| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 11, November 2024, pages 354-358
Epididymo-Orchitis Mimicking Malignancy Resulting From Intravesical Bacillus Calmette-Guerin Immunotherapy for Bladder Cancer: An Attempt to Understand Pathophysiology, Diagnostic Challenges, Patients’ Implications and Future Directions
Sharadchandra K. Prasada, g, Fahmi Sabr Razaa, Sourabh Karnaa, Nahin M. Hoqa, Robert McCormicka, Abu Sadiqa, Imoh Ibioka, Achamma Johnb, Mohammed Mansoor Razac, Mohamed H. Ahmedd, e, f, Mohammed Alsheikha
aDepartment of Urology, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
bDepartment of Pathology, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
cDepartment of Infectious Diseases and Microbiology, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
dDepartment of Medicine and HIV Metabolic Clinic, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
eDepartment of Geriatric Medicine, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
fHonorary Senior Lecturer of the Faculty of Medicine and Health Sciences, University of Buckingham, Buckingham, UK
gCorresponding Author: Sharadchandra K. Prasad, Department of Urology, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
Manuscript submitted August 25, 2024, accepted September 26, 2024, published online October 10, 2024
Short title: BCG-Induced Epididymo-Orchitis Mimicking Malignancy
doi: https://doi.org/10.14740/jmc4323
| Abstract | ▴Top |
This case report describes an 85-year-old patient who presented with painless, unilateral right testicular swelling of 2 months’ duration. This raised the possibility of testicular cancer, especially given his recent treatment for bladder cancer, which included adjuvant intravesical bacillus Calmette-Guerin (BCG) therapy. This poses a diagnostic dilemma regarding tuberculosis (TB) of the testis, BCG complications or a true testicular malignancy. Biochemical markers and a computed tomography (CT) scan showed no evidence of malignancy or disseminated TB. A TB-ELISpot test was negative. An ultrasound of the testis revealed a hypoechoic soft tissue lesion measuring approximately 24 × 19 mm, with internal vascularity and calcifications, causing a bulge in the testicular capsule with probable extracapsular extension. Based on the clinical suspicion of a testicular tumor, a right inguinal orchidectomy was performed. Histopathologic examination revealed isolated tuberculous orchitis with focal epididymal involvement; the spermatic cord was not involved. Polymerase chain reaction (PCR) testing on the histological sample confirmed the presence of Mycobacterium bovis DNA. As a radical right orchidectomy had been performed, no abnormal tissue remained. Additionally, the CT scan showed no evidence of TB dissemination, and the patient was asymptomatic, so he was being closely monitored in the infectious disease clinic. Importantly, a urine culture became positive for TB, and he was started on antituberculosis medication. BCG-induced granulomatous epididymo-orchitis may rarely occur as a late complication following intravesical BCG therapy for superficial bladder cancer. In this case report, we attempted to understand the pathophysiology, diagnostic challenges, patient implications, and potential future research directions.
