| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 5, October 2012, pages 308-311
Subacute Thyroiditis With Coexisting Papillary Carcinoma Diagnosed by Immediately Repeat Fine Needle Aspiration: A Case Report
Young Sik Choia, c, Bu Kyung Kima, Hye Jung Kwona, Jun Seop Leea, Jae Joon Heoa, Sang Bong Jungb, Bong Kwon Chunb
aDepartment of Internal Medicine, Kosin University College of Medicine, Busan, Korea
bDepartment of Pathology, Kosin University College of Medicine, Busan, Korea
cCorresponding author:Young Sik Choi, Department of Internal Medicine, Kosin University College of Medicine, 34 Amnam-dong, Seo-gu, Busan, 602-702, Korea
Manuscript accepted for publication May 10, 2012
Short title: Subacute Thyroiditis With Coexisting Papillary Carcinoma
doi: https://doi.org/10.4021/jmc665w
| Abstract | ▴Top |
Subacute granulomatous thyroiditis (SAT) is a spontaneously remitting inflammatory disease that is probably caused by viral infection. It has typical findings on ultrasound (US) which consist of focal ill-defined hypoechoic areas and no vascular flow in the hypoechoic areas on Doppler ultrasound. Papillary thyroid carcinoma is the most common type of thyroid cancer, and is often detected incidentally on US. However, SAT with coexisting papillary carcinoma is very rare. We report a case of SAT with coexisting papillary carcinoma diagnosed by immediate repeat US-guided fine needle aspiration (FNA). A 44-year-old woman was referred to our center for FNA of a thyroid nodule. She had anterior neck pain beginning 2 months prior to presentation and was treated at a local medical clinic. The thyroid US demonstrated a 1.2 x 0.8 cm nodule in the left lobe of the thyroid and ill-defined hypoechoic areas in both lobes of the thyroid. We performed US-guided FNA on that lesion. One week later, the cytology report was benign. Therefore, we performed repeat aspiration, which revealed papillary thyroid carcinoma. Total thyroidectomy was performed along with dissection of the central compartment of the neck and the nodule was confirmed to be papillary carcinoma without lymph node metastasis. The other portion of the thyroid showed the typical pathologic features of SAT.
Keywords: Subacute granulomatous thyroiditis; Papillary thyroid carcinoma; Repeat fine needle aspiration
| Introduction | ▴Top |
Subacute granulomatous thyroiditis (de Quervain's thyroiditis, SAT) is a self-limited inflammatory disease of the thyroid gland thought to be caused by a viral infection or a post-viral inflammatory process. The majority of patients have a history of upper respiratory tract infection [1, 2] prior to developing SAT. SAT has typical findings on ultrasound (US), which consist of focal ill-defined hypoechoic areas on gray scale US and no hypervascularity in the acute stage, with slightly increased vascularity seen in the recovery stage on color Doppler US [3-5]. SAT associated with papillary thyroid carcinoma is very rare. Only three case reports of SAT associated with papillary thyroid carcinoma have been reported in the literature [6-8].
Recently, we had a case of SAT associated with papillary thyroid carcinoma diagnosed by immediate repeat US-guided fine needle aspiration (FNA).
| Case Report | ▴Top |
A 44-year-old woman visited a local medical clinic for a routine exam. On thyroid US, a nodule in the left lobe of the thyroid was detected incidentally. She was referred to our center for FNA of the thyroid nodule. She had an upper respiratory tract infection about 3 months prior to presentation and then subsequently developed anterior neck pain 2 months prior to presentation. She was treated at a local medical clinic. Physical examination revealed diffuse enlargement and mild tenderness of the thyroid gland, and there were no palpable cervical lymph nodes. On laboratory investigation, T3 was 132.0 pg/mL, (normal range: 60 - 181 pg/mL), free thyroxine (FT4) was 1.34 ng/dL (normal range: 0.89 - 1.76 ng/dL), thyroid-stimulating hormone (TSH) was 0.06 µIU/L (normal range: 0.35 - 5.50 µIU/L), and erythrocyte sedimentation rate (ESR) was 56 mm/h (normal range: 0 - 20 mm/h). Antithyroglobulin was 155.8 U/mL (negative < 60 U/mL), antimicrosomal antibodies were 52.7 U/mL (negative < 60 U/mL), and thyrotropin-binding inhibitory immunoglobulin (TBII) was < 1 U/L (normal range: 0 - 10 U/L).
