced until above the level of the third fracture at the distal femoral metaphysis. At that point, another lateral approach was used at the level of the locking screws insertion and was extended proximally to facilitate the third fracture reduction. After reaching the bone, fracture-reduction was accomplished with the utilization of two pertinent bone holding forceps. After that step, the guidewire was advanced through the last fracture line and was stabilized at the condyle region. It is of paramount significance to underline that advancing the guidewire through the three fractures was obtainable with the assistance of the company’s specified intramedullary reducer. Maintaining the achieved satisfactory reduction of the three fractures was notably challenging, especially in the central and peripheral fracture segments, whilst two assistant surgeons were steadily holding the multiple bone-holding forceps throughout the procedure. Reaming of the femoral canal was executed tremendously gingerly in order to retain the alignment of the fracture fragments. With the employment of two big weber clamps, the middle fragment between the first and second fracture lines was clamped at two parts, both proximally and distally during the whole reaming process to avoid its rotation and subsequent loss of reduction. After vigilant reaming, the nail was inserted into the femoral canal, followed by the timely insertion of central and peripheral screws. Following that step, with careful aseptic manipulations, the affected lower limb was temporarily removed from the fracture table and was contrasted to the other lower limb intraoperatively in order to assess leg length and rotation, which were found similar to the other leg. The patient received an additional unit of packed RBCs during surgery.
Follow-up and outcomes
On the first postoperative day, the patient received another unit of packed RBCs as HCT was 24.5% while Hb was 8.1 g/dL. He was mobilized on the bed during the second postoperative day, while touch-down weight-bearing was permitted on the fifth postoperative day. Partial weight-bearing was initiated on the 10th postoperative day using a Zimmer frame. The patient was discharged after 11 days of hospitalization. No further complications during his hospital stay were noted. After hospital discharge, he was instructed to follow physiotherapy sessions, and multiple regular follow-up visits were scheduled. During the whole follow-up period, both radiological and clinical criteria were used to determine bone union. On the 45th postoperative day, the patient was able to walk with two crutches, whilst, on the 105th day, he started using one crutch. Callus formation was observed at the 3-month follow-up visit (Fig. 2), and the knee range of motion at 90 days was satisfactory (full knee extension and up to 115 degrees of flexion). Finally, he was capable of full weight-bearing without any assistance at 120 days postoperatively. Radiological evaluation at the 6-month and 9-month follow-up visits (Fig. 3) demonstrated good fracture healing, with the patient returning gingerly to his pre-fracture activities. Patient follow-up lasted 12 months, with the patient utterly satisfied with his limb functionality and being able to perform his daily routine with no complaints.
 Click for large image | Figure 2. X-rays at the 3-month follow-up visit. |
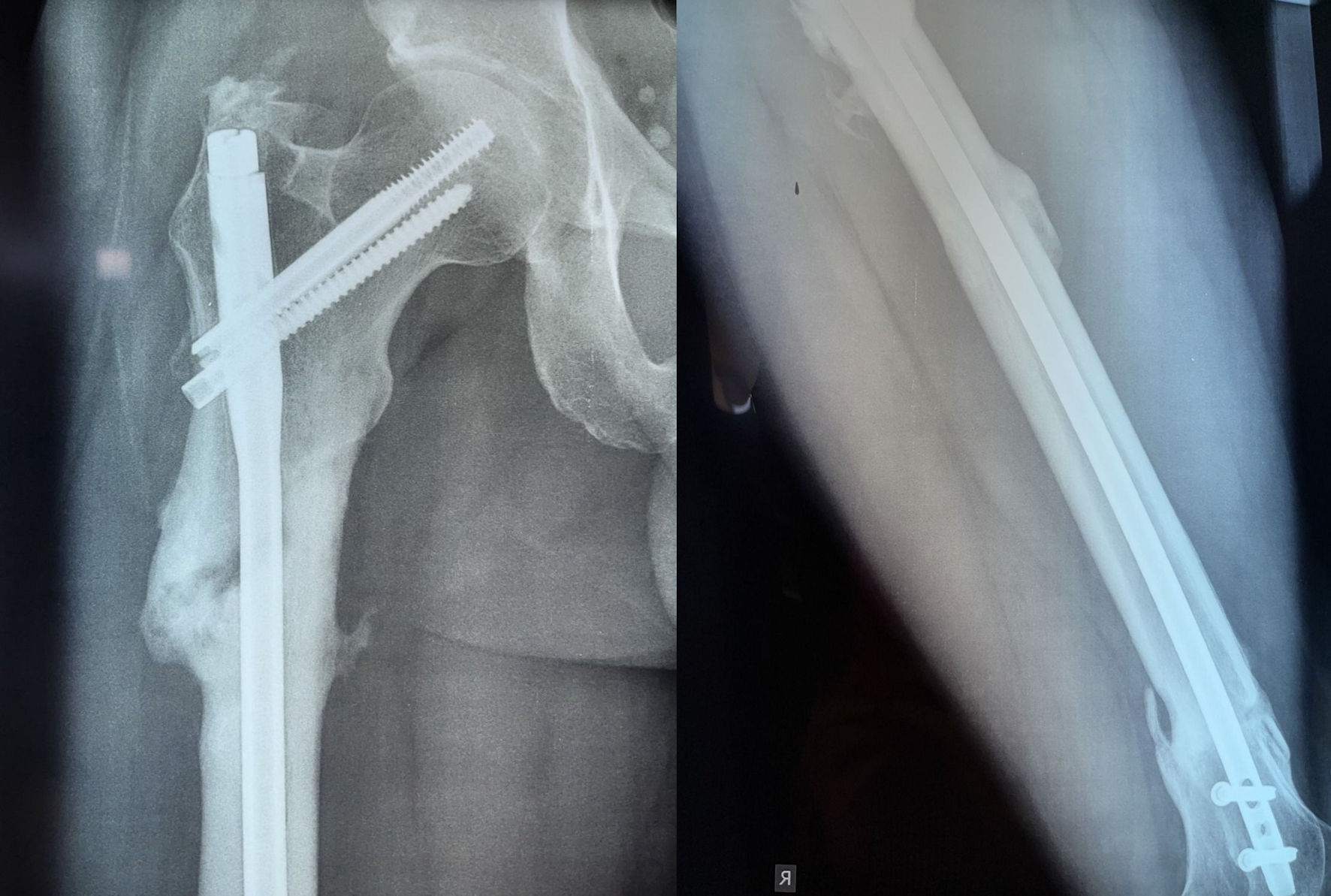 Click for large image | Figure 3. X-rays at the 9-month follow-up visit. |
| Discussion | ▴Top |
