| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 1, January 2013, pages 19-21
Swyer-James Syndrome: Disappearance of Gigantic Bullae and Pulmonary Function Improvement After Infectious Episode
Myung-Hyun Kima, Chul Min Ahna, b
aDivision of Pulmonology, Department of Internal Medicine, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea
bCorresponding author: Chul Min Ahn, 211 Eonju-ro, Gangnam-gu, Seoul, Korea
Manuscript accepted for publication June 12, 2012
Short title: Disappearance of Gigantic Bullae After Infectious Episode
doi: https://doi.org/10.4021/jmc768w
| Abstract | ▴Top |
Swyer-James syndrome is an acquired pulmonary disease following bronchiolitis obliterans in young aged children, in which characteristic unilateral hyperlucence radiologically. Frequently there are repeated pulmonary infections which cause bacterial pneumonia and bronchiectasis. It is reported no definite cause of the disease is revealed but in most cases it is thought to be inflammation and destruction of bronchioles after severe pneumonia, and it is related to measles, pertussis, tuberculosis, adenovirus, mycoplasma pneumonia, foreign body aspiration and radiation therapy. Mostly it is diagnosed at early childhood, however the detection can be delayed until later ages in asymptomatic ones. Swyer-James syndrome is a very rare disease and furthermore it is much rare to be detected in adults. Here we report a case of the disappearance of pre-existing gigantic bullae and improvement of pulmonary function in patient having Swyer-James syndrome of 65-year-old male after recovery from infected bullae with relevant literature reviews.
Keywords: Swyer-James syndrome; Gigantic bullae; Periemphysematous lung infection
| Introduction | ▴Top |
Swyer-James syndrome is a rare disease as a sequale of repeated pulmonary infections during childhood [1]. It is far rare that the disappearance of pre-existing giant bullae and pulmonary function improvement after infection in adults. In this paper we describe a patient having Swyer-James syndrome with the disappearance of pre-existing giant bullae after severe infection and improvement of pulmonary function in long term follow up.
| Case Report | ▴Top |
A 65-year-old male ex-smoker (40 pack years, quit 5 years ago) admitted to our hospital with one month of pain on left anterior chest wall and five days of dyspnea, cough and febrile event. He had a history of admission to our hospital for acute exacerbation of COPD 5 years ago and he had his case diagnosed as Swyer-James syndrome on lung ventilation-perfusion scan. He got recommendations of bullectomy but refused to get operation. He has been treated for asthma and COPD conservatively and complained of chronic dyspnea on exertion. On admission, he was ill-looking in moderate distress. Crackles, hyperresonance and dullness to percussion and auscultation were noted over the left upper lobe area. A chest radiography and computed tomography showed newly developed pleural effusion with loculated air fluid level (Fig. 1). Cultural study of blood and sputum revealed no meaningful organism. After 2 weeks of empirical intravenous antibiotics therapy and cautious medical observation, his general condition slowly improved with the decrease of crackles and dullness. Fluid analysis by invasive aspiration was not done for avoidance of catastrophic complication of bullae rupture. After discharge, patient’s respiratory symptom gradually disappeared with the continuous usage of bronchodilator, mucolytic, theophylline derivative and oral antibiotics. Patient’s pulmonary function test (PFT) 3 months after discharge showed far improved result compared with previous PFT (5 months before admission). PFT after 13 months after discharge reported no significant functional change since then (Table 1), 15 months after discharge, follow up chest radiography and computed tomography revealed disappearance of previously seen gigantic bullae and pleural fluid (Fig. 2). The patient complains no more respiratory symptoms such as cough, sputum or dyspnea on routine follow-up.
