| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 6, December 2012, pages 334-336
Pleomorphic Hyalinising Angiectatic Tumour: A Tumour Diagnosis of Suspicion
Stratos Sofosa, b, Hamid Tehrania, Hassan Shaabana
aWhiston Hospital, Warrington Road, Prescot, Merseyside, L35 5DR, UK
bCorresponding author: Stratos Sofos, Whiston Hospital, Warrington Road, Prescot, Merseyside, L35 5DR, UK
Manuscript accepted for publication February 14, 2012
Short title: A Tumour Diagnosis of Suspicion
doi: https://doi.org/10.4021/jmc573w
| Abstract | ▴Top |
A 62 year old male was referred to our service complaining of a 5 year history of a painful, erythematous swelling on the proximal third of his right tibia. A previous MRI scan displayed appearances suggested to be consistent with fat necrosis, erythema nodosum or pretibial myxoedema. On examination there was an ill-defined, soft, subcutaneous mass on the right anterior leg measuring approximately 30mm x 40mm in diameter. The overlying skin was warm to palpation and mildly tender but with no epidermal changes. There were no associated neurovascular signs or lymphadenopathy. An incisional biopsy revealed histological features highly suggestive of Pleomorphic Hyalinizing Angiectatic Tumour (P.H.A.T). Wide local excision of 3cm margin (90 x 85mm) was subsequently performed with split skin graft reconstruction. The patient remains recurrence-free at 1 year post surgery. Pleomorphic Hyalinizing Angiectatic Tumour is an unusual, highly vascular soft tissue tumour, usually occurring in the subcutis of the lower extremity. Differential diagnoses include neurilemoma and malignant fibrous histiocytoma and, as illustrated by this case report, erythema nodosum or even pretibial myxoedoema. Clinical suspicion of PHAT should initiate MRI scan and incision biopsy. Current literature suggests that, due to a 20-33% rate of local recurrence, P.H.A.T should be treated by wide local excision by a 3cm margin and is to include deep fascia, down to periosteum. It should be reviewed regularly as reports of multiple recurrences 25 years after excision suggest that life-long review may be prudent.
Keywords: Pleomorphic; Hyalinising; Angiectatic; Tumour
| Introduction | ▴Top |
Pleomorphic Hyalinizing Angiectatic Tumour (PHAT) is a rare soft tissue tumour of which there have been approximately fifty cases reported and was first described in 1996 in the American Journal of Surgical pathology. Its diagnosis requires a high index of suspicion and as it has a high rate of recurrence, it requires lifelong follow up. It commonly occurs on the lower limbs and so may present to either skin cancer specialist or Orthopaedic clinic. It can genuinely be misdiagnosed as they are subtle and resemble various other common skin conditions. We present a case in which diagnosis of such a tumour was made following incisional biopsy after an inconclusive MRI scan.
| Case Report | ▴Top |
A 62 year old male, diabetic lorry driver was referred to our plastic surgery clinic, with a 5 year history of a painful, erythematous swelling on the proximal third of his right tibia. He had had an MRI scan performed a year previously when seen by the orthopaedic team, which showed thickening of the subcutis overlying the right tibia with appearances resembling fat necrosis, erythema nodosum or pretibial myxoedema. On examination there was an ill defined, soft, subcutaneous mass on the right anterior leg measuring approximately 30mm x 40 mm in diameter. The overlying skin was warm to palpation and mildly tender but with no epidermal changes (Fig. 1).
 Click for large image | Figure 1. Pre-operative photograph of lesion showing raised lesion on proximal third of right tibia. |
There were no associated neurovascular signs or lymphadenopathy. An incisional biopsy was performed, revealing histological features highly suggestive of Pleomorphic Hyalinizing Angiectatic Tumour (P.H.A.T) (Fig. 2).