US examination was carried out using a real-time scanner (Philips Healthcare IU 22, Bothell, WA, USA) equipped with a 10 MHz linear array transducer using color Doppler imaging. The thyroid US revealed a 1.2 x 0.8 cm hypoechoic, irregularly-shaped nodule in the left lobe of the thyroid which was suspicious for malignancy and ill-defined hypoechoic areas in both lobes of the thyroid, findings compatible with SAT. Color Doppler US showed slightly increased vascularity in the hypoechoic areas (Fig. 1). An US-guided FNA of the nodule was done, and one week later, cytologic diagnosis was found to be benign. We repeated the FNA that day and the result was papillary thyroid carcinoma. Tc-99m scintigraphy showed non-visualization of both thyroid lobes and 24-hour radioactive iodine uptake was 0% (Fig. 2), which suggested destructive thyroiditis. We started oral prednisolone 20 mg per day, and the anterior neck pain and tenderness improved within several days. Total thyroidectomy was performed with dissection of the central compartment of the neck and the nodule was confirmed to be papillary carcinoma without lymph node metastasis. Pathologic finding revealed a stony hard papillary carcinoma and the other portion of the thyroid showed some scattered foci of granulomatous thyroiditis (Fig. 3). The patient was treated with 30mCi of adjuvant radioactive iodine therapy. Four months after discharge, she remains in stable condition.
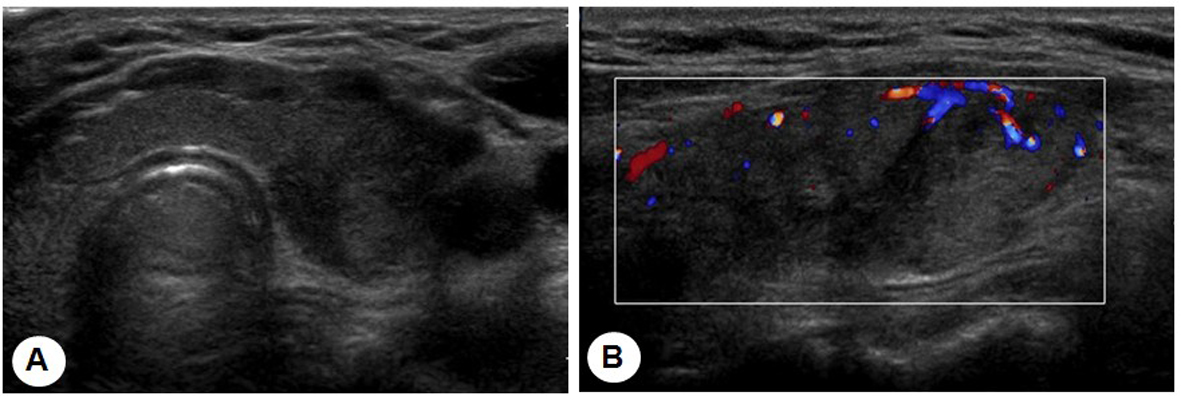 Click for large image | Figure 1. (A) The transverse and longitudinal thyroid sonograms show ill-defined hypoechoic areas in the periphery of both lobes of the thyroid and a 1.2 x 0.8 cm hypoechoic, irregularly-shaped nodule in the left lobe of the thyroid. (B) Color Doppler ultrasonography shows slightly increased vascularity in the hypoechoic areas. |
