| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 2, February 2023, pages 76-79
Left Main Coronary Artery Aneurysm With Rare Quadfurcation Anatomy
Yevgeniy A. Latysheva, b, e, John P. Avendanoc, Sohil Patankard
aDivision of Cardiology, Jersey Shore University Medical Center, Neptune City, NJ 07753, USA
bHMH Interventional Cardiology, East Brunswick, NJ 08816, USA
cRobert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ, USA
dRutgers University, New Brunswick, NJ, USA
eCorresponding Author: Yevgeniy A. Latyshev, HMH Interventional Cardiology, East Brunswick, NJ 08816, USA
Manuscript submitted January 13, 2023, accepted February 16, 2023, published online February 25, 2023
Short title: LMCA Aneurysm With Quadfurcation
doi: https://doi.org/10.14740/jmc4037
| Abstract | ▴Top |
Coronary artery aneurysms (CAAs) are found in a small percentage of coronary angiograms, with left main coronary artery (LMCA) aneurysms being the least common. We present a 63-year-old male patient with a history of chest pain and an abnormal nuclear stress test. Cardiac catheterization showed a large LMCA aneurysm with unusual quadfurcation left main (LM) anatomy, but otherwise showed no evidence of obstructive coronary artery disease. The patient remained clinically stable, and a repeat cardiac catheterization 2 years later showed unchanged coronary anatomy. Further medical management with close observation was elected. This case illustrates that in select cases, large LMCA aneurysms can be successfully managed medically without surgical or percutaneous interventions. To our knowledge, this is the first report of LMCA aneurysm with quadfurcation anatomy. In addition to the case description, a review of the literature is provided.
Keywords: Coronary artery aneurysm; Left main coronary artery; Quadfurcation; Coronary anatomy; Management
| Introduction | ▴Top |
A coronary artery aneurysm (CAA) is defined as a dilatation of the coronary artery segment 1.5 times greater than that of an adjacent healthy segment [1]. CAAs are quite rare, yet their incidence may grow in the coming years due to the widespread use of invasive and noninvasive coronary imaging [2]. Among all CAAs, isolated left main coronary artery (LMCA) aneurysms are especially rare, with literature detailing an incidence of about 5.4% amongst 1,565 analyzed patients [3]. Left main (LM) varies in size, length, and branching across various body sizes, weights, and ethnic groups [4, 5].
The LMCA usually gives rise to two to three branches: the left anterior descending, left circumflex, and ramus intermedius arteries. In less frequent cases [4], the LMCA gives rise to two or three ramus intermedia. Complex branching patterns present a challenge to surgical and percutaneous interventions.
We present a unique case of an LMCA aneurysm with four branches, and further review the definition of CAAs, their overall incidence, how to diagnose them, and current treatment strategies. The findings of a recent systematic review found that ultimately, in the absence of controlled studies, a careful evaluation of each case is warranted to optimize therapeutic strategies for patients [2].
| Case Report | ▴Top |
Investigations
A 63-year-old male with a history of hypertension, hyperlipidemia, and obesity was initially evaluated for increased exertional dyspnea, intermittent chest pain at rest and with exertion, and fatigue. Symptoms started 2 - 3 weeks prior to presentation. The patient described the chest pain as intermittent, non-radiating pain lasting for seconds to minutes a few times per week. The patient does not have any significant family history of premature heart disease.