Keywords: Testicular tumor; Tuberculous orchitis; BCG
| Introduction | ▴Top |
As part of the adjuvant treatment for bladder cancer, intravesical bacillus Calmette-Guerin (BCG) immunotherapy is used [1]. BCG can delay tumor progression and eradicate residual tumors in 60% of patients with papillary carcinoma and in 70% of patients with carcinoma in situ [1, 2]. It is very rare for BCG administration to be associated with tuberculosis (TB) of the urinary tract or testis. A few reports have shown associations between tuberculous epididymo-orchitis and BCG administration. For instance, Chiu et al [3] reported a patient with BCG-related epididymo-orchitis who had bladder cancer and a history of intravesical BCG immunotherapy. The diagnosis of TB was confirmed after a right radical orchiectomy, with a positive tumor pus culture for the Mycobacterium tuberculosis (MTB) complex. He was treated with antituberculosis medications [3]. Klebanov et al [4] reported a case involving a 55-year-old Puerto Rican patient with bladder cancer treated with BCG. He developed left testicular pain, and his symptoms did not resolve after treatment with ciprofloxacin. A subsequent ultrasound showed features suggestive of BCG orchitis. Treatment with levofloxacin and antituberculosis medications led to the resolution of his symptoms, despite the absence of positive cultures. The authors concluded that early anti-tuberculous treatment should be considered in case of high clinical suspicion [4]. Colomba et al [5] described a 69-year-old patient with type 2 diabetes and ulcerative colitis who experienced left testicular pain and a mass following BCG treatment for bladder cancer. The urine culture was negative, an ultrasound scan revealed an abscess, necessitating surgery (left orchidectomy and funiculus spermaticus ligature). Histology showed presence of TB, computed tomography (CT) showed presence of the right pulmonary lobe. An interferon-gamma release assay confirmed immune reactivity to MTB, whereas examinations of three sputum and urine samples using the Ziehl-Neelsen (ZN) technique and polymerase chain reaction (PCR) for MTB were negative. He was also treated with antituberculosis medication [5]. Bulbul et al [6] encountered a similar patient presentation. They performed a left orchiectomy, and histology revealed presence of TB, and patient was treated with antituberculosis therapy [6]. Importantly, this rare complication of BCG-induced orchitis may take a long time to develop. For instance, in one case report, BCG-related epididymo-orchitis occurred 3 years after BCG treatment [7]. Therefore, BCG-related epididymo-orchitis is a rare entity in urology but represents a diagnostic challenge, as it can mimic a testicular mass or cancer. Clinical examination, tumor markers, and ultrasound imaging are used to guide the diagnosis of testicular tumors. Radical orchiectomy serves a dual purpose, offering both diagnostic and therapeutic benefits. In this case report, we discuss whether all patients should undergo radical orchiectomy and explore the utility of fine-needle aspiration (FNA) as an alternative diagnostic modality in association of ultrasound. This consideration is important because the majority of these patients are elderly, and additional surgical interventions may increase anxiety, morbidity, and mortality.
| Case Report | ▴Top |
An 85-year-old male with bladder cancer underwent transurethral resection of bladder tumor (TURBT) and intravesical mitomycin C (MMC). One year later, he had a recurrence of high-grade tumor, and received adjuvant intravesical BCG therapy at the standard dose of 81 mg weekly for 6 weeks, followed by 3-weekly up for 3 months, and then every 6 months for 1 year.
One year after completing BCG, he presented with a hard, non-tender lump in the right testis, clinically and radiological raised high possibility of a testicular tumor. Examination in clinic did not reveal any cervical, axillary, or inguinal lymphadenopathy. Chest examination was essentially clear. Liver and spleen were not palpable. There was no exposure to TB in the past. There was no reaction to the intravesical BCG, fever, night sweats or weight loss. An ultrasound of the testis (Fig. 1) showed a hypoechoic soft tissue lesion measuring about 24 × 19 mm, with internal vascularity and calcifications, seen inducing a bulge of the testicular capsule with probable extracapsular extension suggestive of testicular tumor. The appearance of the left testis and left epididymis was unremarkable.
 Click for large image | Figure 1. Ultrasound of the testes shows a hypoechoic soft tissue lesion measuring about 24 × 19 mm, with internal vascularity and calcifications, seen inducing a bulge of the testicular capsule with probable extracapsular extension. |
Testicular tumor markers including alpha fetoprotein (AFP), beta-human chorionic gonadotropin (β-HCG), and lactate dehydrogenase (LDH) were normal. Staging CT scan of the chest, abdomen and pelvis was normal. There was no axillary or mediastinal lymphadenopathy, and no abdominal visceral lesions visualized. He underwent a right radical orchidectomy. Pathology showed granulomatous inflammation with multiple well-formed granulomas, extensive areas of caseation necrosis and focal calcification (Fig. 2a-c). Ziehl-Nielsen staining showed the presence of acid-fast bacilli (Fig. 3). The TB-ELISpot test was negative. PCR testing on the histological sample confirmed the presence of Mycobacterium bovis DNA. As a radical right orchidectomy had been performed, no abnormal tissue remained. Additionally, the CT scan showed no evidence of TB dissemination, and the patient was asymptomatic, so he was being closely monitored in the infectious disease clinic. Importantly, a urine culture became positive for TB, and he was started on antituberculosis medication.