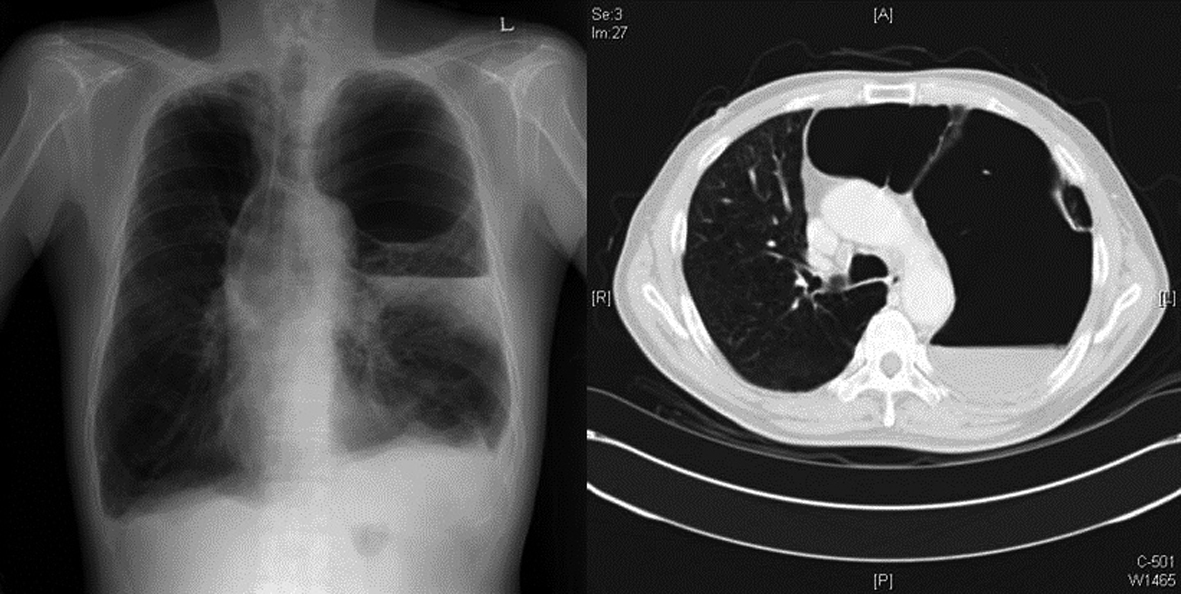 Click for large image | Figure 1. A chest radiography and computed tomography showed newly developed pleural effusion with loculated air fluid level inside the pre-existing huge bulla left sided. Shifting of cardiac border to contralateral side is seen. |
 Click to view | Table 1. Comparison of patient’s pulmonary function test |
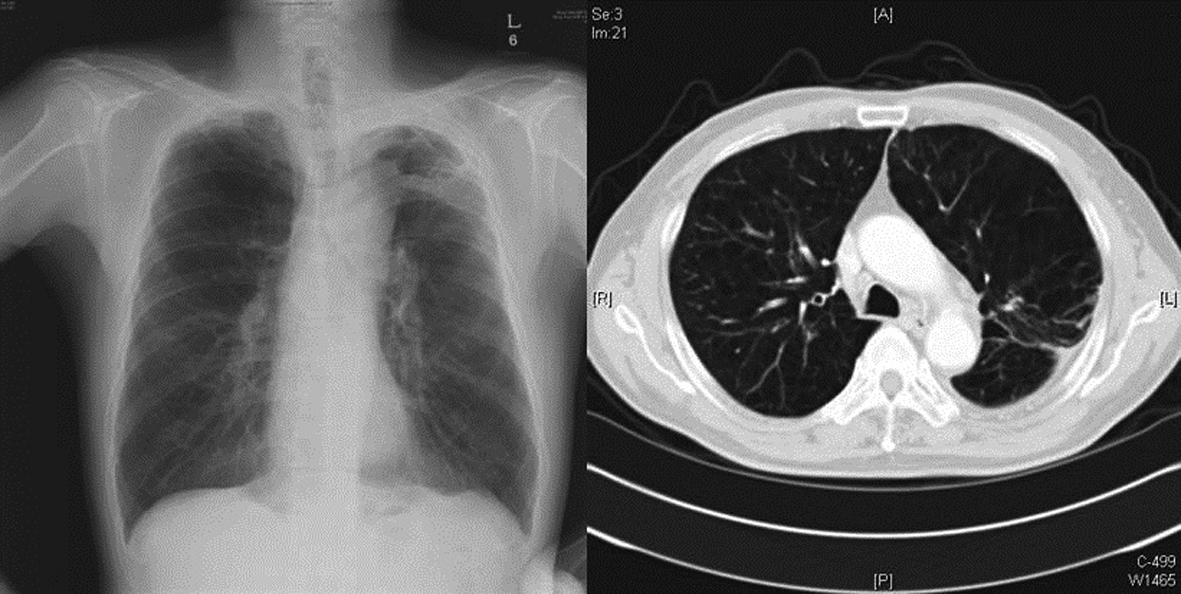 Click for large image | Figure 2. Follow up radiography and computed tomography revealed disappearance of previously seen gigantic bullae and pleural fluid (13 months after admission). Shifting of cardiac border to contralateral side became normal. |
| Discussion | ▴Top |
Swyer and James first described the radiographic entity of unilateral hyperlucent lung in 1953 [2]. Being primarily a radiological diagnosis, histopathology is not usually obtained. While the etiology is unknown, the commonest theory is of an infective bronchitis and bronchiolitis leading to obliteration of small airways. The damage to the terminal or respiratory bronchioles in early childhood possibly prohibits normal development of their alveolar buds [1]. Chest radiography shows ipsilateral hypertranslucency, with a decrease in vascular markings both at hilum and peripherally. Expiratory films typically show air trapping with a shift of the mediastinum to the contralateral side. Most patients are diagnosed at routine radiography and are asymptomatic [3]. Exertional dyspnea is occasionally described, and those with associated bronchiectasis may have a history of recurrent lower respiratory infections.
