| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 6, December 2012, pages 347-351
Takotsubo Cardiomyopathy and Acute Ischemic Stroke
Alexandre Amaral-Silvaa, f, Miguel Lourencob, Renato Fernandesc, Duarte Cacelad, Joao Alcantarae
aUnidade CerebroVascular do Hospital de Sao Jose, Centro Hospitalar de Lisboa Central, EPE, Lisboa, Portugal
bNeurology Department, Hospital de Santo Espirito de Angra do Heroismo ESPR, Angra do Heroismo, Portugal
cCardiology Department, Hospital do Espirito Santo, EPE, Evora, Portugal
dCardiology Department, Hospital de Santa Marta, Centro Hospitalar de Lisboa Central, EPE, Lisboa, Portugal
eUnidade CerebroVascular do Hospital de Sao Jose, Centro Hospitalar de Lisboa Central, EPE, Lisboa, Portugal
fCorresponding author: Alexandre Amaral-Silva,Unidade CerebroVascular, Hospital de S. Jose, Rua Antonio Jose Serrano, 1150-199 Lisboa, Portugal
Manuscript accepted for publication July 10, 2012
Short title: Cardiomyopathy and Stroke
doi: https://doi.org/10.4021/jmc776w
| Abstract | ▴Top |
Takotsubo cardiomyopathy and acute ischemic stroke. The Takotsubo cardiomyopathy is characterized by transient left ventricle dysfunction, with apical ballooning in the absence of significant coronary stenosis, and may clinically mimic an acute myocardial infarction. The association between Takotsubo cardiomyopathy and several acute neurological conditions has been increasingly described. The authors present the case report of an acute stroke patient submitted to intravenous thrombolysis, whose EKG on admittance showed supra-ST deviation in DI, AVL and V2-V6 leads, with concomitant elevation of myocardial necrosis biomarkers. After intravenous thrombolysis, a cardiac catheterism was performed that showed apical ballooning and acinesia of the left ventricle with decreased ventricular function, with no significant coronaropathy. The cerebral MRI performed on the seventh day showed multiple acute infarctions in different vascular territories of the anterior and posterior circulations bilaterally. Transthoracic echocardiogram performed on the same day revealed normal ventricular function and myocardial kinetics supporting the diagnosis of Takotsubo cardiomyopathy. The patient was discharged on day 10, on hypocoagulation therapy. Takotsubo cardiomyopathy is a spontaneously reversible condition, mostly requiring supportive therapeutic measures. The acute left ventricle dysfunction characteristic of this syndrome is a potential mechanism for cardiac embolism. Acute ischemic stroke is a relatively rare but severe complication. According to this, hypocoagulant therapy must be considered especially until the ventricular function is fully recovered.
Keywords: Takotsubo cardiomyopathy; Apical ballooning; Left ventricle dysfunction; Stroke; Hypocoagulation
| Introduction | ▴Top |
Described by Sato et al [1] in 1990, Takotsubo’s cardiomyopathy is characterized by transient left ventricular dysfunction, with apical ballooning, apical hypocinesia/acinesia and basal hypercontractility, in the absence of significant coronary stenosis. It may clinically and electrocardiographically mimic an acute myocardial infarction [1, 2]. Elevation of cardiac ischemia biomarkers, usually mild and transient, can also be a feature of this condition [3]. The differential diagnosis with acute coronary syndrome is established by coronary angiography. Exclusion of other cardiovascular conditions like myocarditis, pericarditis or aortic dissection is also important. Recently diagnostic guidelines for Takotsubo’s cardiomyopathy have been published [4].
Takutsubo’s cardiomyopathy is a transient condition and normalization of left ventricular function has been described between 7 to 37 days [3]. Electrocardiographic normalization usually takes longer-19 to 219 days [5]. The prevalence of this condition has been estimated to be 0.7 to 2.5% among patients with suspected acute coronary syndrome and elevated ST-segment [3, 5, 6]. Almost 90% of all reported cases have been described in postmenopausal women reporting previous history of extreme psychological/emotional stress (80%) or in association with physical stress factors like severe trauma, surgery, severe hypoglycemia, asthma decompensation, etc. (20%) [3, 7]. Association with several neurological conditions, like seizures [8] or Guillain Barre syndrome [9], has been increasingly reported.
