| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 9, September 2013, pages 594-597
Bronchocele: Two Cases
Gulfidan Cakmaka, d, Nurdan Gockunb, Emre Evrenb, Zuhal Aydan Saglamc
aHaseki Training and Research Hospital, Chest Disease, Istanbul, Turkey
bHaseki Training and Research Hospital, Radiology, Istanbul, Turkey
cDepartment of Family Medicine, Goztepe Training and Research Hospital, Istanbul Medeniyet University, Turkey
dCorresponding author: Gulfidan Cakmak, Merkezefendi mh Topkapi merkezevleri A 4 blok D 10 Zeytinburnu, Istanbul, Turkey
Manuscript accepted for publication July 5, 2013
Short title: Bronchocele Case Report
doi: https://doi.org/10.4021/jmc1364w
| Abstract | ▴Top |
A bronchocele (bronchial mucocele) results from the mucoid impaction and dilatation of the proximal bronchus caused by congenital bronchial atresia (CBA) or bronchial obstruction. Bronchocele must be considered in the differential diagnosis of radiologic pathologies.
Keywords: Congenital bronchial atresia; Bronchocele; Congenital pulmonary disease
| Introduction | ▴Top |
Bronchial atresia is a rare variety. In this article we aimed to remind bronchocele clinically and radiologically in differential diagnosis by reporting two patients with bronchocele of which one presented with infection and the other was incidentally found.
| Case Report | ▴Top |
Case 1
An asymptomatic 34-year old woman applied for a health certificate which was required for job application. Her physical examination revealed no pathology. She wasn’t smoking and not taking any medicine for any disease either. Her chest radiography had been taken several times so far, yet she was informed that each of them was normal (Fig. 1). Computed thorax tomography was performed according to the findings at chest x-ray(Fig. 2, 3).
 Click for large image | Figure 1. Scanogram of case 1. |
 Click for large image | Figure 2. Scanogram of case 2. |
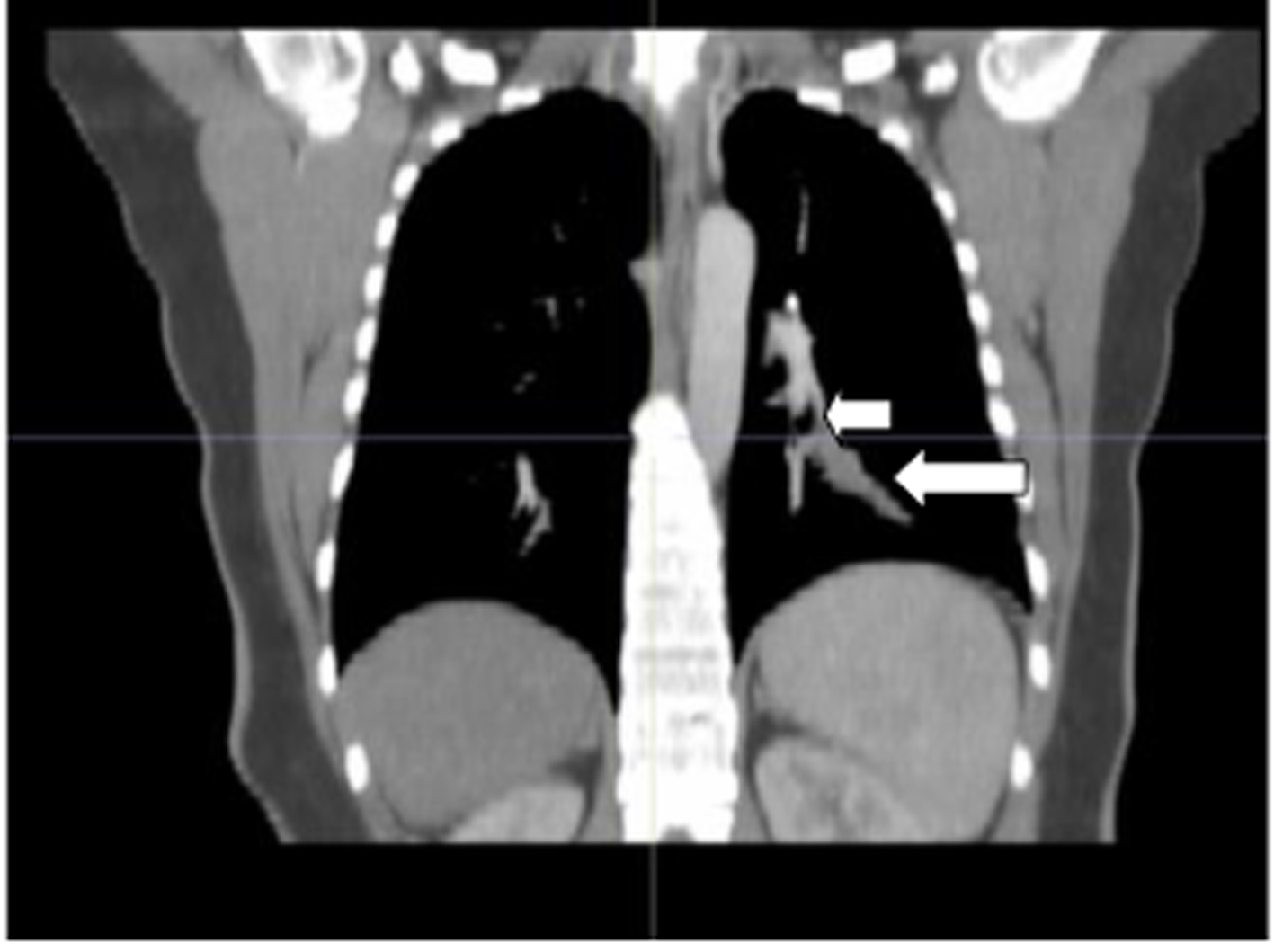 Click for large image | Figure 3. The image with Minimum Intensity Projection technique at coronal mediastinal window of case 1. Short arrow at left: lower bronchial lobe; long arrow: atresic bronchus filled with mucus. |
Case 2
A 30-year old woman had a three-week history of cough, fever and chest pain. The clinical findings lead to a pulmonary infection so antibiotherapy was started. The electrocardiogram