| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 1, Number 2, October 2010, pages 61-63
Giant Radiation-Induced Thoracic Malignant Schwannoma
Mazen Sanoufaa, Mohammad Sami Walida, b
aMedical Center of Central Georgia, 840 Pine Street, Suite 950, Macon, Georgia, USA
bCorresponding author: Mazen Sanoufa
Manuscript accepted for publication September 15, 2010
Short title: Thoracic Malignant Schwannoma
doi: https://doi.org/10.4021/jmc55w
| Abstract | ▴Top |
Schwannomas growing to large sizes in the thoracic cavity are rare. We report such a case in a patient with a history of Hodgkin’s lymphoma and radiotherapy more than two decades before, an example of a radiation-induced malignant schwannoma with a bad prognosis.
Keywords: Giant Malignant Schwannoma; Hodgkin’s Lymphoma; Radiotherapy
| Introduction | ▴Top |
Spinal schwannomas have an incidence of 0.3 - 0.4 cases/100,000 persons per year and account for 25% of intradural spinal cord tumors [1, 2].
| Case Report | ▴Top |
A 42-year-old female presented to our emergency department with weakness and loss of sensation in the right foot of one week duration. General medical exam was unremarkable. Muscle strength in the right lower extremity was 1+ and left lower extremity 3+. Deep tendon reflexes were intact bilaterally. Toes were down-going bilaterally. She had stocking-like anesthesia in the entire right lower extremity and below the calf in the left lower extremity. She had a history of Hodgkin’s lymphoma treated 22 years ago with radiation therapy. Magnetic resonance imaging (MRI) showed a huge 9.3 × 9.4 × 9.3 cm mass in the right thoracic cavity originating from the spinal canal (Fig. 1, 2). Fine needle aspiration revealed malignant schwannoma compatible with malignant peripheral nerve sheath tumor. The patient had T1-3 laminectomy and resection of the intradural-extramedullary neoplasm. She also had thoracotomy and resection of the intracavitary lesion. Unfortunately, the patient expired within several months after surgery.