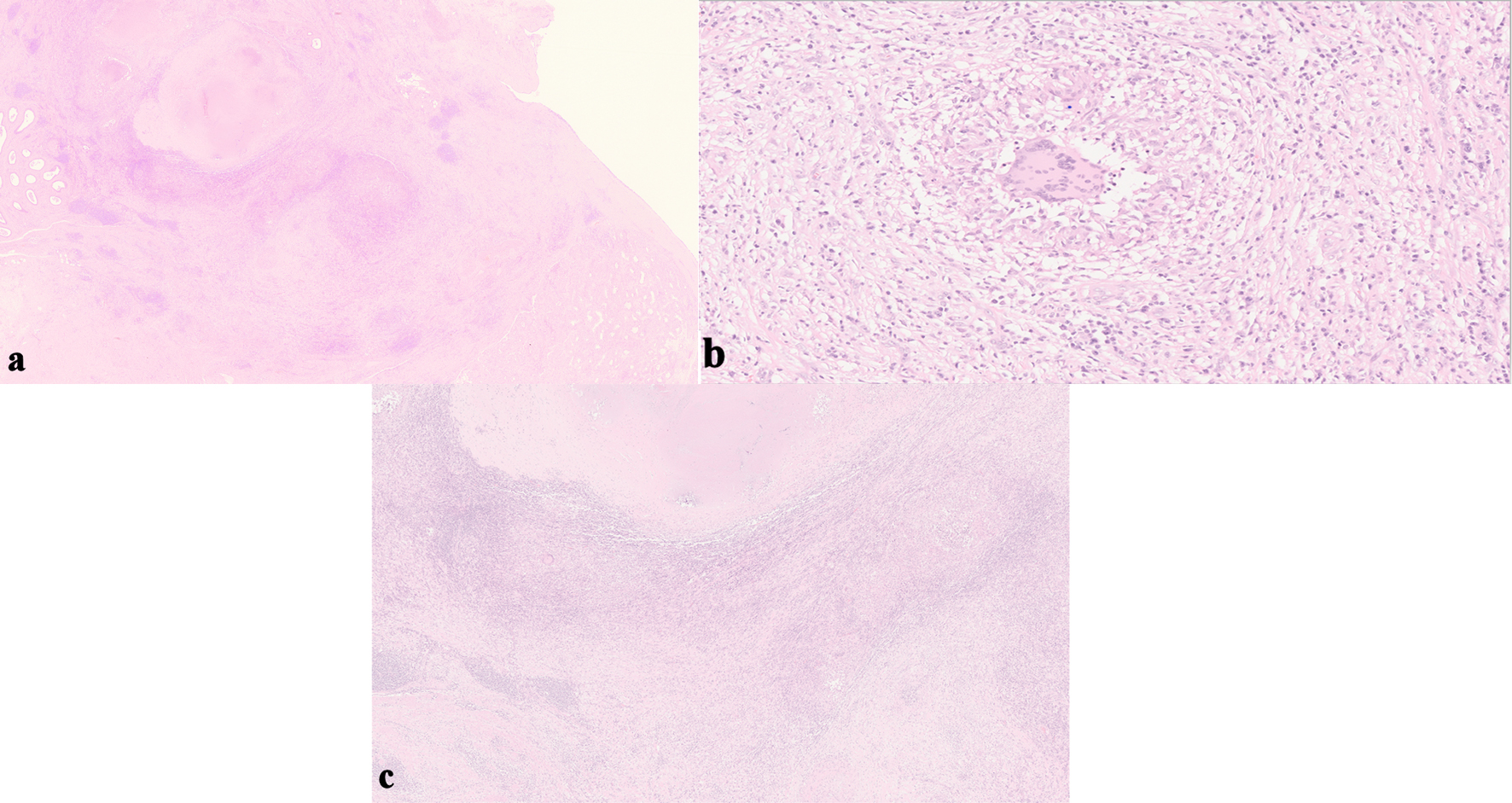 Click for large image | Figure 2. Histopathology of the resected testes shows granulomatous inflammation with multiple well-formed granulomas, extensive areas of caseation necrosis and focal calcification. (a) Necrosis of the testis. (b) Extensive area of granuloma. (c) Areas of caseation necrosis and focal calcification. |
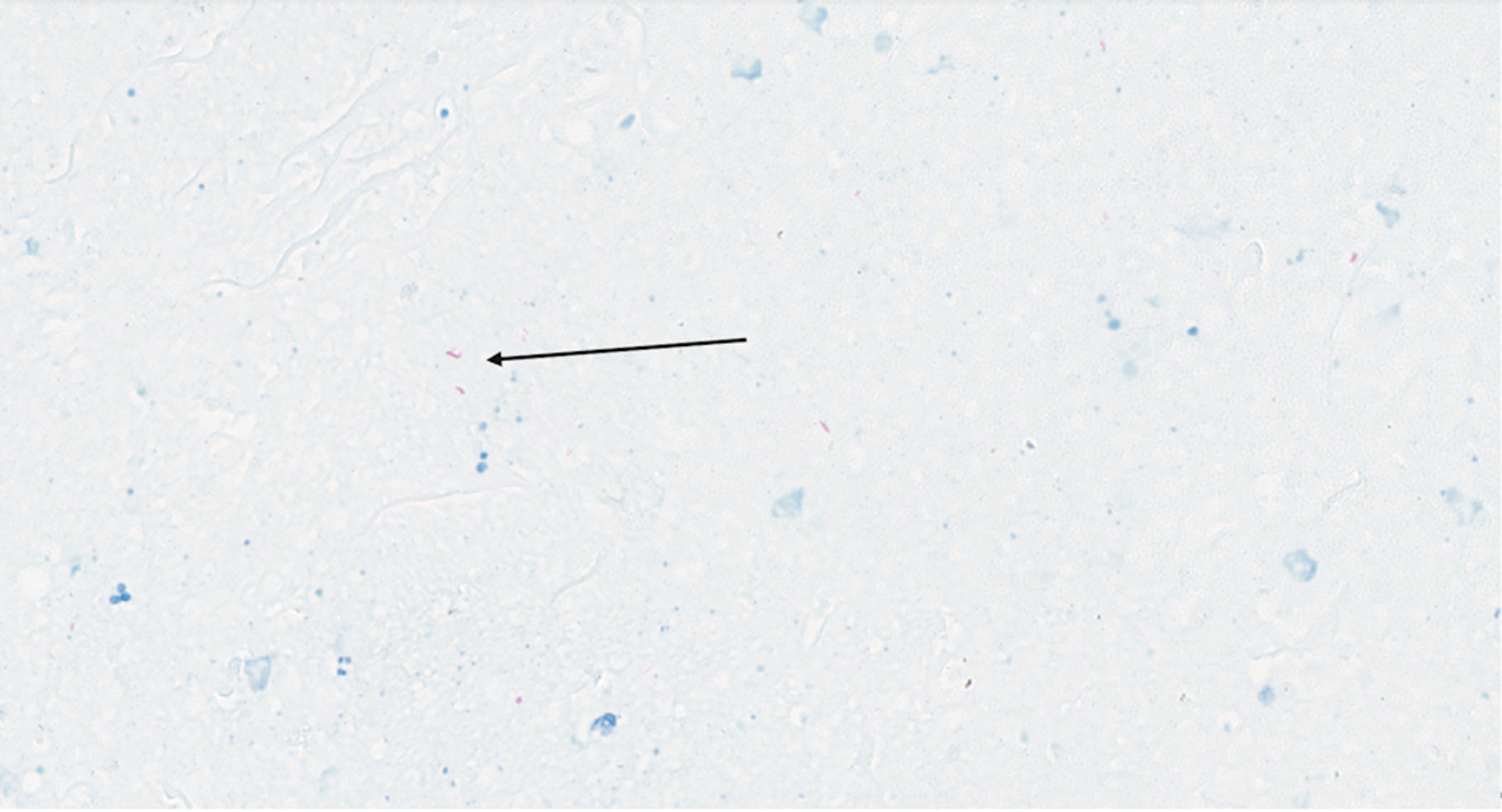 Click for large image | Figure 3. Ziehl-Neilsen staining showed the presence of acid-fast bacilli (arrow). |
| Discussion | ▴Top |
Hard, painless testicular swellings are a classic presentation of testicular tumors. Testicular cancers are rare in the elderly. Non-seminomatous germ cell tumors often occur in men in their 20s and 30s, while seminomas are typically diagnosed in men in their 30s and 40s. The incidence of both seminoma and non-seminoma decreases after the age of 50, while the incidence of spermatocytic tumors increase, particularly beyond the age of 65. These tumors can be treated with orchidectomy, with or without chemotherapy. Rarely, non-Hodgkin lymphomas (NHLs) can be seen in the elderly (over 60 years old) and can also be treated with orchidectomy, chemotherapy, and/or radiation [8].
Systemic complications following intravesical BCG therapy can range from symptoms resembling influenza (fever, malaise, arthritis, and arthralgia) to full-blown disseminated disease (including liver dysfunction, cytopenia, and BCG-positive granulomas in the