was normal. The symptoms slowed down but did not cease so the patient was referred to a chest disease specialist. Her physical examination was unremarkable except a few rales at the left hemithorax. Her white blood count was 8,800/mm3, erythrocyte sedimentation rate: 15 mm/hour and C-reactive protein was: 0.9 mg/dL. Computed tomography was performed on the basis of the opacity seen on posterio-anterior chest graphy (Fig. 4).
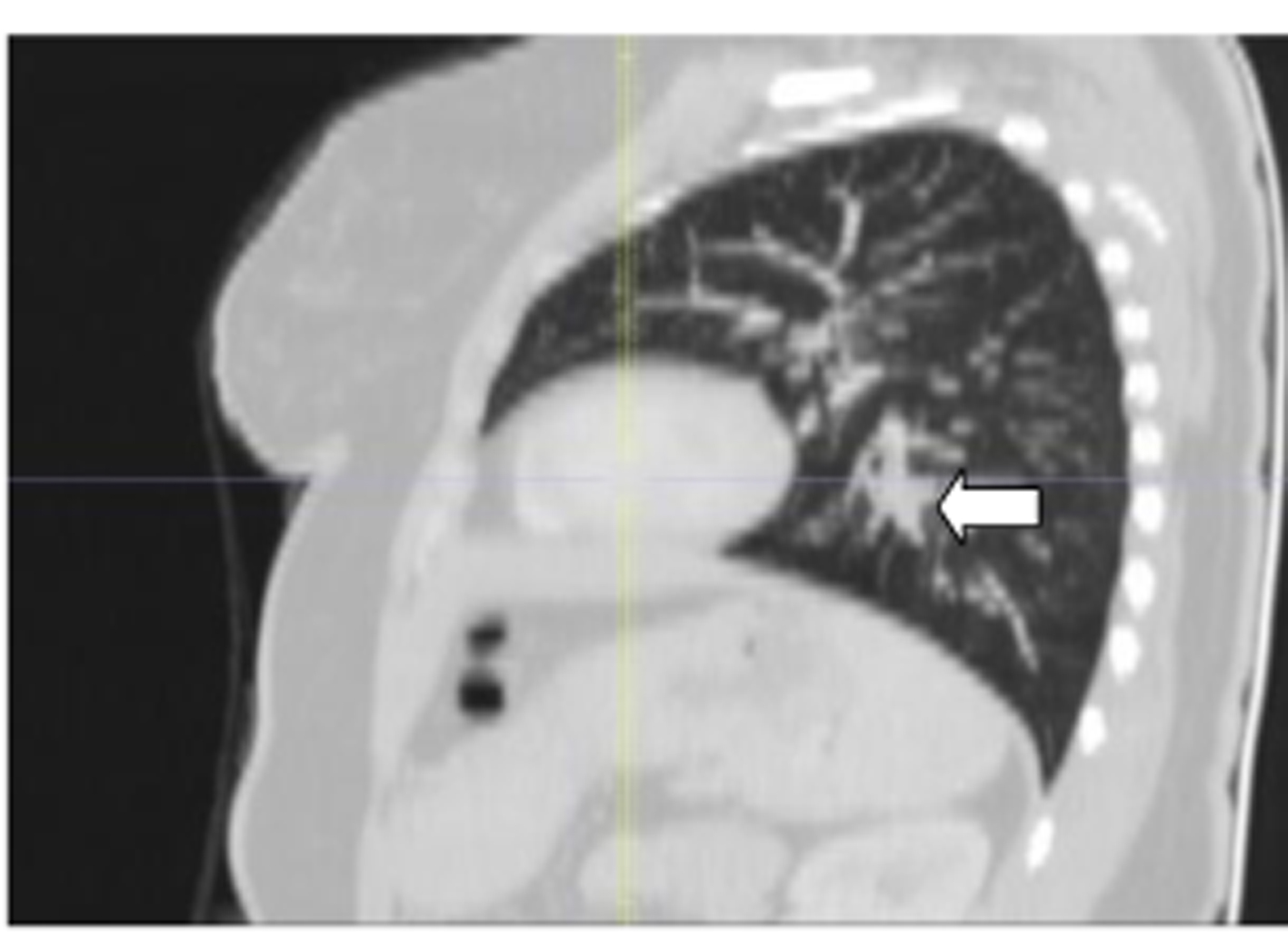 Click for large image | Figure 4. The image with Minimum Intensity Projection technique at sagittal parenchimal window of case 1. The arrow shows the atresic bronchus filled with mucus. |
Chest computed tomography was performed from apical to basale with a 64-detector row CT scanner (Brilliance, Philips Healthcare) at supine position and inspirium. Parameters for helical scanning were: tube voltage, 120 kV; tube current threshold, 300 mAs; rotation time, 0.5 sec/rot; collimation, 64 × 0.625 mm; beam pitch, 0.64 - 1.06; reconstructed section thickness, 1.0 mm. CT angiography was done using a non-ionic iodinated contrast media of 35 mL injected through the antecubital vein at 5 mL/second rate (Fig. 5, 6).