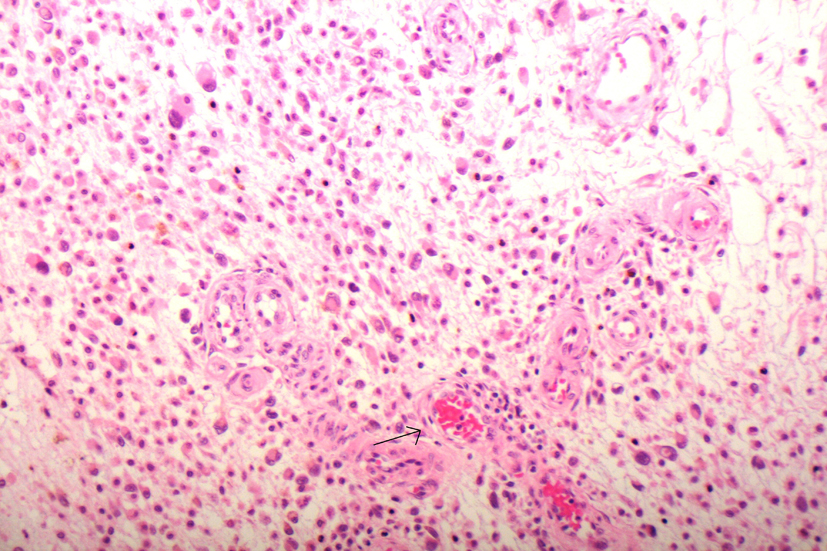 Click for large image | Figure 2. High power view showing diffusely infiltrative tumour which is located in the subcutaneous tissue. The tumour is composed of tightly grouped vessels with thick walls and sheets of spindled and plump neoplastic cells with abundant stippled haemosiderin within the cytoplasm. Many of the cells show marked nuclear pleomorphism and hyperchromasia (arrow) with frequent intranuclear pseudoinclusions. |
Staining was positive to CD34 and showed patchy positivity with S100 and CD68. Staining with SMA was equivocal; Desmin and Melanin A stains were negative. Wide local excision was subsequently performed with split skin graft reconstruction. We avoided a flap reconstruction due to the patient’s diabetic status, varicose veins and previous fracture on the affected leg. The patient remains recurrence-free at 1 year post surgery.
| Discussion | ▴Top |
Pleomorphic Hyalinizing Angiectatic Tumour is an unusual, highly vascular soft tissue tumour, usually occurring in the subcutis of the lower extremity [1]. Clinical evidence shows presentation ranging between the ages of 10-83 and local recurrence rates of up to 20-33% [2, 3]. Whilst the malignant potential of PHAT is still uncertain, we were unable to locate any reports of metastatic dissemination. In a clinicopathologic study by Ke et.al, the P.H.A.T showed the neoplastic cells to be positive for vimentin, CD34, CD99, and VEGF, but negative for S-100 protein, desmin, SMA, and CD31. In all the cases, the MIB-1 proliferative activity of the neoplastic cells was lower than 2%. Ultrastructural analysis did not reveal any evidence of specific differentiation. Aneuploidy was not detected by flow cytometry [4]. Differential diagnoses include neurilemoma and malignant fibrous histiocytoma [4] and, as illustrated by this case report, erythema nodosum or even pretibial myxoedoema.
Clinical suspicion of PHAT should initiate MRI scan and incision biopsy. Based on current literature suggesting a propensity for local recurrence, we suggest that P.H.A.T should be treated by wide local excision down to fascia, with margins varying depending on the size of the lesion and after an MDT consensus. The lesion should be reviewed regularly as the mean recurrence is 20% [3] and reports of multiple recurrences up to 25 years after excision [5] suggest that life-long review may be prudent.
Acknowledgments
We are grateful for the assistance of Dr Sheila Kelly in the diagnosis and provision of histological images of the P.H.A
Conflict of Interest
None
Role of the funding Source
None
| References | ▴Top |
- Weiss SW, Goldblum JR. Enzinger and Weiss's Soft Tissue Tumors, 4th edition, 2001.
- Folpe AL, Weiss SW. Pleomorphic hyalinizing angiectatic tumor: analysis of 41 cases supporting evolution from a distinctive precursor lesion. Am J Surg Pathol. 2004;28(11):1417-1425.
pubmed doi - Iascone C, Sadighi A, Ruperto M, Paliotta A, Borrini F, Mingazzini P. Pleomorphic hyalinizing angiectatic tumour of the mesorectal soft tissue. A case report and review of the literatre. Chir Ital. 2008;60(1):159-163.
pubmed - Ke Q, Erbolat, Zhang HY, Bu H, Li S, Shi DN, Yang GH, et al. Clinicopathologic features of pleomorphic hyalinizing angiectatic tumor of soft parts. Chin Med J (Engl). 2007;120(10):876-881.
pubmed - Smith ME, Fisher C, Weiss SW. Pleomorphic hyalinizing angiectatic tumor of soft parts. A low-grade neoplasm resembling neurilemoma. Am J Surg Pathol. 1996;20(1):21-29.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


