| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 2, April 2012, pages 128-129
Adherent Clot at the Esophagogastric Junction
Mustafa Yakuta, Irfan Soykana, b
aAnkara University Medical School, Ibni Sina Hospital, Department of Gastroenterology, Ankara, Turkey
bCorresponding author: Irfan Soykan, Ankara University Medical School, Ibni Sina Hospital, Department of Gastroenterology, Sihhiye, Ankara, Turkey
Manuscript accepted for publication January 13, 2012
Short title: Mallory-Weiss Syndrome
doi: https://doi.org/10.4021/jmc506e
| Abstract | ▴Top |
Mallory-Weiss syndrome is one of the causes of upper gastrointestinal bleeding and in most of the cases bleeding stops spontaneously and requires no intervention. However, in some patients bleeding does not stop and may require therapeutic intervention in order to control active bleeding. Herein, we report a case of Mallory-Weiss syndrome with adherent clot whose bleeding was controlled with injection sclerotherapy.
Keywords: Mallory-Weiss syndrome; Gastrointestinal bleeding; Sclerotherapy
| Introduction | ▴Top |
Mallory-Weiss syndrome is defined as longitudinal mucosal lacerations located in the distal esophagus and gastric cardia. It is usually associated with forceful retching and often leads to gastrointestinal bleeding from submucosal arteries. The prevalence of Mallory-Weiss syndrome in patients presenting with gastrointestinal bleeding is approximately 5%. Although pathogenesis of this syndrome is not clear, it is usually associated with a sudden increase in intraabdominal pressure leading to mucosal laceration and eventullay may cause gastrointestinal bleeding from submucosal arteries [1]. Therefore, acute gastrointestinal bleeding, nausea, vomiting with or without epigastric pain are the major clinical manifestations. Although the amount of bleeding is usually low and majority of cases heal spontaneously, massive hemorrhage requiring transfusions and deaths may occur.
| Case Report | ▴Top |
A 63-year old patient was admitted to endoscopy unit due to haematemesis after a-day of severe nausea and retching. On physical examination, his appaearance was pale, his body temperature was 37.0 °C , his blood pressure was 100/60 mmHg, and pulse rate was 105 beats/min. He had normal breath and heart sounds, and no skin lesions were observed. An urgent upper gastrointestinal endoscopy was performed which disclosed an adherent clot with blood oozing at the esophagogastric junction (Fig. 1). The bleeding was stopped by epinephrine (1:10.000 dilution) injection. Second-look endoscopy 72 h after the initial endoscopy showed two cracks at the esophagogastric junction consistent with Mallory-Weiss syndrome (Fig. 2).
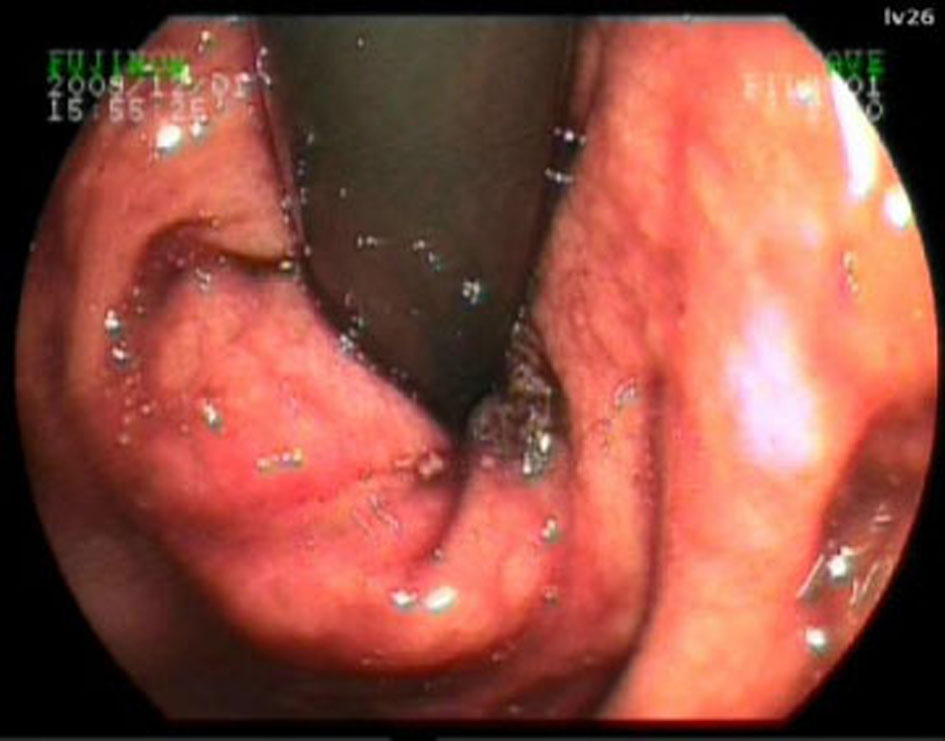 Click for large image | Figure 1. Inital endoscopy showing an adherent clot just at the esophgagogasric junction. |