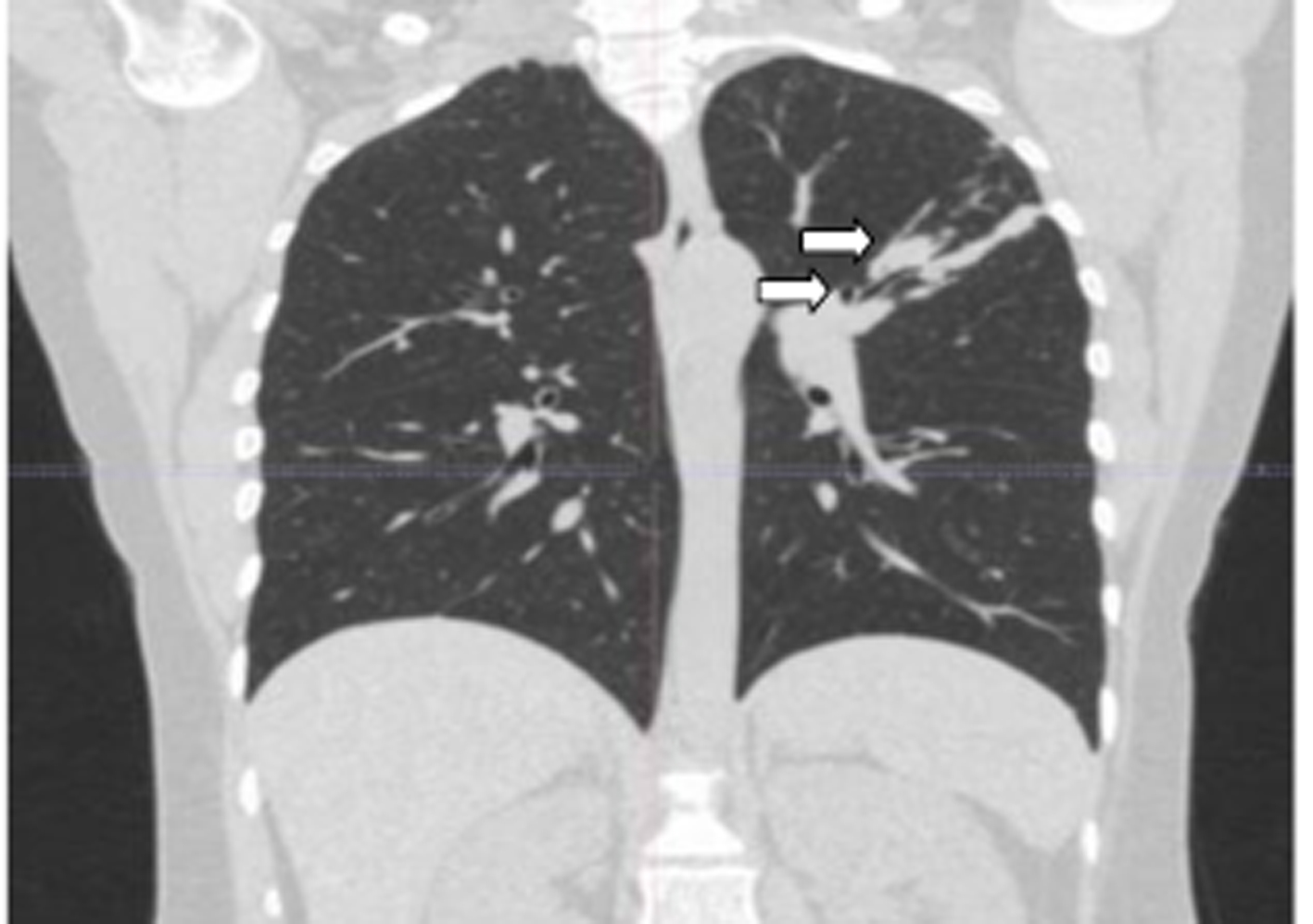 Click for large image | Figure 5. The image with Minimum Intensity Projection technique at coronal parenchimal window of case 2. Left upper arrow: atresic bronchus filled with mucus; left lower arrow: upper apicoposterior segmental bronchus. |
 Click for large image | Figure 6. The image with Minimum Intensity Projection technique at sagittal parenchimal window of case 2. Right arrow: the upper bronchus; left arrow: atresic bronchus filled with mucus. |
High-resolution three-dimensional volume rendering-magnetic resonance technique (3-D VR) was conducted when the images were suggestive of bronchocele. The assessments were made with axial reconstruction of 1 mm and 5 mm at reformats obtained at coronal and sagittal planes using volume rendered 3-D imaging and 5 mm Minimum Intensite Projeksiyon (MIP) imaging techniques [1, 2].