SFFs with three separate fracture sites are tremendously infrequent injuries caused by high-energy trauma. They are distinguished from trifocal fractures as they separate entirely the bony segments [5]. Although very few cases of trifocal femoral fractures have been published [6, 7], our report’s absolute separation of bone cortex and malalignment renders this case even more exacting. To our knowledge, this is the fifth case of “double segmental” femoral fracture reported in the existing literature [5, 8, 9].
The diverse nature of these fractures, combined with the lack of randomized controlled trials, poses challenges to selecting the proper treatment. Although published literature suggests that using separate implants to treat SFFs leads to favorable outcomes, it refers exclusively to cases where femoral shaft fractures and femoral neck fractures coexist [10]. A recent study by Kook et al indicated that SFFs demonstrated a comparatively increased nonunion rate when contrasted to non-SFFs with inadequate canal filling of the intramedullary nail and residual fracture gaps to be the chief factors affecting nonunion rates [11]. Also, a small-scale study by Liu et al denoted that combining IMN and plate fixation appeared to be a fruitful method concerning the surgical treatment of SFFs with high union rates and diminished operation time [2]. On the other hand, solid outcomes in terms of the surgical treatment of double SFFs cannot be acquired since they are extremely scarce in the existing literature.
Recent studies on SFFs that employed IMN as a solitary fixation method have demonstrated great outcomes [8, 12]. On the other hand, opting for extramedullary fracture fixation may trigger excessive soft tissue dissection compromising blood supply and increasing stress at the junction of plates [13]. To date, the role of Ilizarov external fixation for SFFs is confined to managing non-unions with large segmental bone defects [14]. Therefore, after a scrupulous examination of our patient’s radiographs and diligent consideration of relevant literature on SFFs, we deduced that IMN was the most pertinent approach. More specifically, we opted for IMN over external fixation since it would be much more tolerable for the patient as it included no evident metalwork. It was a single operation; all three fractures were closed and there was no requirement for damage control orthopedics in our patient. On the other hand, open reduction and internal fixation with multiple plates and screws was not selected for various reasons. Firstly, it would require a huge single incision from the hip region down to the knee, which would not be easily bearable for the patient since he was young, while it would trigger considerable soft tissue damage and would be technically demanding. Furthermore, it would tremendously escalate the cost of the surgical treatment as placing multiple plates and screws would be necessary for optimal fixation. What is more, opting for fixation with plates and screws would markedly increase the risk for postoperative infection and all associated complications, whilst also if this treatment approach was utilized, the patient would be unable to weight-bear for a prolonged period of time postoperatively in comparison with IMN fixation [8-14]. In the same way, another relevant treatment option which was considered was internal fixation with a long femoral plate introduced via a minimally invasive osteosynthesis (MIO) technique. This option was promptly rejected as our team was not adequately familiarized with these specific techniques, and the patient would be incapable of weight-bearing for a long period of time if this approach was selected. Also, this alternative would require the placement of a huge amount of metalwork into the femur, while implant-removal would be much more demanding contrasted to IMN removal.