liver, lymph nodes, lungs, bone marrow, or spleen) [9]. These effects are usually seen within 6 months of the initial intravesical therapy. The late occurrence of focal granulomatous disease is an unusual presentation. In this case, the patient experienced the onset of testicular swelling more than 10 months after completing intravesical BCG therapy. He had no other symptoms related to BCG therapy. BCG-induced orchitis is a rare complication of intravesical therapy. A previous or latent TB infection does not appear to increase the risk of BCG orchitis. Tuberculous epididymo-orchitis may also develop very late; one study reported a case presenting as late as 17 years post-therapy [10].
The pathogenesis of BCG-related epididymo-orchitis is uncertain. It can affect either the left or right testicle, resulting in necrotic areas in the epididymis. The infection may involve the tail or the entire body of the epididymis. The testis may become infected either primarily from the epididymis or through hematogenous spread, although isolated tuberculous orchitis from hematogenous spread is uncommon. Granulomatous epididymo-orchitis may be difficult to clinically differentiate from malignant testicular neoplasms. It is not yet clear whether the presence of other immunocompromising conditions, such as diabetes or inflammatory bowel disease, may also increase the risk [5].
Further research is needed to understand the pathophysiology of BCG-related epididymo-orchitis and its associated risk factors, though recruiting patients for such studies is challenging due to the rarity of the condition.
Most of the cases reported above involved radical orchiectomy, which is significant because the majority of these patients are elderly, and this procedure can increase anxiety, morbidity, and mortality. The utility of fine-needle aspiration cytology (FNAC) as an alternative diagnostic modality for BCG-related epididymo-orchitis has been demonstrated in a few studies. This is particularly important for older patients, as additional surgical interventions may heighten anxiety, morbidity, and mortality. For instance, Garbyal et al showed that FNAC can be used as the first choice in diagnosing tuberculous orchitis [11]. Kumar et al also demonstrated that FNAC is a useful modality for diagnosing tuberculous orchitis [12]. Importantly, Sah et al [13] found that in 40 patients with tubercular epididymitis or epididymo-orchitis, FNAC was diagnostic in 27 cases (showing epithelioid cell granulomas with caseation) but non-diagnostic in the rest. The diagnosis was confirmed directly by detecting acid-fast bacilli (AFB) on FNA smears in 24 patients and in urine samples from 11 patients, and indirectly in nine patients with negative AFB by using a combination of a positive Mantoux test (five of nine), the presence of caseating granulomas on FNA smears (seven of nine), and therapeutic response to anti-tuberculous medication (nine of nine) [13].