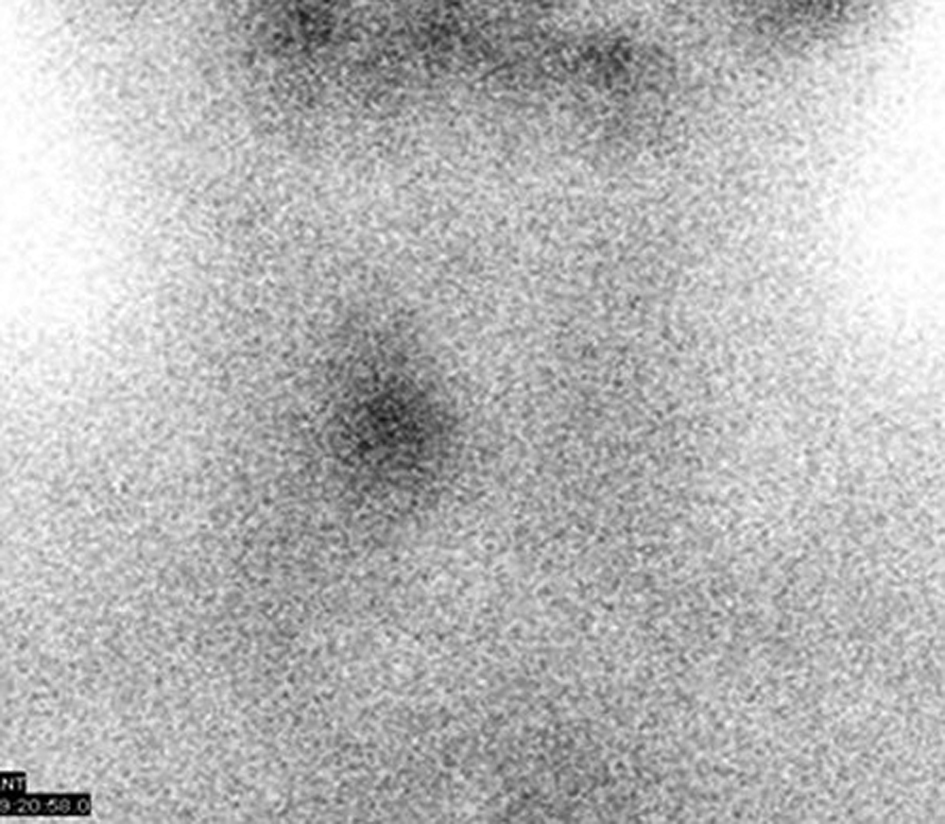 Click for large image | Figure 2. Tc-99m scintigraphy with non-visualization of the thyroid gland. |
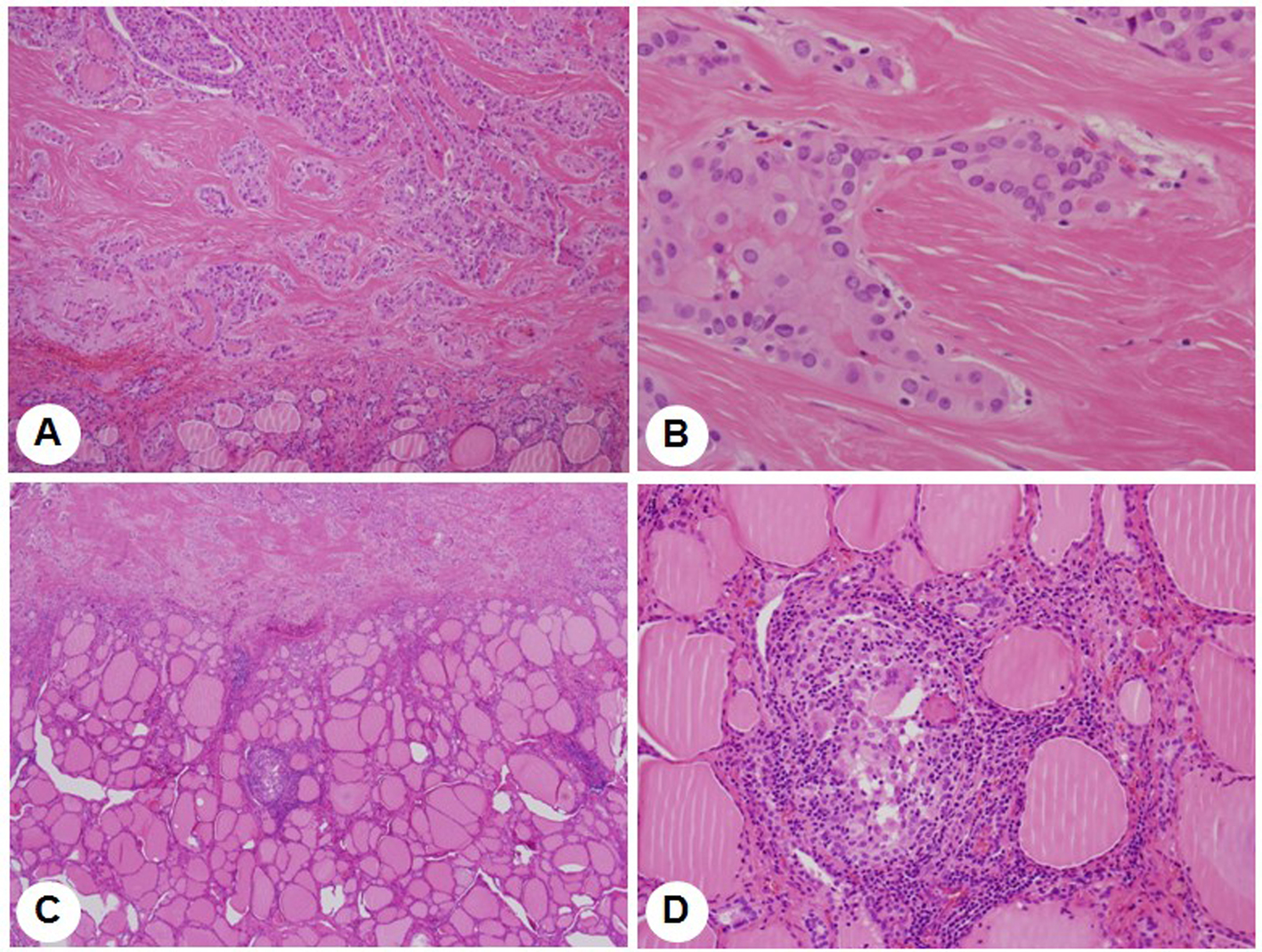 Click for large image | Figure 3. Pathological finding reveals a papillary carcinoma (A, x 40, and B, x 400, H-E stain) and a granuloma surrounded by small lymphocytes in the thyroid parenchyme (C, x 40, and D, x 200, H-E stain). |
| Discussion | ▴Top |
SAT is the most common cause of thyroid pain. However, the prognosis of SAT is excellent. More than 90% of the patients with SAT recover completely, with or without treatment. SAT is diagnosed after evaluating clinical manifestations and laboratory findings including elevated ESR, abnormal thyroid function tests, and thyroid scan with radioactive iodine uptake. Our patient had anterior neck pain, elevated ESR, and non-visualization of the gland on 99mTc thyroid scan. The first reports on ultrasonographic findings in SAT were published as early as the 1970s [9]. Several recent reports have shown that US is a useful tool for diagnosing and monitoring SAT [5, 10]. Typical gray US findings include the presence of ill-defined hypoechoic thyroid lesions without a discrete round or oval shape. Color Doppler US demonstrates no hypervascularity in the acute stage, and slightly increased vascularity is seen in the recovery stage. This suggests that US features of SAT are more useful in the acute stage. US of our patient revealed ill-defined hypoechoic areas in