MIP is a data visualization method that enables detection of highly intense structures and doesn’t give information about the depth of the image. At minimum intensity projection (Min IP) volume rendering technique, the images get information from each voxel. Min IP, as a computed tomography (CT) volumetric rendering technique provides added diagnostic capabilities as well as help better understanding three dimensional relationships of anatomic structures and determining the appropriate surgical approach in case [2].
It is important to assess the case with axially reconstructed images. Volume rendering may be internally or externally performed and it gives important information about the trachea-bronchial tree as detailed as bronchoscopy [1, 3].
So it is granted as a non invasive method in patients who can not tolerate bronchoscopy or refuse to have it done [3, 4]. According to all of these evaluations bronchocele related to bronchial atresia was diagnosed radiologically. VR imaging of cases 1 and 2 are shown at Figures 7 and 8.
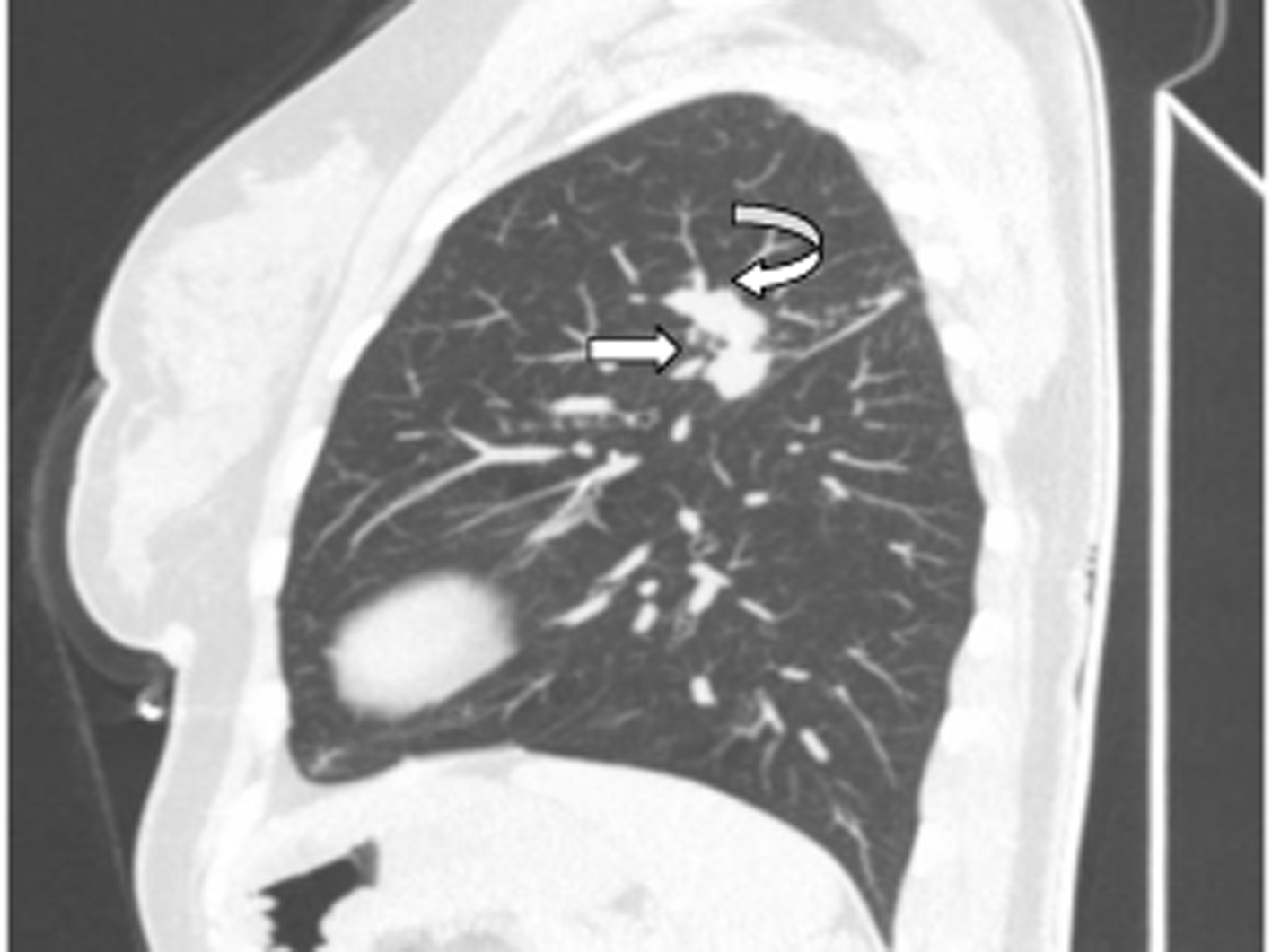