Handa et al [14] conducted a retrospective analysis of 40 patients diagnosed with granulomatous or tubercular epididymo-orchitis based on FNAC findings. Of the 40 patients studied, aspiration smears revealed epithelioid cell granulomas with caseation in 17 cases, granulomas alone in 19 cases, and caseation only in four cases. Acid-fast bacilli were observed in 15 cases. The cytologic diagnoses rendered were tubercular epididymo-orchitis in 15 cases, granulomatous inflammation suggestive of TB in six cases, and granulomatous inflammation in 19 cases [14]. Both Handa and Sah concluded that FNAC has good diagnostic utility and may avoid unnecessary orchidectomy in a significant number of patients [13, 14].
Even though FNAC is not a standard approach for suspected malignant lesions of the testes, the potential utility of combining testicular ultrasound with FNAC could be a subject for future research. Interestingly, Muttarak et al and Salvador et al showed that certain anatomical changes seen on ultrasound might indicate BCG-related epididymo-orchitis or testicular cancer [10, 15]. It is plausible to suggest the need for further research to establish the sensitivity and specificity of the combined use of FNAC and ultrasound in differentiating between BCG-related epididymo-orchitis and testicular cancer. This differentiation is crucial to avoid unnecessary orchidectomy, especially in patients under the age of 65 who may undergo contralateral orchidectomy and subsequently be at a higher risk of developing osteoporosis and fractures in the future. If testicular malignancy cannot be excluded, radical orchidectomy is recommended for definitive diagnosis and further management. Mycobacterial culture and clinical assessment are essential for determining whether antituberculosis therapy is recommended [16, 17].
Our literature review suggests that treatment for BCG orchitis with a combination of anti-tuberculous therapy should be initiated when there is a high index of clinical suspicion. BCG epididymo-orchitis may be clinically indistinguishable from malignancy, and in such cases, orchiectomy can be performed as both a diagnostic and therapeutic procedure. The literature indicates that anti-tuberculous therapy is an effective treatment for tuberculous epididymo-orchitis, with orchidectomy reserved for non-viable testes with abscess formation [16, 17].
Conclusions
Intravesical BCG immunotherapy is used for high-grade non-invasive bladder cancer. BCG tuberculous epididymo-orchitis is an important complication of this therapy. Various diagnostic modalities can be employed to establish the diagnosis of this rare condition. Future research is needed to improve the diagnostic yield of combined use of ultrasound and FNAC in differentiating BCG tuberculous epididymo-orchitis from testicular cancer. This differentiation is crucial to avoid unnecessary orchidectomy, which can have significant implications for psychological well-being, mortality, and morbidity.
Acknowledgments
We are grateful for all the team in the Urology Department in Milton Keynes University Hospital for their unlimited cooperation.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent for publication of this case report was obtained from the patient.
Author Contributions
Conception and design: SKP, AS, MR, MA. Administrative support: all authors. Provision of study materials or patients: all authors. Collection and assembly of data: SKP, AS, MA, and MHA. Data analysis and interpretations, manuscript writing, and final approval of manuscript: all authors.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Houghton BB, Chalasani V, Hayne D, Grimison P, Brown CS, Patel MI, Davis ID, et al. Intravesical chemotherapy plus bacille Calmette-Guerin in non-muscle invasive bladder cancer: a systematic review with meta-analysis. BJU Int. 2013;111(6):977-983.