Surgery’s success is predominantly grounded on proper fracture reduction. In our case, incisions in the central and peripheral fracture segments were requisite to attain fracture reduction prior to guidewire positioning. The uniqueness of having a large bone fragment between the fracture lines in double segmental fractures makes the concurrent reduction of all bone segments demanding for the operating orthopedic surgeon [8, 9]. Reduction methods can vary in multifocal fractures. Open reduction with the employment of small plates with monocortical screws can be one option facilitating the work of the surgeon, while diminishing the needs for several assistants. Also, the use of a great distractor or ex-fix with monocortical screw can control the free fragments aiding reduction and finding of rotation [3, 5-7, 9-11]. In our case, these methods were not employed as the duration of the surgery would be extended, and the effortless existence of multiple surgeon’s assistants and the utilization of bone holding forceps and weber clamps enabled us to accomplish satisfactory reduction in the multiple fracture sites. Regarding the distal fragment, it should be noticed that fixation of the third fracture site could be augmented with a plate or poller screws. We decided not to opt for this approach, as we evaluated that the existing fixation was sufficient enough, the duration of the surgery would be considerably extended, and the amount of implemented metalwork would be increased. Thus, operation cost and the risk for infection would be enhanced and implant removal would be more exacting.
Another key aspect for effective management of double SFFs that should be highlighted is timely management. External fixation should be placed on time if damage-control orthopedics approach is required from the patient’s overall trauma condition and in continuous consultation with the other physicians involved in patient’s treatment. If IMN is the option, it should be carried out timely as delaying surgery could significantly hamper the fracture reduction during surgery [9-13]. On the other hand, it should be noted that the utilization of traction both preoperatively and intraoperatively cannot align free fragments in multisegmental femoral fractures. The existing literature regarding the effect of traction on these fractures is negligible, and all trials have been conducted on single femoral shaft fractures. Consequently, alignment of free fragments in multisegmental fractures can only be achieved by appropriate intraoperative reduction techniques.
The decision of reaming before IMN insertion is another point of interest. Double segmental fractures are featured with a free central bone fragment. During the reaming process, this fragment is susceptible to rotational displacement, which could compromise fracture reduction and may also lead to devascularization [15]. Consequently, the surgeon should be particularly meticulous during the reaming process and clamp the bone fragment, avoiding potentially devastating intraoperative and postoperative complications [9, 15]. In our case, the utilization of multiple bone holding forceps and weber clamps enabled us to reduce the various fractures satisfactorily and retain the position of the free segments throughout the reaming and nailing process. Pertinent reduction of the three separate fracture sites provided proper leg length and rotation, which were evaluated intraoperatively after the typical nailing procedure. Nonetheless, another concern that should be noted in terms of the treatment of these injuries is the varus malalignment of the proximal femur, which is very frequent in subtrochanteric fractures, and happened also in our case [11-13].
During hospitalization, routine lab tests to assess patients’ HCT are considered of pivotal importance. Recent clinical studies indicated that patients suffering from femoral fractures require two transfusion units during hospital stay and operation [16]. Nonetheless, in our case, three units of packed RBCs were demanded. Of note, our patient had no additional injury that could contribute to his acute blood loss.
Finally, taking into consideration the intricate nature of these fractures and the numerous treatment options available, it is imperative to accentuate that the physicians must necessarily provide every appropriate information to the patient regarding the potential risks, benefits, and specific advantages of one procedure compared to another when dealing with double SFFs. In this context, when carrying out an accurate process of informed consent, physicians have the professional duty to present the risks, benefits and potential alternatives to a given procedure [17]. In our case, prior to the surgery and during the informed consent process, the patient was explained in detail our rationale in terms of the treatment option selected by our team.
Conclusions
All in all, “double segmental” femoral fractures are considered extremely rare injuries that arise from high-energy trauma. The copious amount of possible “double segmental” fracture combinations render determining the appropriate fracture fixation choice a rigorous process. Our experience with IMN demonstrated excellent postoperative results, with the patient being capable of full weight-bearing roughly 4 months postoperatively and achieving full range of motion. Further randomized controlled trials contrasting the different treatment options could elucidate the ambiguity of proper fixation selection, providing beneficial information on patients’ outcomes. However, it needs to be highlighted that conducting these necessary trials could not be really feasible considering the extremely infrequent nature of these injuries.
Learning points
This case accentuates the considerably exigent nature of treating double SFFs, which are underreported in the existing literature. Orthopedic surgeons should assiduously consider all possible fixation alternatives, taking into account the specific aspects of these injuries, as every case is unique. Pertinent IMN of the femur should be the first option when operating these cases provided that the double segmental fracture is closed and the potential soft tissue damage is manageable. Also, it is vitally important to underline that trauma surgeons should practice and ameliorate their mini-open surgical techniques, as executing an apposite IMN for the treatment of a double SFF would possibly require utilizing these skills.
