| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 3, June 2012, pages 190-192
Hypoglycemic Encephalopathy Caused by Insulin Aspart (Novorapid ®) Overdose During a Suicide Attempt
Makoto Onoderaa, b, Yasuhisa Fujinoa, Yoshihiro Inouea, Tatsuyori Shozushimaa, Satoshi Kikuchia, Shigeatsu Endoa
aDepartment of Critical Care Medicine, Iwate Medical University, Japan
bCorresponding author: Makoto Onodera, 19-1 Uchimaru, Morioka, Iwate 020-8505, Japan
| Abstract | ▴Top |
We present a case of a 41-year-old man who attempted suicide by injection of 600 units of insulin aspart. On arrival at the ER (after eating high-carbohydrate foods), he was awake and blood glucose was 40 mg/dl. He received a total glucose load of 230 g in the first 15 hours. Head CT was not remarkable. He was discharged on day 14. Three weeks later, he was found in a deep coma. He had injected 900 units of insulin aspart in a suicide attempt 8 hours prior to be found. On arrival, he was comatose and his blood glucose was 19 mg/dl. Head CT revealed low density areas throughout the cerebral cortex and partial cerebral edema. He received a total glucose load of 270 g in the first 22 hours. A repeat head CT examination on day 9, revealed worsening of the findings throughout the cerebral cortex. He fell into an apallic syndrome and was transferred to a local hospital. In the second overdose, the patient rapidly developed a sustained hypoglycemia, and fell into hypoglycemic encephalopathy because of the delay in receiving appropriate treatment. We consider that insulin aspart overdose may, in fact, predispose to hypoglycemic encephalopathy compared with long-acting insulin.
Keywords: Rapid-acting insulin; Acute poisoning; Diabetes Mellitus
| Introduction | ▴Top |
Reports of intentional massive overdoses of rapid-acting insulin are infrequent [1-4]. No case reports are found in the literature documenting hypoglycemic encephalopathy caused by rapid-acting insulin overdose. Here, we report a case of hypoglycemic encephalopathy caused by insulin aspart (NovoRapid ®) overdose during a suicide attempt.
| Case Report | ▴Top |
A 41-year-old man with type 2 diabetes mellitus had been receiving insulin for 9 years. His additional past medical history was notable for depression for which he had been treated with antidepressant agents. He presented to our emergency center 3 h after attempting suicide by insulin overdose. He injected 600 units of insulin aspart, cut off his left fifth finger, and had subsequently eaten high-carbohydrate foods. On arrival, vital signs were within normal range. He was awake, alert, and without any focal deficits. Blood glucose was 40 mg/dl. The laboratory data revealed leukocytes of 12,480/mm3 and serum potassium of 2.9 mEq/l. Other laboratory results were not remarkable. Head CT was not remarkable. First, he was administered a bolus of 40 ml intravenous 50% dextrose. A continuous infusion of 10% dextrose was required to maintain the blood glucose concentration between 100 and 200 mg/dl. Supplemental dextrose was needed for glucose values < 80 mg/dl and he required intermittent bolus therapy during the first 15 h (Fig. 1 Top). He received a total glucose load of 230 g during these 15 h. His left fifth finger was amputated and a psychiatrist was consulted to evaluate his psychiatric problem; anti-anxiety drugs were prescribed. The patient was deemed medically stable and was discharged on day 14.