The authors discuss the physiopathological and temporal relation between acute ischemic stroke and Takotsubo cardiomyopathy.
| Case Report | ▴Top |
Seventy-year-old woman, with past medical history of depression, parkinsonism, arterial hypertension and dyslipidemia. No previous history of atrial fibrillation has been reported. She was on clopidogrel, indapamide, captopril, bisoprolol, transdermic nitroglycerine, levodopa/carbidopa and olanzapine. She was admitted because of right hemiparesis and motor aphasia (National Institute Health Stroke Scale Score (NIHSSS) = 6), 50 minutes after symptoms-onset. There was no previous or concomitant history of physical or psychological stress. CT scan on admittance showed no acute ischemic or hemorrhagic lesions. The patient was treated with i.v. t-PA one hour and 30 minutes after symptom-onset. EKG on admittance showed sinus rhythm, ST elevation and negative, symmetric T waves in I, AVL and V2-V6 (Fig. 1). Blood chemistry evidenced elevated myocardial necrosis biomarkers (CPK: 601U/L and troponine T: 0.9 ng/mL) and a Pro-BNP of 24855 pg/mL.
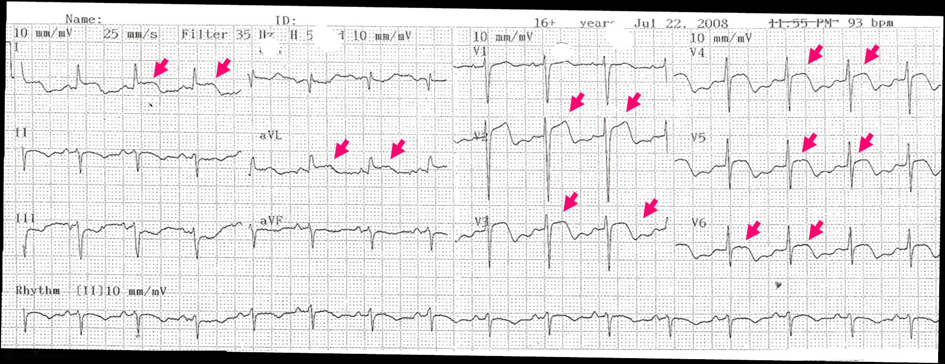 Click for large image | Figure 1. Electrocardiogram performed on admission showed supra ST deviation and inverted T waves in DI, AVL and V2-V6 leads (colored arrows). |
Neurological deterioration was observed one hour after the thrombolytic therapy have been finished - NIHSSS = 15. Another CT scan and EKG were immediately performed that were similar to the ones performed on admittance. It was decided to perform a cardiac angiography that documented apical ballooning and acinesia, basal hypercontractility and decreased left ventricular function, in the absence of coronary stenosis (Fig. 2).
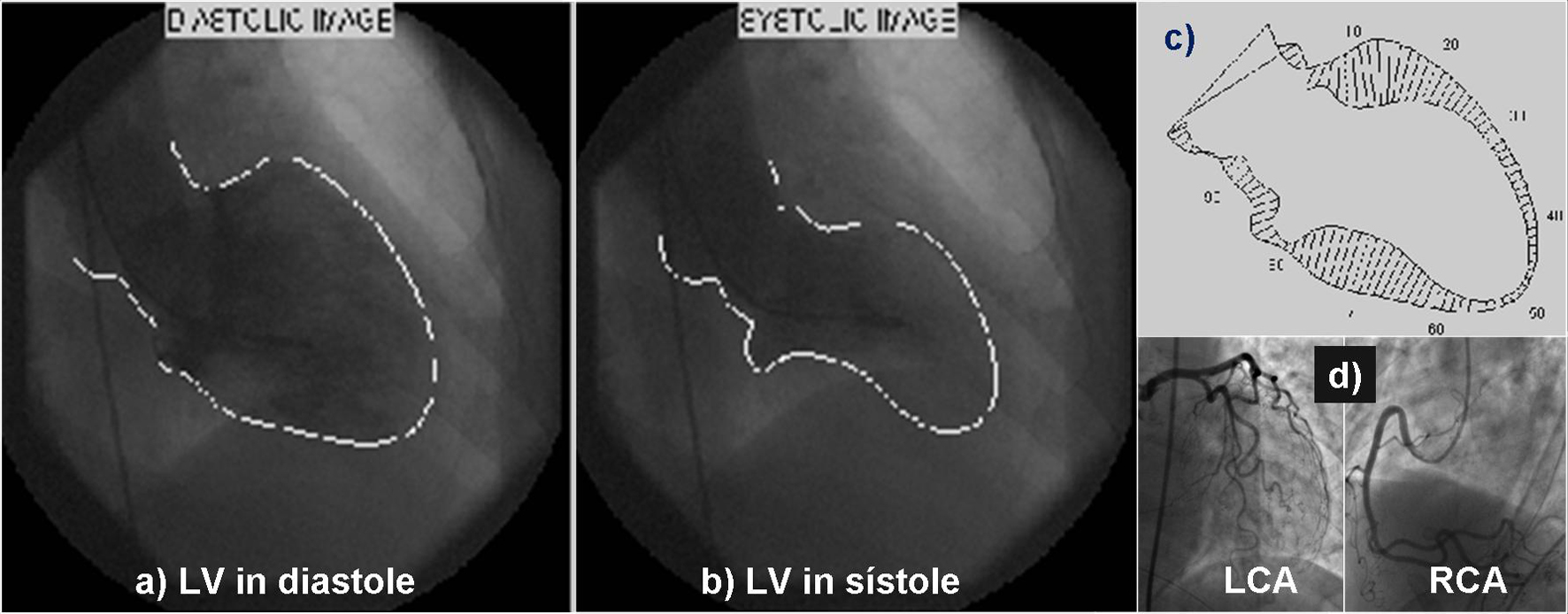 Click for large image | Figure 2. Ventriculography on diastole (a) and systole (b), showing apical ballooning and acinesia and left ventricle basal hypercontractility with compromised systolic function (c). Coronariography (d) showing no stenotic lesions in left and right coronary arteries. LV: Left ventricle, LC: left coronary artery, RC: right coronary artery. |