Diagnosis
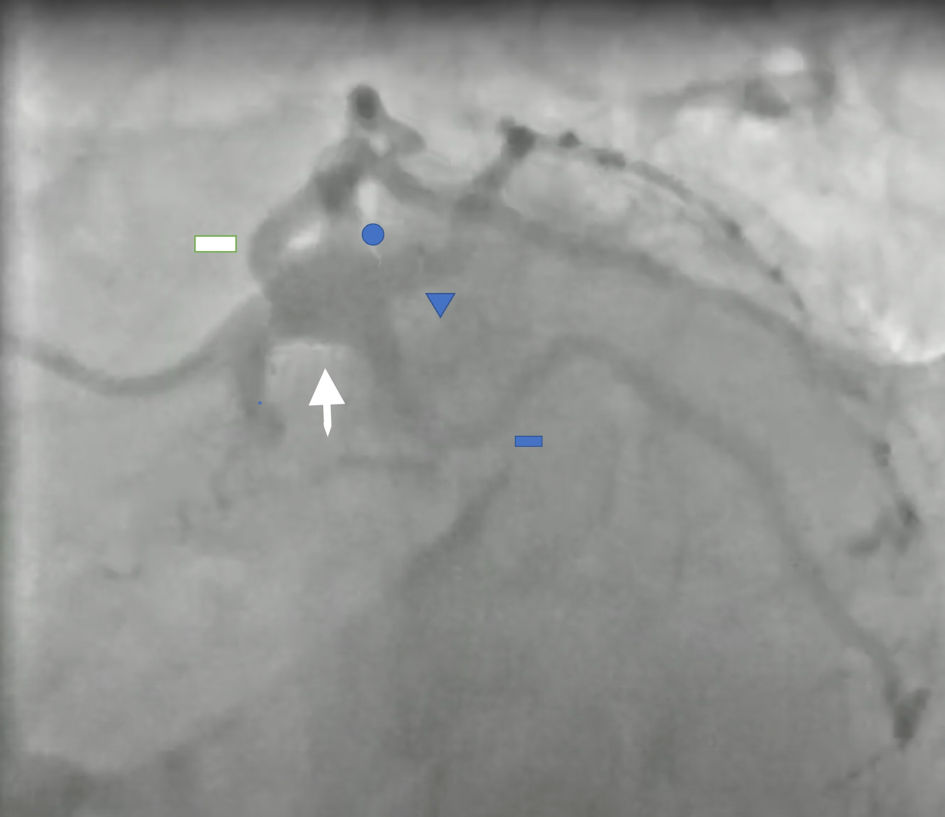
Initial investigations showed a slightly elevated blood pressure (136/80 mm Hg). On physical examination, the patient was obese with a body mass index (BMI) of 34 kg/m2. Otherwise, the physical examination was unremarkable. Electrocardiogram (ECG) revealed a normal sinus rhythm with no ischemic changes. The patient’s laboratory workup showed elevated low-density lipoprotein (LDL) levels at 126 mg/dL. Due to his symptoms and risk factors, an exercise nuclear stress test and echocardiogram were ordered. The nuclear stress test showed fair exercise tolerance without ischemic ECG changes, while perfusion images revealed inferior ischemia. Echocardiogram showed preserved left ventricular ejection fraction of 60-65% and no significant valvular abnormalities. Cardiac catheterization was subsequently recommended and showed an aneurysmal dilation of the trunk of the LMCA with an 11 mm transverse diameter. The left anterior descending, left circumflex, and first and second ramus intermedii revealed mild luminal irregularities (Fig. 1). Inferior ischemia observed on the stress test may have been due to the diaphragmatic attenuation artifact or microvascular disease.
 Click for large image | Figure 1. Left anterior oblique caudal (LAO caudal) view showed aneurysmal left main (LM) coronary artery (white arrow) with four branches (quadfurcation). Blue circle: first ramus intermedius artery, blue triangle: second ramus intermedius artery, angiographically mild luminal irregularities of the left anterior descending, first and second ramus intermedius, and left circumflex coronary arteries. White rectangle: left anterior descending artery; blue rectangle: left circumflex artery. |
Treatment
After consulting cardiothoracic surgery, the patient was started on 81 mg of aspirin daily while their daily evening dose of atorvastatin was increased from 40 to 80 mg. Blood pressure was managed with metoprolol 25 mg daily as well as losartan 25 mg daily. The patient’s blood pressure and cholesterol were much better controlled with a repeat LDL after 3 months on a high intensity statin of 88 mg/dL, and his chest pain resolved. Two years later, the patient had a repeat cardiac catheterization that showed a stable, unchanged aneurysmal LMCA (Fig. 2). After a discussion regarding potential further treatment with either a coronary artery bypass graft (CABG) or medical therapy, a decision was ultimately made to opt for medical therapy.
