| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 4, August 2012, pages 267-269
Idiopathic Hypertrophic Pachymeningitis as a Rare Cause of Spinal Cord Compression
Haobin Chena, Yulong Lib, Nikita Mehraa, Sheela Mehraa, David Frescoc, Joseph Paula, Chi P Cheunga, d
aDepartment of Medicine, Kingsbrook Jewish Medical Center, Brooklyn, NY 11203, USA
bDepartment of Medicine, Raritan Bay Medical Center, Perth Amboy, NJ 08861, USA
cDepartment of Pathology, Kingsbrook Jewish Medical Center, Brooklyn, NY 11203, USA
dCorresponding author: Chi P Cheung, Department of Medicine, Kingsbrook Jewish Medical Center, 585 Schenectady Avenue, Brooklyn, NY 11203, USA
Manuscript accepted for publication April 4, 2012
Short title: Idiopathic Hypertrophic Pachymeningitis
doi: https://doi.org/10.4021/jmc637w
| Abstract | ▴Top |
Hypertrophic pachymeningitis is a chronic diffuse inflammatory fibrosis of dural mater. We herein report a rare case of spinal cord compression caused by idiopathic spinal hypertrophic pachymeningitis. A 49-year-old man, with a history of HIV infection, presented with worsening thoracic back pain and right leg pain for one year. A continuous epidural mass from T1 to T4 and a second ventral epidural mass at L5 were found on the MRI scan of the spine. Laminectomy and spinal cord decompression were performed, and the histopathology reported fibrosis with mixed inflammatory cellular infiltrates in the dural mater without any evidence of mycobacterial and fungal infection. The diagnosis of idiopathic spinal hypertrophic pachymeningitis was concluded. He received steroids therapy and recovered full neurological functions. The existing English literature on this rare disease was reviewed and discussed.
Keywords: Dural mater; Spinal cord; Fibrosis
| Introduction | ▴Top |
Spinal cord compression is a serious disease. Hypertrophic pachymeningitis, a chronic diffuse inflammatory fibrosis of dural mater, is an uncommon cause of spinal cord compression. This disease was first described by Charcot and Joffroy in the 19th century, and infections (e.g., tuberculosis, syphilis or fungi) were often the causes in the past. We report herein a rare case of idiopathic spinal hypertrophic pachymeningitis (ISHP) in a patient with HIV and hepatitis B infections, and the existing literature on this disease was reviewed.
| Case Report | ▴Top |
A 49-year-old African-American man presented with thoracic back pain and right leg pain for one year. The pain was aggravated by prolonged walking and standing without any change in bowel and urination habits. Past medical history was significant for HIV infection for 10 years. The HAART therapy (Prezista, Norvir, and Truvada) was discontinued 3 months before the presentation because of appearance of jaundice. On physical evaluation, he had icteric sclera and palpable liver edge that was soft and non-tender. In addition, there was tenderness around the T3 vertebrae and decreased range of motion at the back and right leg. Straight leg test was positive on the right side, but strength and sensation in the extremities remained intact.
His initial laboratory work reported total bilirubin 6.5 mg/dL, direct bilirubin 3.8 mg/dL, alanine aminotransferase 275 U/L and aspartate aminotransferase 162 U/L. HIV virus load was 198,322, and CD4 count 281 cells/µL (normal: 490 - 1740 cells/µL). Hepatitis panel was positive for hepatitis B core antibody only, indicating hepatitis B infection. Antinuclear, anti-mitochondrial, cryptococcal and toxoplasma IgM antibodies were all negative. Rapid plasma reagin test was nonreactive. MRI scan of spine found an epidural mass from T1 to T3 and a second ventral epidural mass at L5, both of which compressed the corresponding level of spinal cord (Fig. 1).