 Click for large image | Figure 2. Second-look endoscopy 72 h after the initial endoscopy showed two cracks at the esophagogastric junction consistent with Mallory-Weiss syndrome. |
| Discussion | ▴Top |
Mallory-Weiss syndrome is associated with severe nausea, vomiting and retching that leads to gastrointestinal bleeding. The prevalence of Mallory-Weiss tears among patients with upper gastrointestinal bleeding is approximately 5 percent. On endoscopy, Mallory-Weiss syndrome typically presents as longitudinal tears and appears as a crack in the mucosa and occasionally covered by a clot [1]. Patients with active bleeding or signs of recent bleeding at endoscopy need immediate endoscopic therapy for hemostasis and for preventing recurrent bleeding. In most of the cases, bleeding is mild and stops spontaneously in up to 90% of patients. However, some of the patients require blood transfusion and mortality may be as high as 12% [2]. Our patient presented with hematemesis and endocopic examination revealed adherent clot and active bleeding. The bleeding was stopped by epinephrine (1:10.000 dilution) injection. Endoscopic treatment is the preferred choice of therapy in actively bleeding lacerations. Injection of various agents including epinephrine, ethanol and other sclerosants or band ligation and hemoclipping have all been used [3]. The mortality rate from Mallory-Weiss syndrome was reported as 9.7%. Some risk factors exist as significant independent predictors of the mortality in MWS patients: advanced age, low hemoglobin level, high AST and the presence of melena [4]. Therefore, we suggest that Mallor-Weiss syndrome patients with risk factors such as advanced age, low hemoglobin level and patients with active bleeding should be monitored closely and endoscopic interventions are very useful techniques in the treatment of Mallory-Weiss syndrome.
Conflict of Interest
None.
Grant Support
None.
| References | ▴Top |
- Dellon ES, Shaheen NJ. Miscellaneous diseases of the esophagus: foreign bodies, physical injury and systemic and dermatological diseases. In: Textbook of Gastroenterology, Ed: Yamada T, pp:871-888, 2009, Blackwell Publishing, UK.
- Harris JM, DiPalma JA. Clinical significance of Mallory-Weiss tears. Am J Gastroenterol. 1993;88(12):2056-2058.
pubmed - Lecleire S, Antonietti M, Iwanicki-Caron I, Duclos A, Ramirez S, Ben-Soussan E, Herve S, et al. Endoscopic band ligation could decrease recurrent bleeding in Mallory-Weiss syndrome as compared to haemostasis by hemoclips plus epinephrine. Aliment Pharmacol Ther. 2009;30(4):399-405.
pubmed doi - Fujisawa N, Inamori M, Sekino Y, Akimoto K, Iida H, Takahata A, Endo H, et al. Risk factors for mortality in patients with Mallory-Weiss syndrome. Hepatogastroenterology. 2011;58(106):417-420.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