The control CT performed on the 3rd day showed a left temporo-parieto-occipital acute ischemic lesion and a right parasagittal hemorrhagic infarction. The cerebral MRI performed on the 7th day documented a large acute ischemic lesion in the territory of the left middle cerebral artery (MCA) and multiple small ischemic lesions in the left MCA and posterior cerebral artery (PCA) and ipsilateral cerebellar hemisphere (Fig. 3). In the same day blood chemistry showed normal cardiac biomarkers. The transesophageal echocardiogram showed no embolic sources and documented left ventricular function and myocardial kinetics normalization, supporting the diagnosis of left ventricle’s transient dysfunction. The remaining tests performed (namely carotid triplex scan and transcranial color coded duplex) were normal. Considering the probable cardioembolic etiology of stroke, and despite normalization of left ventricle’s function, it was decided to start hypocoagulation with warfarin. Regarding complications during admission, transitory hypotension requiring no specific therapeutical measures, during the first five days, has to be mentioned.
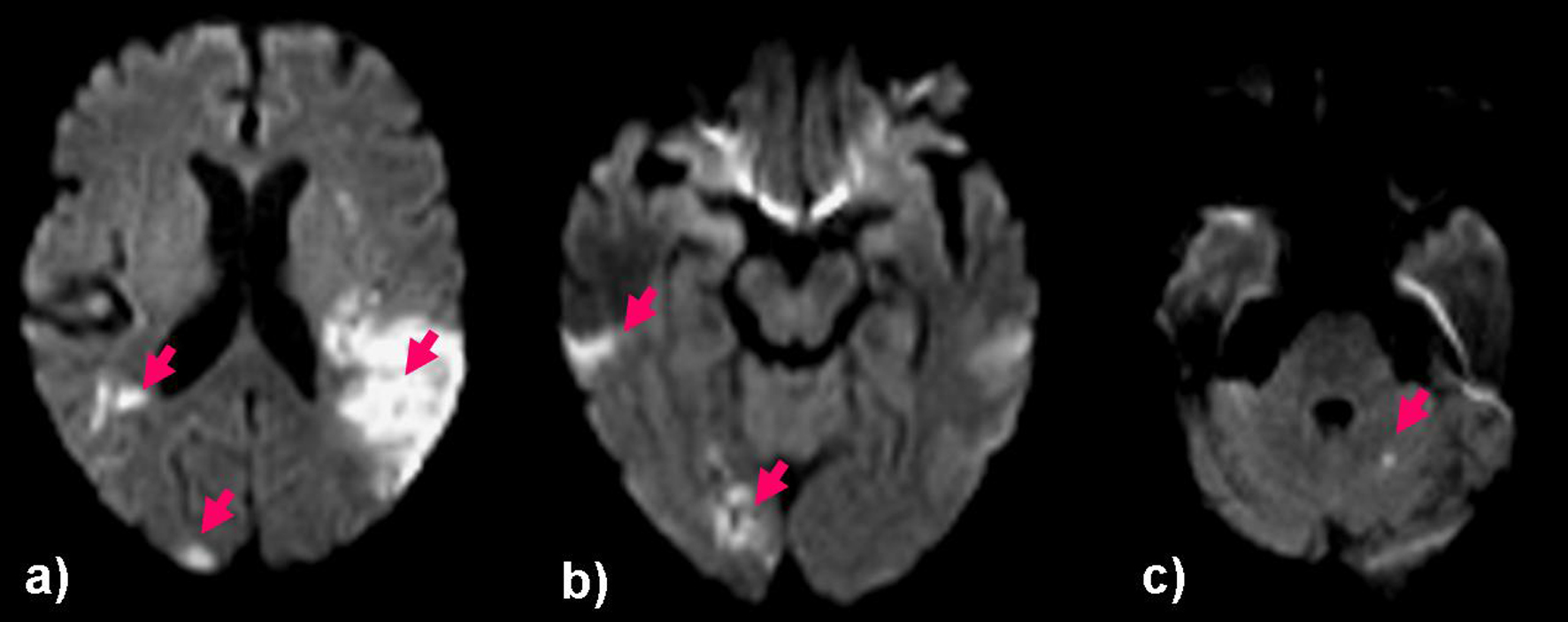 Click for large image | Figure 3. Cerebral MRI performed at the 7th day-DWI sequence-Showing multiple acute ischemic lesions: large left temporo-parietal and insular ischemic infarct (a), multiple small infarcts in right medial and posterior cerebral arteries (a, b) and small left cerebellar hemispheric infarct (c). |
Patient was discharged home on the 10th day, functionally dependent (Modified Rankin scale score = 4). No complications, cardiac or neurologic were observed during the one-year period of follow up. It was decided to stop hypocoagulation after echocardiography reevaluation performed 9 months after discharge, that showed normal left ventricle function and no embolic sources.
| Discussion | ▴Top |
The morphological features documented in the ventriculography, without evidence of coronariopathy, strongly suggest the diagnosis of Takotsubo’s cardiomyopathy. Although early administration of t-PA could be responsible for dissolving some thrombi or emboli, precluding their identification in the coronariography, complete normalization of left ventricle function in a patient with anterior wall myocardial infarction would be unlikely. Furthermore, the contractility changes documented in the ventriculography involved different coronary vascular territories making it improbable. Only multiple vessel embolization could explain this situation and this is also not likely to happen in coronary vessels.