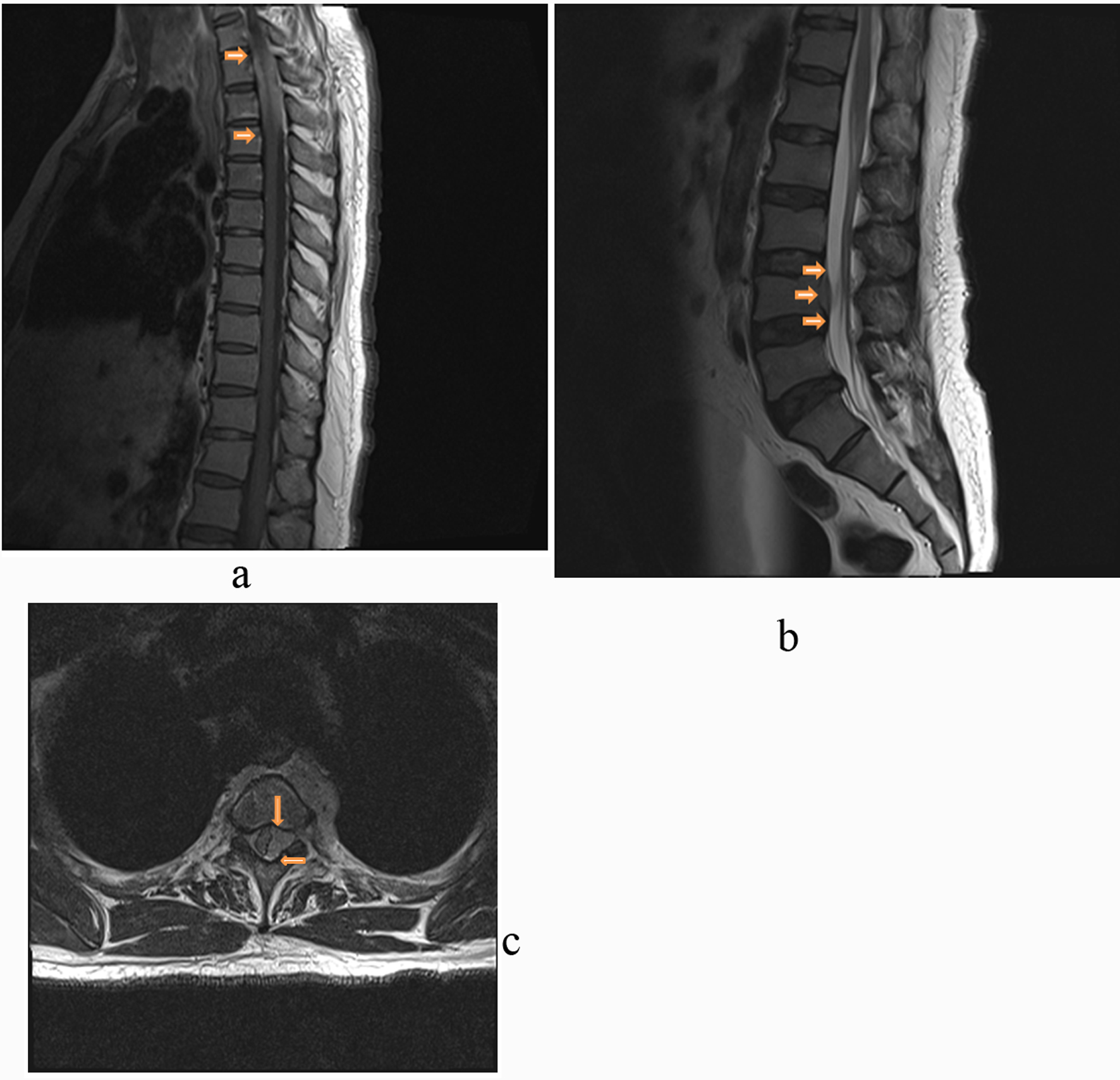 Click for large image | Figure 1. Hypertrophic pachymeningitis shown on MRI of spine with gadolinium contrast. A) Prominent abnormal enhancement infiltrated epidural space from T1 to T3, shown in the T1-weighted post-gadolinium sagittal image of thoracic spine. B) Prominent abnormal enhancement at ventral side at L4, shown in the T2-weighted post-gadolinium sagittal image of lumbar spine. C). Abnormal soft tissue on the left lateral side with mass effect on spinal cord, shown in the T2-weghted post-gadolinium transverse image at the thoracic T3. Arrows point to the thickened dura. |
Lymphoma was suspected and a T3 dorsal laminectomy was performed. Intraoperatively, a pale whitish mass continuous with the dura covering of left T3 nerve root was found. After a partial left facetectomy, the mass was found to extend beyond the left-side foramen. Debulking of the mass was carried out and the left T3 nerve root skeletonized. The pathology reported fibrosis with mixed inflammatory cellular infiltrates in the dural mater (Fig. 2). The staining of the specimen for acid fast bacteria and fungi was all negative. Diagnosis of idiopathic spinal hypertrophic pachymeningitis (ISHP) was concluded. Steroids therapy was administered post-operatively, and his neurological function fully recovered within three weeks. At review one year later, he was doing well.