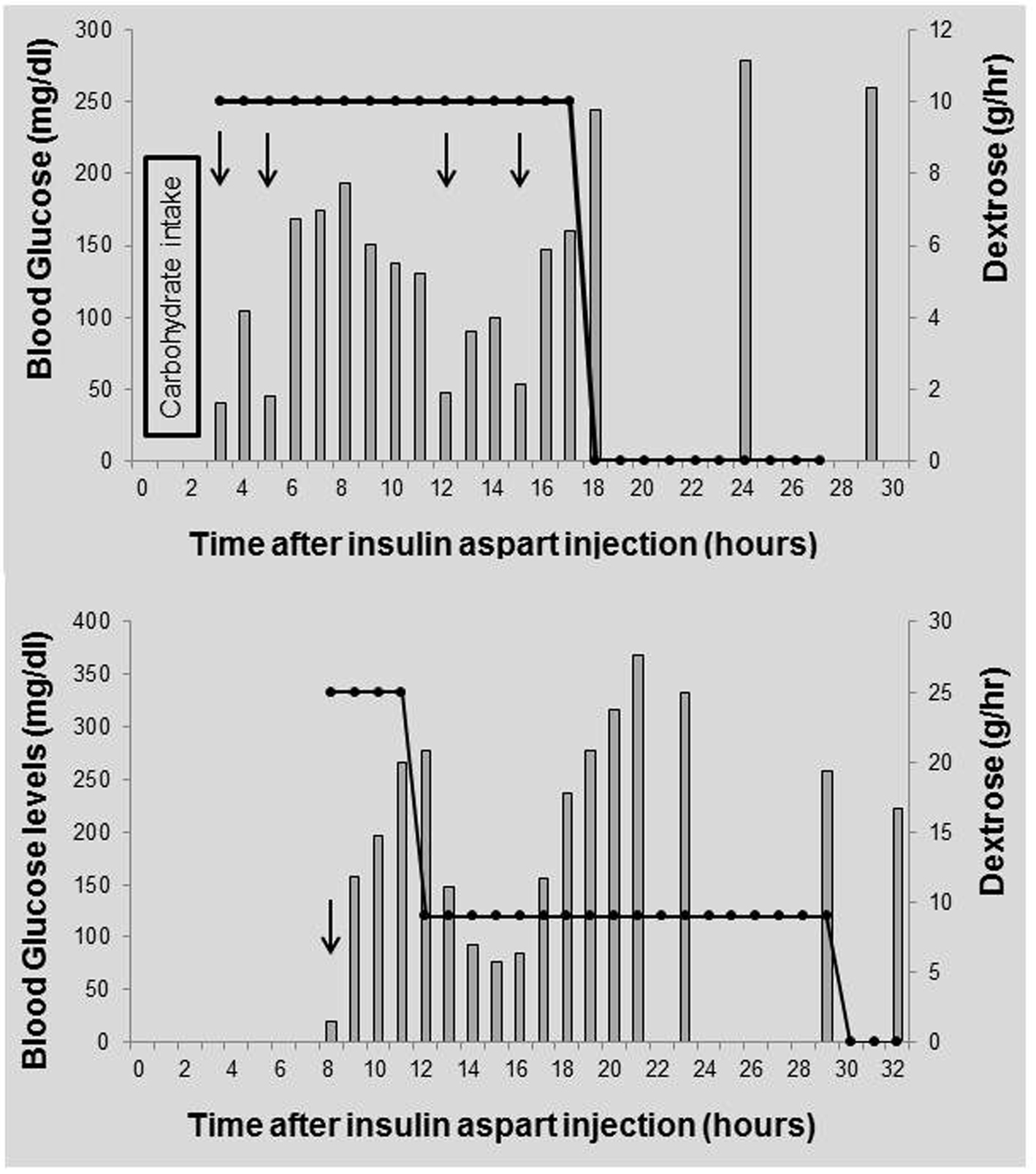 Click for large image | Figure 1. Top: Time in hours from insulin aspart overdose to our emergency center during the first suicide attempt. Bottom: Time in hours from insulin aspart overdose to our emergency center during the second suicide attempt. Bars indicate blood glucose levels, the line corresponds to infusion of dextrose, and arrows indicate receipt of 50% dextrose. |
Three weeks later, he was found in a deep coma by family. On arrival, he was comatose. Vital signs were as follows: blood pressure 166/120 mmHg, temperature 37.5 degrees Celsius, and pulse 110/minute. Blood glucose was 19mg/dl. The laboratory data revealed leukocytes of 21,670/mm3 and serum creatine phosphokinase of 4315 IU/l. Careful history taking revealed that he had injected 900 units of insulin aspart in a suicide attempt approximately 8 h before being found. Head CT revealed low density areas throughout the cerebral cortex and partial cerebral edema. He was given an intravenous bolus of 40 ml 50% dextrose and a continuous infusion of 50% dextrose was started at a rate of 25 g/h during the first 4 h period after admission. Over the next 18 h, he received a dextrose infusion at 10 g/h (Fig. 1 Bottom). He received a total glucose load of 270 g in the first 22 h. He was given intravenous infusion of 400 ml isosorbide every day for cerebral edema, but his level of consciousness never improved. Head CT examination on day 9 revealed worsening findings throughout the cerebral cortex. Unfortunately, he fell into an apallic syndrome. He was transferred to a local hospital on day 49.