Takotsubo’s cardiomyopathy is a spontaneously reversible condition that most often requires only general support measures. More than 95% of the patients recover completely and recurrence is rare [3, 10]. Cardiogenic shock, acute pulmonary edema, pulmonary thromboembolism, cardiac (atrial and ventricular) arrythmias and stroke are the most severe acute complications [10] and the mortality rate associated with this condition is calculated between 1 and 10%. The pathogenic mechanisms are not completely understood. Proposed mechanisms include diffuse coronary vasospasm [1, 2], changes in coronary microvascular function [11], catecholamine mediated cardiotoxicity [12], or myocarditis [7].
Acute left ventricular dysfunction is a potential mechanism of cardiac embolism. Thrombi formation in left ventricular apex is calculated to happen in about 2.5% of these patients, justifying a 0.8% incidence rate of thromboembolic complications [13].
Although, in this particular case report, there was no reference to a preceding physical or emotional stress situation, the past medical history of humor disturbance requiring chronic antidepressants treatment may represent a contributing factor to the cardiomyopathýs development. This hypothesis is strongly supported by documentation of electrocardiographic and cardiac biomarker changes immediately after hospital admission (about two hours after symptoms onset). In fact, it is well known that troponine T levels take about three to four hours to become pathologically increased even in patients with transmural myocardial infarction, therefore corroborating the proposed sequence of events. Data published in a literature review by Yoshimura et al [14] in 2008 support this hypothesis. In fact, in most of the reported patients, with stroke preceding the cardiomyopathy documentation, the clinical, laboratorial and especially electrocardiographic manifestations appeared mostly between two and a half hours and twelve days after stroke diagnosis.
The imagiological documentation of ischemic lesions in multiple vascular territories, suggesting and embolic mechanism, is another argument favoring the etiological relation between left ventricular dysfunction and stroke, even if no visible left ventricular thrombi was identified and, especially, in the absence of atrial fibrillation or other embolic sources.