 Click for large image | Figure 2. Angiogram taken 2 years later showed no change from prior angiogram. White arrow: aneurysmal left main coronary artery; blue circle: first ramus intermedius artery; blue triangle: second ramus intermedius artery; white rectangle: left anterior descending artery; blue rectangle: left circumflex artery. |
Follow-up and outcomes
The patient visits our office every 4 - 6 months and is being closely observed for recurrence of chest pain or worsening of his shortness of breath. The patient periodically repeats coronary angiography via cardiac catheterization or computed tomography angiography (CTA) to monitor for progression of the disease.
| Discussion | ▴Top |
LMs vary in size, length, and branching across various body sizes, weights, and ethnic groups. Although trifurcation is a common anatomical variant, quadfurcation and pentafurcation are also possible, yet less common [4]. An anatomical study of an Indian population observed quadfurcation in 8% of cadavers [5]. Another anatomical study from an indigenous Kenyan population revealed 9.6% of cadaveric hearts with quadfurcation anatomy [4]. Quadfurcation is less frequent in patients of European decent, although the true incidence is not known [4].
CAAs are classified as either true aneurysms or pseudoaneurysms. True aneurysms include all three layers of the vessel. Pseudoaneurysms, or false aneurysm, are abnormal dilatations of an artery that is contained only by the outermost vessel layer, otherwise known as the tunica adventitia [1]. The first pathological case of a CAA aneurysm was reported by Margagni in 1761 [6], and almost 200 years later, in 1958, Munkner et al reported the first case of a CAA diagnosed by cardiac catheterization [7].
The right coronary artery is the most common location of CAAs (40%), followed by the left anterior descending coronary artery (32%), and LMCA (0.1-3.5%) [8, 9]. Angiographic diagnosis of CAA is operator dependent, with variability in diagnoses. While the true incidence of CAA is likely underestimated, more widespread use of coronary CTA will lead to further understanding of true incidence of the disease [9].
The etiology of CAA varies geographically. In Europe and North America, about 50% of cases are due to atherosclerosis, followed by congenital cases constituting 17%, and Kawasaki disease accounting for the last 10% [10]. In Japan and China, most cases are due to Kawasaki disease. Giant coronary aneurysms are thought to be due to congenital heart disease [10]. CAA can be iatrogenic due to coronary artery stenting via direct intimal injury, delay in healing due to antiproliferative coating, and/or stent malapposition. One of the procedural risk factors for iatrogenic CAA include chronic total occlusion (CTO) and long lesions [11].
CABG surgery remains a frequently used treatment for multivessel disease. Although arterial grafts are preferred, venous conduits remain widely used. Although rare, saphenous vein graft (SVG) aneurysms have been reported as large as 10 cm, and they often present more than 10 years after CABG. SVG aneurysms present with mechanical complications: compression of adjacent structures, fistulas to adjacent structures, and/or rupture [12].
CAAs are most often incidentally found on coronary CTA or during catheterization, as most patients are asymptomatic [13]. Patients with concomitant coronary artery disease can present with stable angina and/or acute coronary syndrome [13]. CAA predisposes patients to thrombus formation and distal embolization, often resulting in acute coronary syndrome [13]. Management and intervention of suspected aneurysms is of the utmost importance, as aneurysm rupture can lead to tamponade, and aneurysm expansion can lead to compression of adjacent structures [13]. Additionally, patients with large aneurysms can present with superior vena cava syndrome or with a mediastinal mass [9].
The two most common modalities for coronary ectasia and aneurysm diagnosis are coronary angiography and coronary CTA [14]. Coronary angiography paired with intravascular ultrasound (IVUS) provides a better understanding of vessel wall structure. Through angiography, true aneurysms can be better differentiated from pseudoaneurysms [13]. Although optical coherence tomography (OCT) offers greater axial resolution compared to IVUS, penetrating depth is lower. OCT is of limited benefit in assessment of large CAA [15]. Coronary CTA offers advantages due to more accurate assessment of the aneurysm size and degree of thrombus verses invasive angiography. CTA is especially useful for patients with giant aneurysms and vein graft aneurysms [13].