doi pubmed - Jokisch JF, Karl A, Stief C. Intravesical immunotherapy in nonmuscle invasive bladder cancer. Indian J Urol. 2015;31(4):304-311.
doi pubmed pmc - Chiu LW, Tsai LH, Hsieh PF, Chen WC, Chang CH. Tuberculosis epididymo-orchitis mimicking malignancy resulting from intravesical bacillus calmette-guerin immunotherapy for bladder cancer: a case report of a rare complication. Diagnostics (Basel). 2022;12(11):2663.
doi pubmed pmc - Klebanov N, Raghavan A. Tuberculous orchitis following intravesical bacille calmette-guerin (BCG) therapy. Cureus. 2018;10(5):e2703.
doi pubmed pmc - Colomba C, Di Carlo P, Guadagnino G, Siracusa L, Trizzino M, Gioe C, Cascio A. A Case of Epididymo-orchitis after intravesical bacille Calmette-Guerin therapy for superficial bladder carcinoma in a patient with latent tuberculosis infection. Infect Agent Cancer. 2016;11:25.
doi pubmed pmc - Bulbul MA, Hijaz A, Beaini M, Araj GF, Tawil A. Tuberculous epididymo-orchitis following intravesical BCG for superficial bladder cancer. J Med Liban. 2002;50(1-2):67-69.
pubmed - Falkensammer C, Gozzi C, Hager M, Maier H, Bartsch G, Holtl L, Rehder P. Late occurrence of bilateral tuberculous-like epididymo-orchitis after intravesical bacille Calmette-Guerin therapy for superficial bladder carcinoma. Urology. 2005;65(1):175.
doi pubmed - Lantz AG, Power N, Hutton B, Gupta R. Malignant lymphoma of the testis: a study of 12 cases. Can Urol Assoc J. 2009;3(5):393-398.
doi pubmed pmc - Liu Y, Lu J, Huang Y, Ma L. Clinical Spectrum of Complications Induced by Intravesical Immunotherapy of Bacillus Calmette-Guerin for Bladder Cancer. J Oncol. 2019;2019:6230409.
doi pubmed pmc - Salvador R, Vilana R, Bargallo X, Araque X, Nicolau C. Tuberculous epididymo-orchitis after intravesical BCG therapy for superficial bladder carcinoma: sonographic findings. J Ultrasound Med. 2007;26(5):671-674.
doi pubmed - Garbyal RS, Gupta P, Kumar S, Anshu. Diagnosis of isolated tuberculous orchitis by fine-needle aspiration cytology. Diagn Cytopathol. 2006;34(10):698-700.
doi pubmed - Kumar PV, Owji SM, Khezri AA. Tuberculous orchitis diagnosed by fine needle aspiration cytology. Acta Cytol. 1996;40(6):1253-1256.
doi pubmed - Sah SP, Bhadani PP, Regmi R, Tewari A, Raj GA. Fine needle aspiration cytology of tubercular epididymitis and epididymo-orchitis. Acta Cytol. 2006;50(3):243-249.
doi pubmed - Handa U, Kundu R, Raghubanshi G, Bhalla V. Granulomatous epididymo-orchitis: diagnosis by fine needle aspiration. Trop Doct. 2018;48(1):17-20.
doi pubmed - Muttarak M, Lojanapiwat B, Chaiwun B, Wudhikarn S. Preoperative diagnosis of bilateral tuberculous epididymo-orchitis following intravesical Bacillus Calmette-Guerin therapy for superficial bladder carcinoma. Australas Radiol. 2002;46(2):183-185.
doi pubmed - Lamm DL. Efficacy and safety of bacille Calmette-Guerin immunotherapy in superficial bladder cancer. Clin Infect Dis. 2000;31(Suppl 3):S86-90.
doi pubmed - Parker SG, Kommu SS. Post-intravesical BCG epididymo-orchitis: case report and a review of the literature. Int J Surg Case Rep. 2013;4(9):768-770.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