both lobes of the thyroid and color Doppler US showed slightly increased vascularity in the hypoechoic areas. Though our patient complained of anterior neck pain, the US findings suggested that the patient was not in the acute stage. In terms of the thyroid function tests, T3 and FT4 were normal range, which also suggests that our patient was not in the acute stage.
As thyroid US has become increasingly common, many incidental thyroid nodules are being detected. US features suggestive of thyroid cancer include the presence of microcalcifications, irregular margins, marked hypoechogenicity, nodule height greater than width, and evidence of invasion or regional lymphadenopathy. Many guidelines recommended FNA for such suspicious thyroid nodules [11, 12]. FNA of thyroid nodules is widely used as a diagnostic method in identifying malignant lesions. However, false-negative results are reported in 1.3% to 13.6% of cases. Repeat FNA may reduce the false negativity of FNA [13, 14]. However, there has been continuous debate on the management of thyroid nodules with benign cytologic results. Most guidelines suggest that benign lesions may be followed annually by US only. However, Kwak et al [15] recommend that repeat FNA should be performed for thyroid nodules that have suspicious US features, even if the initial cytologic results are benign. Timing of repeat FNA also has been debated [16]. The Bethesda System recommends that thyroid nodules with an initial fine-needle aspiration (FNA) result of non-diagnostic, unsatisfactory, or atypia of undetermined significance (AUS) be re-aspirated, but no sooner than 3 months following the initial aspiration [17].