Stroke associated with Takotsubo’s cardiomyopathy is usually severe [14]. As well as in our case report, more than 30% of all strokes reported in the literature, as a cause or consequence of Takotsubo’s cardiomyopathy, were associated with major neurological deficits (NIHSSS equal or superior to 15). This is true either for anterior or posterior circulation strokes [14]. Another finding reported in the literature, and observed in our patient, is the common presence of ischemic lesions in the insular area in patients with Takotsubo’s cardiomyopathy. This fact has been hypothesized to be of etiological relevance, with insular lesions probably contributing to the development of the cardiomyopathy and justifying the association between both entities [14].
Another finding to be highlighted in our case report is the significant increase in cardiac biomarkers (namely pro-BNP), especially when compared to the usual values reported in the literature [14]. This is particularly relevant once it is presently discussed the relation between the magnitude of this increase and the severity of the ventricular dysfunction [7].
Regarding the therapeutical approach, and considering the potential risk of embolic events, many authors advocate the use of hypocoagulants, at least until complete normalization of the left ventricular function. The use of these pharmacological agents is mandatory in case of intraventricular thrombus documentation [7, 15]. In our patient, it was decided not to initiate hypocoagulation immediately considering the extension of the ischemic brain lesions and the risk of hemorrhagic transformation. Treatment was started by the end of the first week. Considering the potential risk of recurrence and the fact that the patient was bedridden it was decided to maintain warfarin despite complete recovery of the left ventricular function and the absence of intra-cardiac thrombus. This treatment was stopped nine month after discharge after echocardiographic reevaluation and mild functional improvement.
Conflict of Interests
The authors declare no conflict of interests related to this manuscript.
| References | ▴Top |
- Satoh H, Tateishi H, Uchida T, Dote K, Ishihara M. Takotsubo-type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M, editors. Clinical Aspect of Myocardial Injury: From Ischemia to Heart Failure. Tokyo: Kagakuhyouronsya Co.,1990: 56-64.
- Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. [Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases]. J Cardiol. 1991;21(2):203-214.
pubmed - Pilgrim TM, Wyss TR. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review. Int J Cardiol. 2008;124(3):283-292.
pubmed doi - Kawai S, Kitabatake A, Tomoike H. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ J. 2007;71(6):990-992.
pubmed doi - Matsuoka K, Okubo S, Fujii E, Uchida F, Kasai A, Aoki T, Makino K, et al. Evaluation of the arrhythmogenecity of stress-induced "Takotsubo cardiomyopathy" from the time course of the 12-lead surface electrocardiogram. Am J Cardiol. 2003;92(2):230-233.
pubmed doi - Abdulla I, Kay S, Mussap C, Nelson GI, Rasmussen HH, Hansen PS, Ward MR. Apical sparing in tako-tsubo cardiomyopathy. Intern Med J. 2006;36(7):414-418.
pubmed doi - Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155(3):408-417.
pubmed doi - Lemke DM, Hussain SI, Wolfe TJ, Torbey MA, Lynch JR, Carlin A, Fitzsimmons BF, et al. Takotsubo cardiomyopathy associated with seizures. Neurocrit Care. 2008;9(1):112-117.
pubmed doi - Bernstein R, Mayer SA, Magnano A. Neurogenic stunned myocardium in Guillain-Barre syndrome. Neurology. 2000;54(3):759-762.
pubmed doi - Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27(13):1523-1529.
pubmed doi - Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Nakamura S, Yoshida M, et al. Time course of electrocardiographic changes in patients with tako-tsubo syndrome: comparison with acute myocardial infarction with minimal enzymatic release. Circ J. 2004;68(1):77-81.
pubmed doi - Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352(6):539-548.
pubmed doi - de Gregorio C, Grimaldi P, Lentini C. Left ventricular thrombus formation and cardioembolic complications in patients with Takotsubo-like syndrome: a systematic review. Int J Cardiol. 2008;131(1):18-24.
pubmed doi - Yoshimura S, Toyoda K, Ohara T, Nagasawa H, Ohtani N, Kuwashiro T, Naritomi H, et al. Takotsubo cardiomyopathy in acute ischemic stroke. Ann Neurol. 2008;64(5):547-554.
pubmed doi - Ramirez-Moreno JM, Bejarano-Moguer V, Elduayen J, Millan-Nunez MV, Pons-Garcia MA, Gomez MJ, Nogales-Asensio JM. [Ischemic stroke due to transient left ventricular apical ballooning in women with epilepsy debut]. Rev Neurol. 2009;48(6):333-335.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