Given that LMCA aneurysms are incredibly infrequent, with a study reporting a frequency of about 0.1% amongst 20,332 adult patients, optimal treatment is not standardized and currently relies on expert opinion [8]. Treatment options include conservative medical management, stenting, and/or surgery.
Although no consensus exists regarding the best surgical approach to treatment of LMCA aneurysms, several surgical options have been described. LM branch ligation, LM aneurysm repair, or reconstruction have all been listed as potential treatment routes. A significant limitation of LM ligation is subsequent future loss of percutaneous coronary access to treat coronary artery disease. Patch repair of the LM aneurysm enables future access of the coronary tree. Pericardial patch, internal thoracic artery and saphenous veins can be used for repair of the aneurysm [14]. A hybrid technique using percutaneous coronary intervention (PCI) and a surgical treatment has also been described [16].
In a recent systematic review of 209 cases of LMCA aneurysms, more than half of cases were treated surgically [2]. Surgical management of LMCA aneurysms is often appropriate in symptomatic patients who have obstructive coronary artery disease, patients with evidence of embolization leading to myocardial ischemia, or in patients with CAAs at risk of rupture [2, 17].
A carefully selected subset of aneurysms can be treated with stents. Covered stents mainly are appropriate for saccular aneurysms, pseudoaneurysms, and aneurysms < 10 mm in diameter [18]. Conventional stents and coil embolization are also available. Coiling or stent assisted coiling can be used to treat aneurysms involving significant side branches [13]. Three or more LM branches also present additional challenges for LM stenting. Ultimately, treatment choice should be based on patient factors and operator preference.
Risk factor modifications are a cornerstone of the treatment of coronary aneurysms, especially when atherosclerotic disease is the predominant cause of aneurysmal disease in the European and American adult populations. However, the role of dual antiplatelet therapy or therapeutic anticoagulation is not well understood. There may be a role in therapeutic anticoagulation in patients with CAAs and myocardial infarction as well as patients with Kawasaki disease and rapidly expanding aneurysms [13].
While surgical management is often heralded as the mainstay of treatment in LMCA aneurysms, conservative medical treatment has also been reported in the literature as a viable alternative. The severity of coexistent coronary artery stenoses dictates whether surgical treatment is necessary for CAA patients, and surgical management is appropriate in symptomatic patients with evidence of emboli from the aneurysm to the distal coronary bed that could lead to myocardial ischemia [19]. In cases of documented CAA enlargement over a period of time, surgery is also an option [20].
LMCA aneurysms with complex branching present a diagnostic and treatment dilemma for a clinician. LM aneurysms and rare branching patterns should be recognized due to additional surgical or percutaneous treatment complexity. After a discussion with a heart team that included an interventional cardiologist and a cardiothoracic surgeon, we felt that medical treatment was appropriate given his asymptomatic state over a 2-year period without angiographic progression of disease. We will continue to monitor our patient for aneurysmal growth with periodic cardiac catheterizations.
Our report presents an unusual case of LMCA aneurysm with quadfurcation anatomy. Due to the increasing use of noninvasive coronary imaging, we can detect CAA much more frequently. In many cases of clinically stable patients with minimal or no symptoms, LMCA presents a treatment challenge. Due to lack of randomized trials and validated treatment algorithms, clinicians must evaluate each case individually. With an expected increase in LMCA aneurysm incidence, we hope that additional data will provide further insight into optimal treatment strategies.
Learning points
Medical management of LMCA aneurysms continue to prove to be effective treatments in asymptomatic patients without evidence of emboli from the aneurysm to the distal coronary bed and no risk of myocardial ischemia and/or predisposing risk factors of rupture.
Acknowledgments
We thank the staff of the Division of Cardiology at Jersey Shore University Medical Center.
Financial Disclosure
Authors have no financial disclosures to report.
Conflict of Interest
The authors declare that they have no conflict of interests concerning this article.
Informed Consent
Patient consent for publication was obtained.