Acknowledgments
None to declare.
Financial Disclosure
No funding was received for conducting this study.
Conflict of Interest
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement, etc.) that might pose a conflict of interest in connection with the submitted article.
Informed Consent
Written consent was obtained for the publication of the data presented in this work.
Author Contributions
AG: conceptualization, manuscript preparation - original draft presentation; SK: study design; MV: manuscript preparation - original draft presentation; PK: manuscript preparation - review and editing; ES: data collection, data interpretation; GT: data collection, data interpretation; IV: literature search; AK: manuscript preparation - review and editing; EV: conceptualization, supervision.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Enninghorst N, McDougall D, Evans JA, Sisak K, Balogh ZJ. Population-based epidemiology of femur shaft fractures. J Trauma Acute Care Surg. 2013;74(6):1516-1520.
doi pubmed - Liu H, Wu J, Lin D, Lian K, Luo D. Results of combining intramedullary nailing and plate fixation for treating segmental femoral fractures. ANZ J Surg. 2019;89(4):325-328.
doi pubmed - Ferreira N, Britz E, Gould A, Harrison WD. The management of segmental femur fractures: the radiographic 'cover-up' test to guide decision making. Injury. 2022;53(8):2865-2871.
doi pubmed - Adeel M, Zardad S, Jadoon SM, Younas M, Shah U. Outcome of open interlocking nailing in closed fracture shaft of femur. J Ayub Med Coll Abbottabad. 2020;32(4):546-550.
pubmed - Bansal N, Singh G, Tiwari P, Kaur H. Double trouble of "Double Segmental" fractures - a report of two cases. J Orthop Case Rep. 2022;12(2):30-33.
doi pubmed pmc - Griffin M, Dick AG, Umarji S. Outcomes after trifocal femoral fractures. Case Rep Surg. 2014;2014:528061.
doi pubmed pmc - Papaioannou I, Baikousis A, Korovessis P. Trifocal Femoral Fracture Treated With an Intramedullary Nail Accompanied With Compression Bolts and Lag Screws: Case Presentation and Literature Review. Cureus. 2020;12(5):e8173.
doi pubmed pmc - Loganathan S, Thiyagarajan U. Multilevel segmental femur fracture in young individuals treated by a single step - All in one intramedullary device - A prospective study. Biomedicine. 2021;40(4):488-491.
- Velmurugeasn D, Valleri DP, Jayaramaraju D, Rajasekaran S. Double segmental femur fracture: Two case reports with a technical note and perioperative illustration. International Journal of Orthopaedics Sciences. 2020;6(2):618-621.
- Wei YP, Lin KC. Dual-construct fixation is recommended in ipsilateral femoral neck fractures with infra-isthmus shaft fracture: A STROBE compliant study. Medicine (Baltimore). 2021;100(17):e25708.
doi pubmed pmc - Kook I, Park KC, Kim DH, Sohn OJ, Hwang KT. A multicenter study of factors affecting nonunion by radiographic analysis after intramedullary nailing in segmental femoral shaft fractures. Sci Rep. 2023;13(1):7802.
doi pubmed pmc - Wu KT, Lin SJ, Chou YC, Cheng HH, Wen PC, Lin CH, Yeh WL. Ipsilateral femoral neck and shaft fractures fixation with proximal femoral nail antirotation II (PFNA II): technical note and cases series. J Orthop Surg Res. 2020;15(1):20.
doi pubmed pmc - Howe TS. Double level fractures of the femur treated with closed intramedullary nailing. Ann Acad Med Singap. 1998;27(2):188-191.
pubmed - Zhang Q, Zhang W, Zhang Z, Zhang L, Chen H, Hao M, Deng J, et al. Femoral nonunion with segmental bone defect treated by distraction osteogenesis with monolateral external fixation. J Orthop Surg Res. 2017;12(1):183.
doi pubmed pmc - Arastu MH, Sheehan B, Paolucci EO, Buckley RE. Does it really spin? Intra-medullary nailing of segmental tibial fractures—a cadaveric study. Injury. 2015;46(4):643-648.
doi pubmed - Wertheimer A, Olaussen A, Perera S, Liew S, Mitra B. Fractures of the femur and blood transfusions. Injury. 2018;49(4):846-851.
doi pubmed - Bolcato V, Franzetti C, Fassina G, Basile G, Martinez RM, Tronconi LP. Comparative study on informed consent regulation in health care among Italy, France, United Kingdom, Nordic Countries, Germany, and Spain. J Forensic Leg Med. 2024;103:102674.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


