| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 5, May 2014, pages 260-261
Pasteurella Multocida Pneumonia: A Case of Mistaken Identity in a Previously Well 47-Year-Old Woman
Layth Alsaffara, c, Amy Jonesb
aDepartment of Microbiology, University Hospital of Wales, Heath Park, Cardiff, CF14 4XW, United Kingdom
bDepartment of Elderly Care Medicine, Llandough Hospital, Penlan Rd, Llandough, Penarth, CF64 2XX, United Kingdom
cCorresponding author: Layth Alsaffar, Department of Microbiology, University Hospital of Wales, Heath Park, Cardiff, CF14 4XW, United Kingdom
Manuscript accepted for publication November 16, 2012
Short title: Pasteurella multocida Pneumonia
doi: https://doi.org/10.14740/jmc967w
| Abstract | ▴Top |
Pasteurella infections in humans are usually zoonotic in origin, with a variety of presentations including cellulitis, septic arthritis and respiratory illness in elderly patients, the immunocompromised or those with existing chronic lung disease. We present a case of Pasteurella multocida pneumonia in a middle-aged woman with no previous lung disease and highlight a potential difficulty in the laboratory identification of Pasteurella species.
Keywords: Pasteurella pneumonia; Infection; Diagnosis
| Introduction | ▴Top |
Pasteurella multocida is a gram negative coccobacillus commonly found in the mouths of domestic and wild animals. It is estimated that 50 to 66% of healthy dogs carry the organism in their nasal secretions [1]. P.multocida cellulitis, pneumonia, bacteremia and even acute septic arthritis in humans can occur after a bite or scratch injury [2]. Since the 1980s molecular techniques have been used to further characterize the Pasteurella taxonomy and P.multocida sub-species multocida has a higher association with respiratory illnesses compared to P.multocida sub-species septica which appears to show an association with wound infections following animal bites [3]. Rarer presentations of P.multocida infections include meningitis and empyema [2, 4]. P.multocida pneumonia has been colloquially described as “cat cuddlers’ cough” and has previously most frequently been described in patients who were immunocompromised, elderly or with existing lung pathology such as chronic obstructive pulmonary disease [5]. Laboratory differentiation between Pasteurella and Hemophilus species can sometimes be difficult as both species are gram negative, coccobacilli, indole and oxidase positive. Misdiagnosis between the two species has been reported using biochemical assays [6]. In this report we present the case of a previously well 47-year-old woman who was ultimately diagnosed with P.multocida pneumonia.
| Case Report | ▴Top |
A 47-year-old woman presented to the Royal Gwent Hospital emergency unit in October 2009 with a 2-day history of headache, myalgia, chills and sweats and a 12-h history of sore throat with chest pain but no cough. At this time the UK was in the middle of the H1N1 pandemic and she had previously been started on Oseltamivir by her general practitioner on suspicion of H1N1 infection, as she had been in contact with a co-worker with a flu-like illness. The patient’s past medical history was unremarkable, she was an ex smoker (stopped 10 years ago) and on no regular medications. On examination she was pyrexial and tachycardic with a blood pressure of 137/72. Her respiratory rate was 44 breaths per minute and she was hypoxic on air. She had bi-basal crackles on auscultation, heart sounds normal with no murmurs, and there were no obvious rashes. Her ECG was normal and her chest X-ray showed left basal changes (Fig. 1). Her peripheral blood white cell count was elevated at 22.5 × 109 cells/mL (neutrophils 18.8 × 109 cells/mL). Her CRP was raised at 217 mg/L and a clinical diagnosis of a bacterial lower respiratory tract infection was made.