Author Contributions
Yevgeniy A. Latyshev: idea, manuscript writing. John P. Avendano: manuscript writing. Sohil Patankar: manuscript writing.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- D'Souza D, Bickle I, Bickle I, et al. False aneurysm. Reference article, Radiopaedia.org. Accessed on Dec 11, 2022.
doi - Negro F, Gentile F, Rizza A, Giannoni A, Bianchi G, Clemente A, Emdin M, et al. Etiology, clinical presentation, and management of left main coronary artery aneurysms. J Card Surg. 2022;37(11):3675-3686.
doi pubmed - Nunez-Gil IJ, Cerrato E, Bollati M, Nombela-Franco L, Terol B, Alfonso-Rodriguez E, Camacho Freire SJ, et al. Coronary artery aneurysms, insights from the international coronary artery aneurysm registry (CAAR). Int J Cardiol. 2020;299:49-55.
doi pubmed - Ogeng'o JA, Misiani MK, Olabu BO, Waisiko BM, Murunga A. Variant termination of the left coronary artery: pentafurcation is not uncommon. Eur J Anat. 2014;18:98-101.
- Agrawal R. Anatomical study of branching pattern of main trunk of left coronary artery and its importance. Indian J App Research. 2016;6:626-628.
- Morgagni GB. de Sedibus et Causis morborum. Venectus I. 1761:28.
- Munkner T, Petersen O, Vesterdal J. Congenital aneurysm of the coronary artery with an arteriovenous fistula. Acta radiol. 1958;50(4):333-340.
doi pubmed - Syed M, Lesch M. Coronary artery aneurysm: a review. Prog Cardiovasc Dis. 1997;40(1):77-84.
doi pubmed - Abou Sherif S, Ozden Tok O, Taskoylu O, Goktekin O, Kilic ID. Coronary artery aneurysms: a review of the epidemiology, pathophysiology, diagnosis, and treatment. Front Cardiovasc Med. 2017;4:24.
doi pubmed - Li D, Wu Q, Sun L, Song Y, Wang W, Pan S, Luo G, et al. Surgical treatment of giant coronary artery aneurysm. J Thorac Cardiovasc Surg. 2005;130(3):817-821.
doi pubmed - Ipek G, Gungor B, Karatas MB, Onuk T, Keskin M, Tanik O, Hayiroglu MI, et al. Risk factors and outcomes in patients with ectatic infarct-related artery who underwent primary percutaneous coronary intervention after ST elevated myocardial infarction. Catheter Cardiovasc Interv. 2016;88(5):748-753.
doi pubmed - Ramirez FD, Hibbert B, Simard T, Pourdjabbar A, Wilson KR, Hibbert R, Kazmi M, et al. Natural history and management of aortocoronary saphenous vein graft aneurysms: a systematic review of published cases. Circulation. 2012;126(18):2248-2256.
doi pubmed - Kawsara A, Nunez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of coronary artery aneurysms. JACC Cardiovasc Interv. 2018;11(13):1211-1223.
doi pubmed - Iwakura T, Toguchi K, Kato I, Asakawa N. Internal thoracic artery patch repair of a saccular left main coronary artery aneurysm. J Cardiothorac Surg. 2019;14(1):38.
doi pubmed - Gupta A, Shrivastava A, Vijayvergiya R, Chhikara S, Datta R, Aziz A, Singh Meena D, et al. Optical coherence tomography: an eye into the coronary artery. Front Cardiovasc Med. 2022;9:854554.
doi pubmed - Bhamidipati CM, McCabe JM, Jones TK, Lombardi WL, Reisman M, Pal JD. Hybrid management of a giant left main coronary artery aneurysm. Ann Thorac Surg. 2017;103(1):e89.
doi pubmed - Doustkami H, Maleki N, Tavosi Z. Left main coronary artery aneurysm. J Tehran Heart Cent. 2016;11(1):41-45.
- Cohen P, O'Gara PT. Coronary artery aneurysms: a review of the natural history, pathophysiology, and management. Cardiol Rev. 2008;16(6):301-304.
doi pubmed - Lima B, Varma SK, Lowe JE. Nonsurgical management of left main coronary artery aneurysms: report of 2 cases and review of the literature. Tex Heart Inst J. 2006;33(3):376-379.
- Khalid N, Chhabra L, Ahmad SA, Sareen P. A large-sized left main coronary artery with quadfurcation: a rare anatomy. Conn Med. 2015;79(4):211-212.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