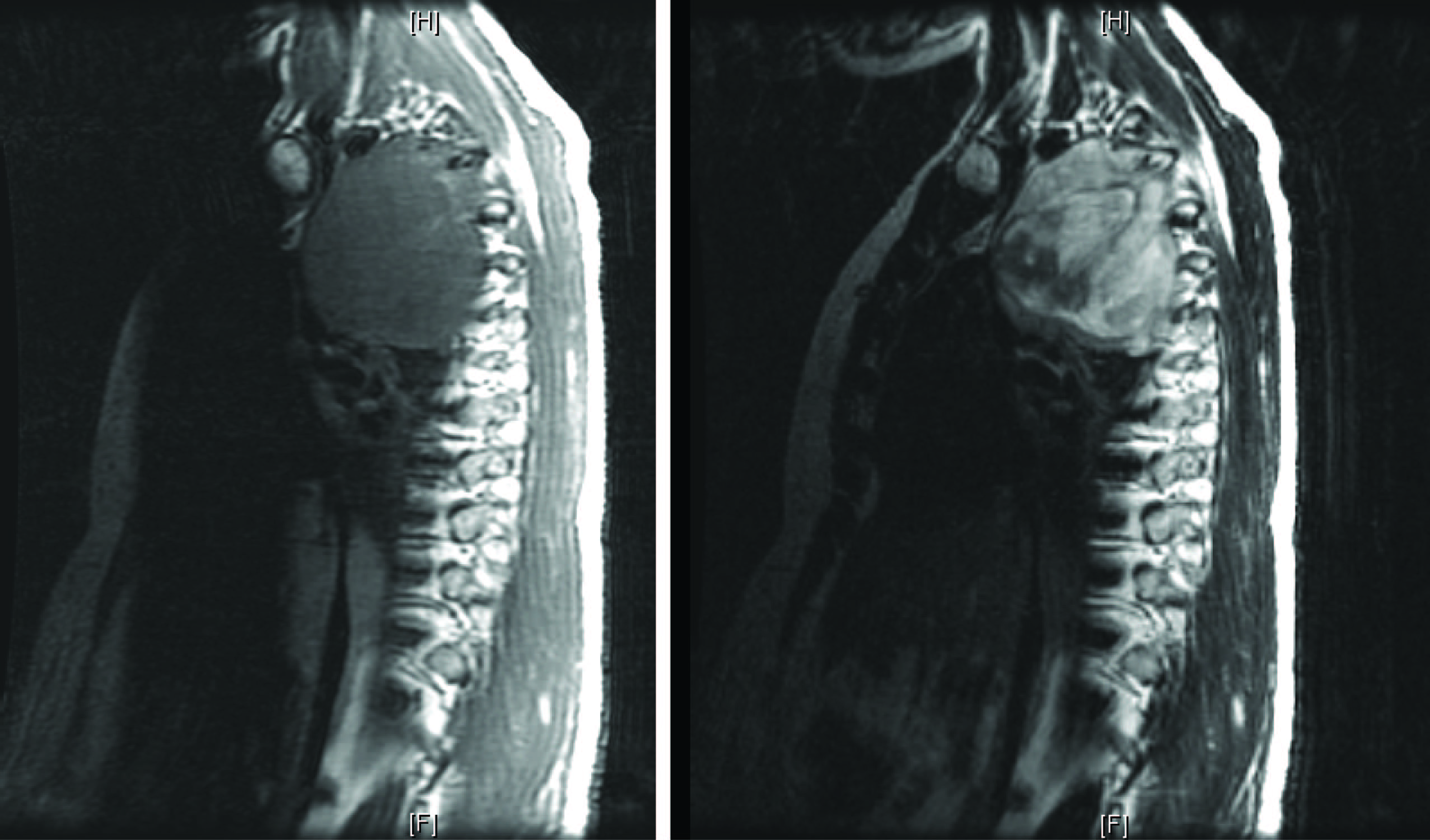 Click for large image | Figure 1. MRI T1 (left) and T2 (right) sagittal views of the thoracic cage. |
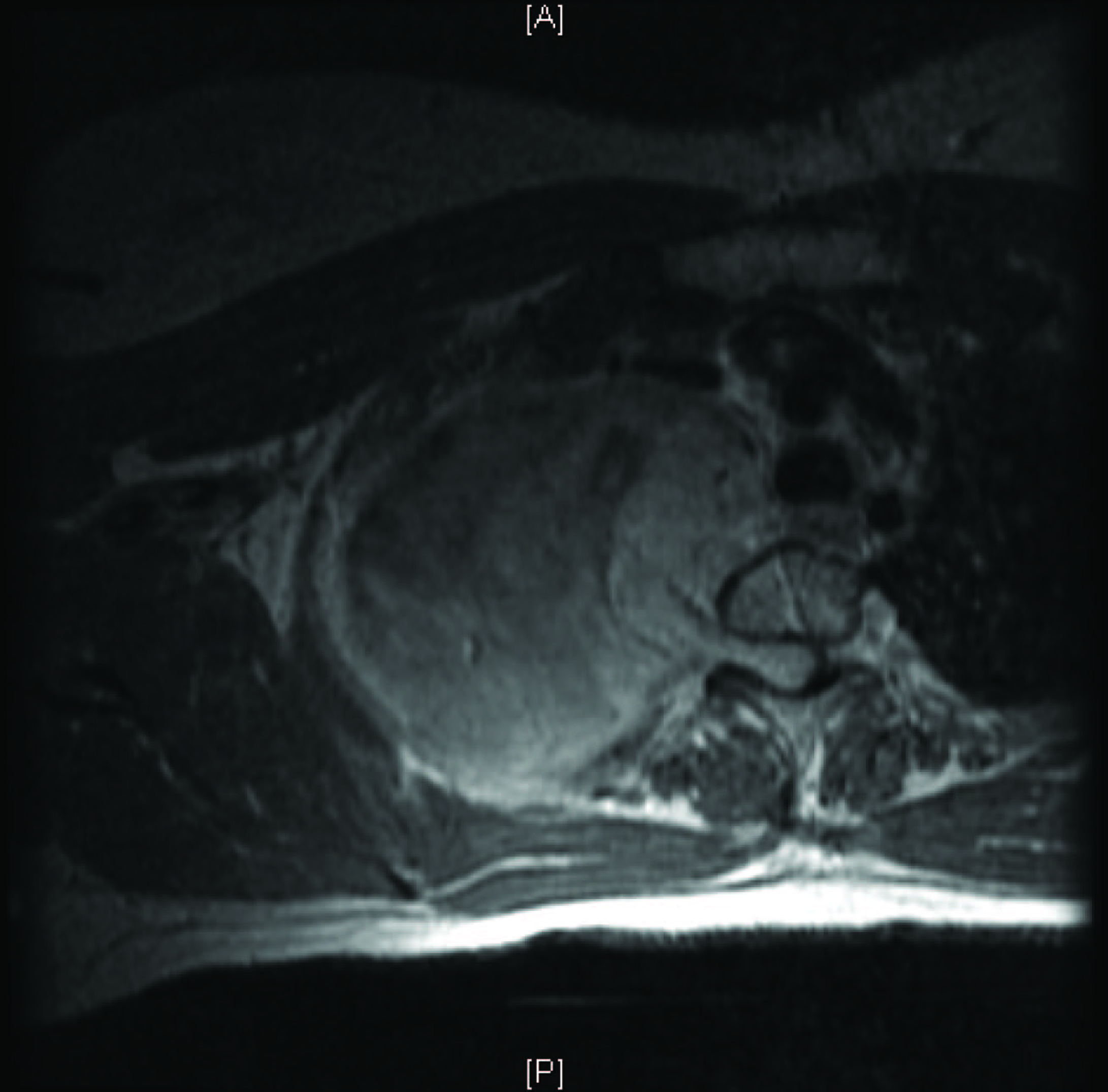 Click for large image | Figure 2. MRI T1 transverse view of the thoracic cage. |
| Discussion | ▴Top |
This is a very rare case of a giant type IV schwannoma growing in the confined space of the thoracic cavity without significant pulmonary symptoms. A giant type IV schwannoma is an intraspinal-extraspinal dumbbell-like tumor with the extraspinal component more than 2.5 cm in diameter [2]. Spinal schwannomas are mostly benign and extramedullary and rarely grow beyond 6 - 8 cm in diameter without giving significant symptoms [2-6]. They may, however, manifest themselves in different ways. For example, Georghiou et al., 2003, reported a 57-year-old woman who presented with progressively aggravated dyspnea at rest, productive cough, and a referred vague left chest pain. She was found to have a 12 × 14 cm schwannoma compressing the upper lobe of the left lung and displacing the mediastinum with subocclusion of the main pulmonary artery [7]. Kara et al, 2002, reported a 45-year-old woman who presented with cough and mild sputum production and was found to have a 16 cm ancient schwannoma in her left hemithorax [8]. On the other hand, Kumar et al, 2006, reported an incidental finding of a 14 × 15 × 19 cm schwannoma in the right hemithorax of a 59-year-old woman [4]. Schwannomas, thus, can be insidious tumors that give subtle symptoms for many years before the patient decides to seek medical help [9] or discovering them by chance [10].