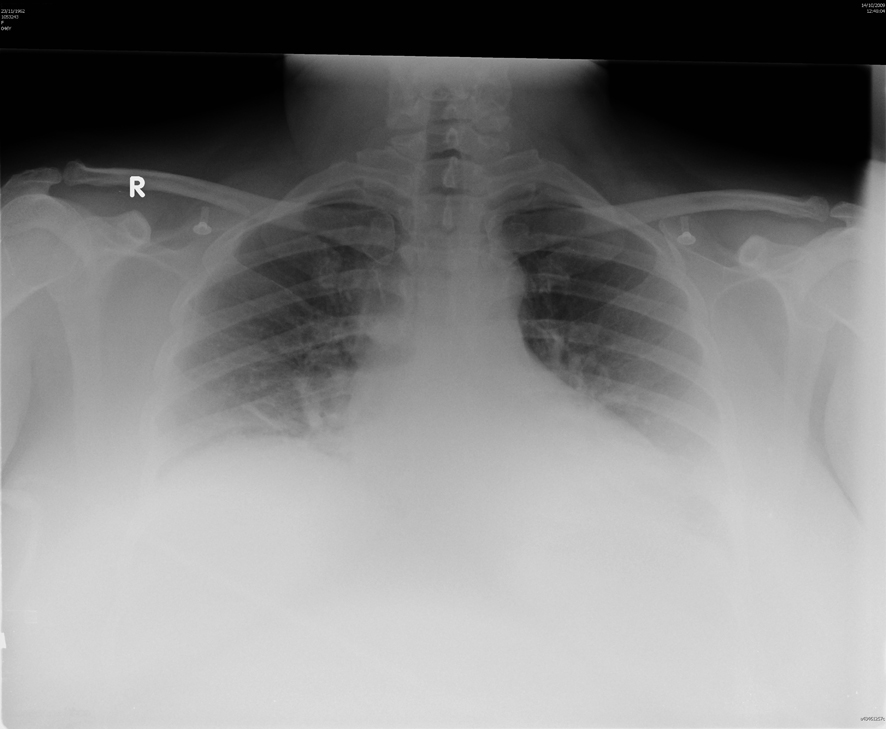 Click for large image | Figure 1. Chest X-ray on admission. |
Blood cultures were taken on admission, oseltamavir was discontinued and the patient was prescribed IV co-amoxiclav and oral clarithromycin. She was closely followed up by the critical care outreach team for 24 h due to her tachypnea and hypoxia but made a good clinical recovery and the co-amoxiclav was switched to oral after 72 h. Antibiotic treatment was given for 7 days and the patient went home well 5 days after admission.
The day after admission both anaerobic and aerobic blood culture bottles became positive and the gram stain indicated the organism was a gram negative coccobacillus.
The organism was indole and oxidase positive but failed to identify on the BD Phoenix™ Automated Microbiology System. An API® NH test was used as the organism was presumed to be a Hemophilus at this stage. The organism grew poorly on cystine lactose electrolyte deficient (CLED) agar, but grew well on the chocolate agar swarming the X and V factors. The API NH test identified the organism as Hemophilus sp (99.7%). Direct disk sensitivity testing indicated the organism was sensitive to ampicillin, trimethoprim, tetracycline, cefotaxime, co-amoxiclav, ciprofloxacin, imipenem and piperacillin/tazobactam.
An interim laboratory report was issued stating that the organism was a gram negative bacillus presumed Hemophilus and the organism was sent to the HPA reference laboratory in Colindale. The final report from the opportunistic pathogens section of the reference laboratory identified the organism as P.multocida, by 16S rDNA sequencing (not identified to sub-species level). The patient returned to Royal Gwent Hospital for follow-up 2 months after initial presentation having made a full recovery. When questioned, at that time, the patient reported looking after a sick cat with hematemesis prior to her illness. Unfortunately the cat had died so there was no opportunity to get a sample from the animal to confirm that the cat was the source of the infection.
Conclusions
Pneumonia caused by P.multocida in well middle-aged patients with no risk factors is extremely rare. This patient was unlucky to present with respiratory illness during an influenza pandemic following contact with H1N1 and therefore was initially misdiagnosed and treated inappropriately. It is understandable that the presumptive identification of Hemophilus was made given that: 1) this would be a more common respiratory pathogen and 2) laboratory identification of Pasteurella species can be confused with Hemophilus. Arguably when the organism was found to be easily cultured on chocolate agar the presumptive identification of Hemophilus species should have been questioned, but at that time the history of contact with a sick cat was not known. There is a distinct possibility that the organism was transmitted to the patient by aspiration whilst nursing the sick cat; however, only circumstantial evidence was available for this hypothesis. Fortunately for the patient the antibiotic treatment chosen was entirely appropriate and she made a full recovery.
| References | ▴Top |
- Weber DJ, Hansen AR. Infections resulting from animal bites. Infect Dis Clin North Am. 1991;5(3):663-680.
pubmed - Weber DJ, Wolfson JS, Swartz MN, Hooper DC. Pasteurella multocida infections. Report of 34 cases and review of the literature. Medicine (Baltimore). 1984;63(3):133-154.
- Chen HI, Hulten K, Clarridge JE
3rd . Taxonomic subgroups of Pasteurella multocida correlate with clinical presentation. J Clin Microbiol. 2002;40(9):3438-3441.
doi pubmed - Nelson SC, Hammer GS. Pasteurella multocida empyema: case report and review of the literature. Am J Med Sci. 1981;281(1):43-49.
doi - Mathai MG, Ebeo CT, Byrd RP
Jr , Fields CL, Roy TM. Cat cuddler's cough. Tenn Med. 2001;94(3):98-99.
pubmed - Hamilton-Miller JM. A possible pitfall in the identification of Pasteurella spp. with the API system. J Med Microbiol. 1993;39(1):78-79.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