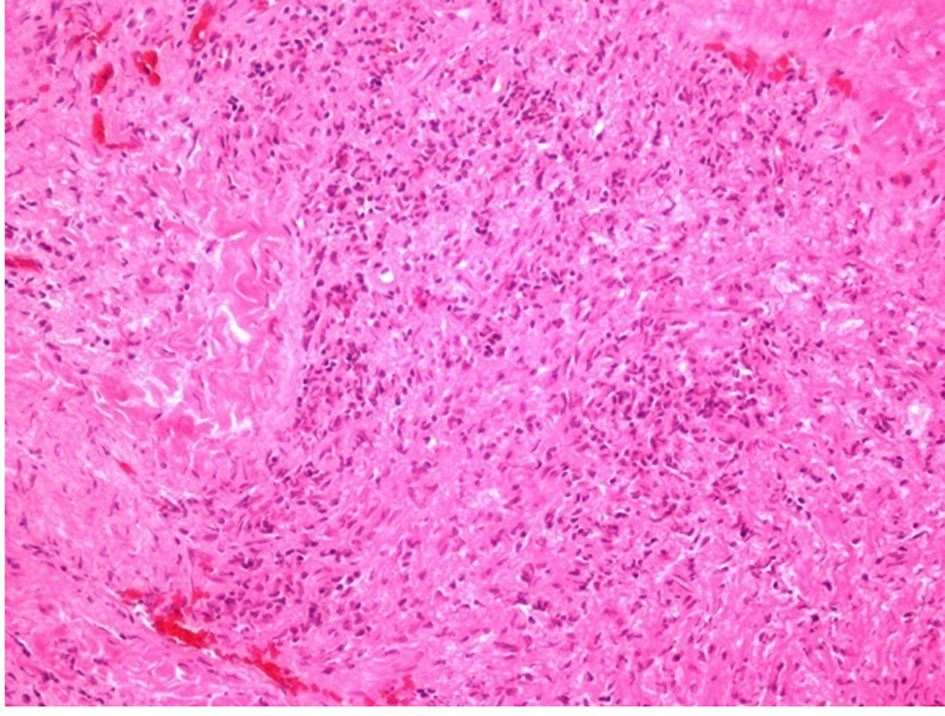 Click for large image | Figure 2. Hematoxylin and eosin staining of the excised dura mater. Fibrosis and chronic inflammation with lymphocytes and eosinophils were found. |
| Discussion | ▴Top |
Based on anatomic site, hypertrophic pachymeningitis can be classified into spinal form, intracranial form, and a combination of both. Because hypertrophic pachymeningitis was limited to spine in our case, the English literature on the spinal form of this disease with idiopathic etiology was reviewed. In total, fifteen cases (including our case) were found (see supplemental 1). Among these cases, the age of disease onset ranges from 28 to 68 (median age 56), and female is more common to be afflicted (male/female ratio: 6:9). Thoracic spine (14 cases) is most commonly to be affected, followed by cervical (7 cases) and lumbar spine (2 cases). Eight cases reported ISHP at more than one anatomic spinal region.
The clinical presentations of ISHP include radicular pain, sensory disturbance, and muscle weakness/atrophy. Surprisingly, bladder and bowel dysfunction was not uncommon (8 cases). MRI is an important tool to differentiate hypertrophic pachymeningitis from other causes of spinal cord compression. A characteristic finding of hypertrophic pachymeningitis in MRI is thickened dura at multiple continuous spinal levels. In average, the dura of seven spinal levels (with a range of 2 - 11) were affected in the reported cases. Pai et al. proposed that a long extramedullary mass with low T2 signal intensity and peripheral enhancement (due to edema) is highly suggestive of this diagnosis [1]. The definite diagnosis still relies on pathology to demonstrate fibrosis and infiltration of inflammatory cells in dura mater. Infectious diseases (e.g., syphilis, fungi, tuberculosis) need to be ruled out in order to diagnose ISHP. The association of hypertrophic pachymeningitis with HIV and hepatitis infection as well as use of antiretroviral agents is unknown. To our knowledge, this is the first case that reports ISHP in patients with HIV and hepatitis B infection.
Treatment of ISHP includes surgery and steroids. Laminectomy or laminoplasty was performed to decompress spinal cord in all reported cases. After diagnosis is confirmed by histology, the main stay of treatment is steroids. It has been reported that steroids led to dramatic reduction of symptoms and complete remission, but some patients became dependent on steroids to remain in remission [2]. No alternative treatment has yet been reported. In the patients with cranial form of hypertrophic pachymeningitis, methotrexate [3] and immunosuppressive therapy (azathioprine) [4] have been tried with good results. ISHP has 33% recurrence rate, which may still be underestimated because the length of follow-up was less than one year in many reported cases. Relapse of ISHP can be treated with steroids alone without laminectomy. It is the authors' opinion that development of new therapies is necessary and methotrexate may be tried as an alternative therapy of steroids.
Conclusion
Spinal hypertrophic pachymeningitis is a chronic diffuse inflammatory fibrosis of dural mater, with a characterized finding of thickened dura at multiple spinal levels in MRI. Hypertrophic pachymeningitis should be considered as a differential diagnosis in the evaluation of spinal cord compression by an epidural mass.
Conflicts of Interest and Source of Funding
None declared.
| References | ▴Top |
- Pai S, Welsh CT, Patel S, Rumboldt Z. Idiopathic hypertrophic spinal pachymeningitis: report of two cases with typical MR imaging findings. AJNR Am J Neuroradiol. 2007;28(3):590-592.
pubmed - Claus E, Rutgers M, Sindic C, Raftopoulos C, Godfraind C, Duprez T. Remitting/relapsing idiopathic hypertrophic spinal pachymeningitidis: comprehensive imaging work-up and MR monitoring. Eur Radiol. 2005;15(1):53-58.
pubmed doi - Bosman T, Simonin C, Launay D, Caron S, Destee A, Defebvre L. Idiopathic hypertrophic cranial pachymeningitis treated by oral methotrexate: a case report and review of literature. Rheumatol Int. 2008;28(7):713-718.
pubmed doi - Kupersmith MJ, Martin V, Heller G, Shah A, Mitnick HJ. Idiopathic hypertrophic pachymeningitis. Neurology. 2004;62(5):686-694.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