There are two possible mechanisms to explain cause of air-fluid level. One mechanism is inflammatory response from adjacent pneumonitis and the other is inflammatory mucous plugging of narrowed bronchiolar communications between in bullae and larger airways [4]. The role of antibiotics in treatment of infected bullae remains speculative, but most patients present with symptoms of acute inflammatory disease and probably benefit from antibiotic therapy. Unless the sputum demonstrates pathogenic organisms of the patient acutely ill, therapy with antibiotics is recommended [4].
There are some reports that surgical treatment is to be considered when infections cannot be controlled or repeated to patients with diffuse emphysema [5]. Lung volume reduction surgery (LVRS) is predicated upon the principle that a reduction in lung volume can favorably affect the mechanics of diaphragm, chest wall and airways. It is generally believed LVRS is a therapeutic option for patients with severe emphysema after all conservative measures have been exhausted [5]. Large bullae are often at maximal inflation and act as space-occupying regions that partially compress areas of underlying lung [6].
To our knowledge, there is rare report of Swyer-James syndrome presenting with disappearance of not only pleural effusion but huge bullae after infectious episode in non-surgically treated patient. Absorption of air and fluid during treatment lead to contracture of pre-existing bullae secondarily [7]. It causes partially auto-bullectomy state and improves lung function by increment of elastic recoil. Replacement of pre-occupying bullae by parenchymal tissue occurs [7]. Follow-up PFT revealed 102% in FVC and 114% in FEV1. It is due to loss of compressing effect of bullae to bronchus and pulmonary vasculature. In contrast to FVC, FEV1 did not reach normal value even showing dramatic increase in PFT. It may be due to pre-existing destruction of small airways in childhood in case of Swyer-James syndrome.
In summary, this report describes an old male having underlying Swyer-James syndrome that developed infected bullae and recovered. We can explain the disappearance of pre-existing huge bullae by increment of elastic recoil of the lung owing to contracture of bullae during absorption of air and fluid on recovery phase.
Conflicts of Interest
There are no conflicts of interest.
| References | ▴Top |
- Erkasar CF, Caglar CE, Koray D, Ilgin KN. Bilateral Swyer-James (Macleod's) syndrome. Indian J Pediatr. 2002;69(5):433-435.
pubmed doi - Swyer PR, James GC. A case of unilateral pulmonary emphysema. Thorax. 1953;8(2):133-136.
pubmed doi - Leahy DJ. Increased transradiancy of one lung. Br J Dis Chest. 1961;55:72-76.
pubmed - Peters JI, Kubitschek KR, Gotlieb MS, Awe RJ. Lung bullae with air-fluid levels. Am J Med. 1987;82(4):759-763.
pubmed doi - Roue C, Mal H, Sleiman C, Fournier M, Duchatelle JP, Baldeyrou P, Pariente R. Lung volume reduction in patients with severe diffuse emphysema. A retrospective study. Chest. 1996;110(1):28-34.
pubmed doi - Sciurba FC, Rogers RM, Keenan RJ, Slivka WA, Gorcsan J, 3rd, Ferson PF, Holbert JM, et al. Improvement in pulmonary function and elastic recoil after lung-reduction surgery for diffuse emphysema. N Engl J Med. 1996;334(17):1095-1099.
pubmed doi - Guimard Y, Lemmens B, Carre P, Asquier E, Lavandier M. [Disappearance of emphysematous bullae after infectious episodes]. Rev Pneumol Clin. 1995;51(4):253-256.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