| Discussion | ▴Top |
Our case is unique in that the clinical outcome differed between the first insulin aspart overdose and the second insulin aspart overdose. Rapid-acting insulin (insulin aspart) exists in solution as a monomer, which allows a higher rate of absorption from the subcutaneous sites of injection. Longer-acting insulin is formulated as multimers, which, after subcutaneous injection, will slow down the absorptive process and the postprandial peak [1]. Due to the nature of these different molecular forms, a patient who sustains a rapid-acting insulin overdose may develop hypoglycemia in a much shorter time period than with a longer-acting insulin overdose. Our case arrived at the emergency center after having eaten high-carbohydrate foods shortly after the first overdose. Similar to our report, there is a case report in which the patient had taken a meal after insulin overdose, and was conscious upon arrival to the emergency facility [1]. Therefore, a patient who sustains a rapid-acting insulin overdose can quickly develop hypoglycemia and it is important to recognize this early on. Hypoglycemia may be prevented if the overdose patient has liberal access to high-carbohydrate foods.
In our case, hypoglycemia persisted at least 15 h after subcutaneous injection. Previous reports have suggested that the duration of hypoglycemia appears to depend on the amount of insulin administered [1, 5, 6]. Brvar et al. reported that intermittent hypoglycemia requiring treatment with 50% glucose was recorded three times during the 11 h after insulin overdose [2]. There are also reports of cases who injected two kinds of insulin. In one instance, a patient who injected 300 U of insulin glargine and 200 U of insulin aspart was unable to maintain blood glucose concentration normally for 5 days in spite of dextrose infusion [1]. Fromont et al. reported a case who had injected with 300 U of insulin glargine and 300 U of insulin aspart. The patient developed relapse of hypoglycemia until 30 h after injection [3]. In addition, Mork et al. reported a case who had injected with 800 U of insulin lispro and 3800 U of insulin glargine. In spite of a continuous dextrose infusion, hypoglycemia persisted for 52 h after injection [4]. The mechanism of this prolonged hypoglycemia with slower release of insulin from subcutaneous tissue remains unclear. The huge volume of insulin solution may reduce local blood flow due to compression of tissue at the injection site [2]; others have suggested a ‘depot’ effect with the actual insulin absorption diminishing due to an increase in the injection site [7].
No case reports are found in the literature documenting hypoglycemic encephalopathy by rapid-acting insulin overdose. There are previous reports of cases with rapid-acting insulin overdose that arrived at the emergency facility within 4 hours after injection and a case that arrived more than 4 hours after injection that had been given high-carbohydrate drinks and foods. In our case, hypoglycemic encephalopathy occurred at only the second overdose. He rapidly developed hypoglycemia, and fell into hypoglycemic encephalopathy presumably because of the delay in receiving proper therapy. We consider that insulin aspart overdose may predispose to the development of hypoglycemic encephalopathy more readily than overdose with long-acting insulin.
Financial Support
We declare that we have no conflict of interest and no financial support in connection with this paper.
| References | ▴Top |
- Tofade TS, Liles EA. Intentional overdose with insulin glargine and insulin aspart. Pharmacotherapy. 2004;24(10):1412-1418.
pubmed doi - Brvar M, Mozina M, Bunc M. Prolonged hypoglycaemia after insulin lispro overdose. Eur J Emerg Med. 2005;12(5):234-235.
pubmed doi - Fromont I, Benhaim D, Ottomani A, Valéro R, Molines L, Vialettes B. Prolonged glucose requirements after intentional glargine and aspart overdose. Diabetes Metab. 2007;33(5):390-392.
pubmed doi - Mork TA, Killeen CT, Patel NK, Dohnal JM, Karydes HC, Leikin JB. Massive insulin overdose managed by monitoring daily insulin levels. Am J Ther. 2011;18(5):e162-166.
pubmed doi - Samuels MH, Eckel RH. Massive insulin overdose: detailed studies of free insulin levels and glucose requirements. J Toxicol Clin Toxicol. 1989;27(3):157-168.
pubmed doi - Arem R, Zoghbi W. Insulin overdose in eight patients: insulin pharmacokinetics and review of the literature. Medicine (Baltimore). 1985;64(5):323-332.
pubmed - McIntyre AS, Woolf VJ, Burnham WR. Local excision of subcutaneous fat in the management of insulin overdose. Br J Surg. 1986;73(7):538.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