Our case is interesting because previous radiotherapy probably contributed to the pathogenesis of the schwannoma. These tumors can occur 10 to 50 years after the original radiation [11-14]. Malignant forms of these tumors have dim prognosis [15-17].
| References | ▴Top |
- Sridhar K, Ramamurthi R, Vasudevan MC, Ramamurthi B. Giant invasive spinal schwannomas: definition and surgical management. J Neurosurg 2001;94(2 Suppl):210-215.
pubmed - Jeon JH, Hwang HS, Jeong JH, Park SH, Moon JG, Kim CH. Spinal schwannoma; analysis of 40 cases. J Korean Neurosurg Soc 2008;43(3):135-138.
pubmed doi - Kyoshima K, Horiuchi T, Zenisaka H, Nakazato F. Thoracic dumbbell intra- and extramedullary schwannoma. J Clin Neurosci 2005;12(4):481-484.
pubmed doi - Kumar S, Rafiq MU, Ahamed I, Ansari J, Cowen ME. Asymptomatic giant thoracic schwannoma. Ann Thorac Surg 2006;82(3):e26.
pubmed doi - Hagiwara K, Higa T, Miyazato H, Nonaka S. A case of a giant schwannoma on the extremities. J Dermatol 1993;20(11):700-702.
pubmed - Stout AP. The peripheral manifestation of the specific nerve sheath tumor (neurilemmoma). Amer J Cancer 1935; 24: 751–96.
- Georghiou GP, Vidne BA, Boikov O, Saute M. Giant schwannoma of the posterior mediastinum. Eur J Cardiothorac Surg 2003;24(6):1030.
pubmed doi - Kara M, Ozkan M, Sak SD, Aksu O, Kavukcu S. Giant ancient schwannoma of the posterior mediastinum cytologically misdiagnosed as a malignant tumour. A case report. Acta Chir Belg 2002;102(6):464-466.
pubmed - Naganska E, Matyja E, Mossakowski Z, Zabek M. Giant cervico-thoracic schwannoma with long clinical history. Case report. Folia Neuropathol 1999;37(3):185-188.
pubmed - Lucas S, Cendan E, Auque J, Civit T, Caremelle S, Braun D. [Asymptomatic giant thoracic dumbbell neurinoma. Apropos of a case]. J Chir (Paris) 1992;129(2):81-87.
pubmed - Zadeh G, Buckle C, Shannon P, Massicotte EM, Wong S, Guha A. Radiation induced peripheral nerve tumors: case series and review of the literature. J Neurooncol 2007;83(2):205-212.
pubmed doi - Morbidini-Gaffney S, Alpert TE, Hatoum GF, Sagerman RH. Benign pleural schwannoma secondary to radiotherapy for Hodgkin disease. Am J Clin Oncol 2005;28(6):640-641.
pubmed doi - Kochbati L, Boussen H, Benna F, Belhaj Ali Z, Gammoudi A, Bouaouina N, Besbes M, et al. [Second malignancies following Hodgkin's disease treatment in Tunisia. Retrospective study of 26 cases observed at the institute Salah-Azaiz]. Cancer Radiother 2003;7(5):302-307.
pubmed doi - Grudeva-Popova J, Goranov S, Kumchev I. Third malignancy after treatment of Hodgkin's disease. Folia Med (Plovdiv) 1999;41(2):13-15.
pubmed - Fenzi F, Moretto G, Zamboni G, Passarin MG, Rizzuto N. Brain metastases from post-radiation malignant peripheral nerve sheath tumour. Ital J Neurol Sci 1995;16(7):495-498.
pubmed doi - Watine O, Morel P, Bauters F, Ribet M. [Thoracic tumors after treatment for Hodgkin disease]. Ann Chir 1995;49(3):225-231.
pubmed - Fisher PM, Dodwell DJ, Bridges LR, Cartwright SC, Stone J. Malignant schwannoma following treatment for Hodgkin's disease. Clin Oncol (R Coll Radiol) 1994;6(3):204-205.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