The US features of our patient’s nodule were suspicious for malignancy. We performed US-guided FNA and the initial cytologic results were benign. Therefore, we performed immediate repeat aspiration which revealed papillary thyroid carcinoma. Although the prognosis of thyroid carcinoma is good and the growth rate of tumors is slow, patients worry about malignancy. Therefore, it is helpful to perform early repeat aspiration in patients with US features suspicious for malignancy to obtain a prompt diagnosis.
The coexistence of subacute thyroiditis and papillary carcinoma is generally regarded as coincidental. Therefore, when SAT is suspected clinically and by laboratory findings, thyroid US is a useful tool for diagnosing and monitoring this disorder and it may help identify a hidden thyroid malignancy as in this case.
| References | ▴Top |
- Fatourechi V, Aniszewski JP, Fatourechi GZ, Atkinson EJ, Jacobsen SJ. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003;88(5):2100-2105.
pubmed doi - Benbassat CA, Olchovsky D, Tsvetov G, Shimon I. Subacute thyroiditis: clinical characteristics and treatment outcome in fifty-six consecutive patients diagnosed between 1999 and 2005. J Endocrinol Invest. 2007;30(8):631-635.
pubmed - Park SY, Kim EK, Kim MJ, Kim BM, Oh KK, Hong SW, Park CS. Ultrasonographic characteristics of subacute granulomatous thyroiditis. Korean J Radiol. 2006;7(4):229-234.
pubmed doi - Zacharia TT, Perumpallichira JJ, Sindhwani V, Chavhan G. Gray-scale and color Doppler sonographic findings in a case of subacute granulomatous thyroiditis mimicking thyroid carcinoma. J Clin Ultrasound. 2002;30(7):442-444.
pubmed doi - Langer JE, Khan A, Nisenbaum HL, Baloch ZW, Horii SC, Coleman BG, Mandel SJ. Sonographic appearance of focal thyroiditis. AJR Am J Roentgenol. 2001;176(3):751-754.
pubmed - Lam KY, Lo CY. Papillary carcinoma with subacute thyroiditis. Endocr Pathol. 2002;13(3):263-265.
pubmed doi - Nishihara E, Hirokawa M, Ohye H, Ito M, Kubota S, Fukata S, Amino N, et al. Papillary carcinoma obscured by complication with subacute thyroiditis: sequential ultrasonographic and histopathological findings in five cases. Thyroid. 2008;18(11):1221-1225.
pubmed doi - Sung PS, Kim MH, Lim DJ, Choi YH, Kang MI, Cha BY, Bae JS. Subacute thyroiditis with coexisting papillary carcinoma. J Korean Thyroid Assoc. 2011;4(1):58-624.
- Blum M, Passalaqua AM, Sackler JP, Pudlowski R. Thyroid echography of subacute thyroiditis. Radiology. 1977;125(3):795-798.
pubmed - Tokuda Y, Kasagi K, Iida Y, Yamamoto K, Hatabu H, Hidaka A, Konishi J, et al. Sonography of subacute thyroiditis: changes in the findings during the course of the disease. J Clin Ultrasound. 1990;18(1):21-26.
pubmed doi - Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, Yoo HS. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002;178(3):687-691.
pubmed - Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19(11):1167-1214.
pubmed doi - Hamburger JI. Diagnosis of thyroid nodules by fine needle biopsy: use and abuse. J Clin Endocrinol Metab. 1994;79(2):335-339.
pubmed doi - Castro MR, Gharib H. Thyroid fine-needle aspiration biopsy: progress, practice, and pitfalls. Endocr Pract. 2003;9(2):128-136.
pubmed - Kwak JY, Koo H, Youk JH, Kim MJ, Moon HJ, Son EJ, Kim EK. Value of US correlation of a thyroid nodule with initially benign cytologic results. Radiology. 2010;254(1):292-300.
pubmed doi - Singh RS, Wang HH. Timing of repeat thyroid fine-needle aspiration in the management of thyroid nodules. Acta Cytol. 2011;55(6):544-548.
pubmed doi - Ali SZ, Cibas E: The Bethesda System for Reporting Thyroid Cytopathology. New York: Springer, 2009: Book Chapter 2.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