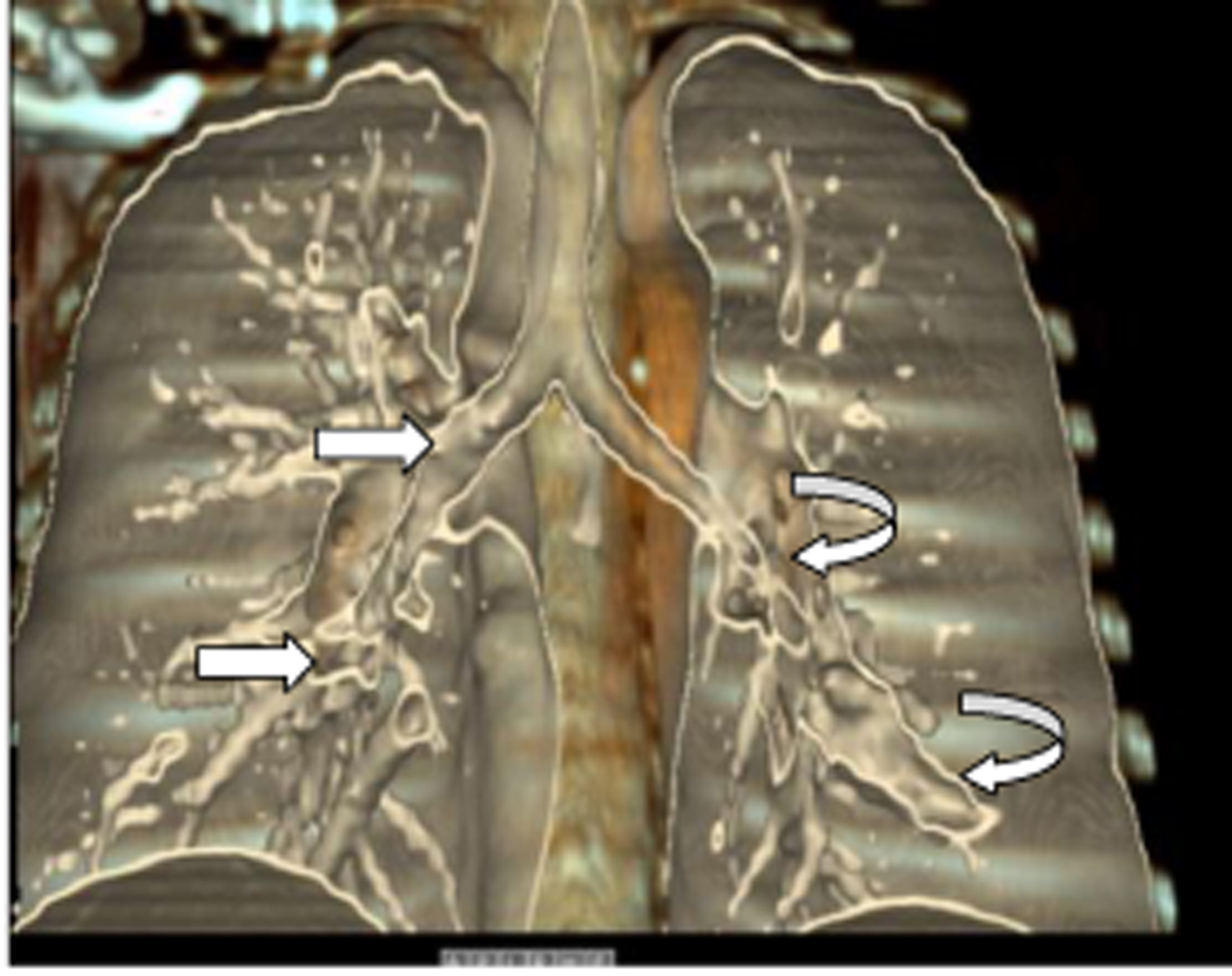 Click for large image | Figure 7. Coronal VR imaging of case 1. Right upper arrow: right main bronchus; right lower arrow: bronchus of lower lobe. Curved left arrows, upper: bronchus of lower lobe; lower: atresic bronchus filled with mucus. |
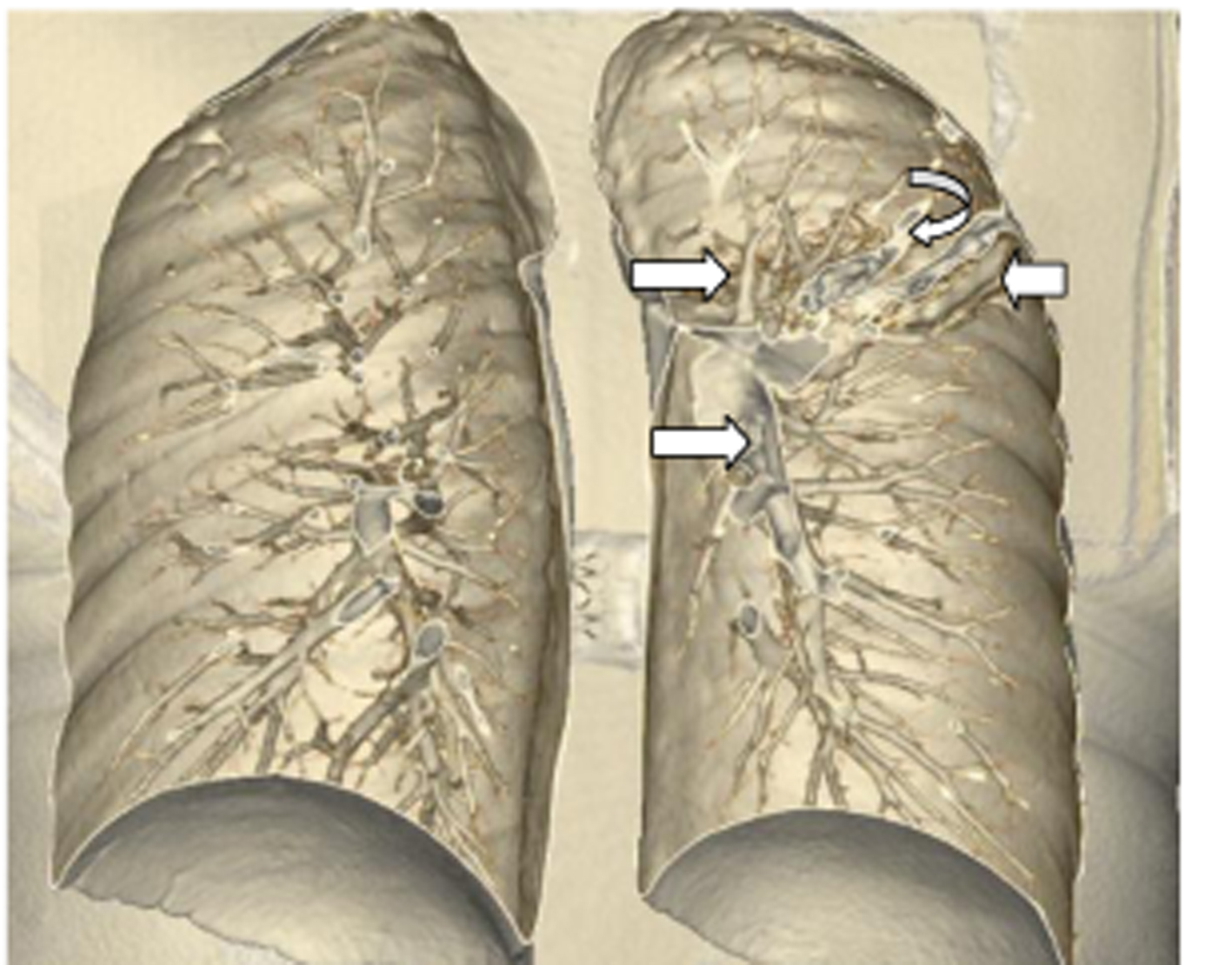 Click for large image | Figure 8. VR image of case 2. Right upper arrow: upper lobe bronchus; right lower arrow: lower lobe bronchus. Left upper arrow: atresic bronchus filled with mucus; left lower arrow: infiltration limited with major fissura. |
| Discussion | ▴Top |
Bronchocele is first defined at 1800’s. CBA is the most common reason of bronchocele and. It is a cystic formation caused by mucus impaction and dilatation at the proximal of obstructed or atresic bronchiol [2-4]. Congenital atresia, scatricial shrinkage of bronchial lumen, a foreign object or neoplasms may cause the obstruction. Nevertheless bronchial atresia is the most common reason and first defined at 1949 [1]. Although the obstruction or atresia may cause atelectasis at the lober bronchus, it may not result with volume depletion at segmental or subsegmental bronchioles [1, 5]. Since we could not demonstrate any massive lesion, a foreign object or fibrotic sequel band which may cause the obstruction in none of our cases, bronchial atresia was considered to be the main reason of the obstruction. Bronchocele cases in literature are generally in association with an obstruction caused by a neoplasm [6, 7].
Bronchial atresia is a rare variety of chest anomaly. It generally results from a localized defect in normal bronchopulmonary embryogenesis [5, 8]. The development of lungparenchyme is generally normal [9]. It has a male predominance. The estimated prevalence is 1.2 cases per 100,000 males [10]. The patients are generally asymptomatic and the disease is diagnosed coincidentally at the second or third decades.
The left upper lobe involvement is 64% while left lower lobe is 14% involved [9]. It is commonly demonstrated at a single segmential bronchiol, yet multiple segmential atresias are also reported [1, 6]. Our cases were diagnosed at their thirties.Raza and Aronberg’s cases were at their sixties. Bronchial atresia was at the left lower lobe in our first case while it was at the left upper lobe in the second one. In Raza, Yoon, and Aronberg’s cases bronchoceles were at the right upper lobe and lingula, in Gibson’s case it was at the left upper lobe similar to our case.
Bronchocele is diagnosed radiologically or/and by bronchoscopy. Radiologically hyperinflation is reported commonly in the affected side as well as collapse at the affected lobe and mass image of the mucocele. Calcification may also be reported [5, 11]. In our first case, there was only oscultative findings. In the second one radiologic infiltration was recorded. In differential diagnosis of cystic lesions of lungs; congenital abnormalities (pulmonary sequestration, bronchogenic cyst and bronchocele), tumoral masses (primary pulmonary mucinous adenocarcinosis or pulmonary metastasis of it) should be necessarily kept in mind. Bronchoscopically, blind ending may be demonstrated at the atresic bronchus yet it may be normal as well [10]. Bronchoscopy is also recommended for patients with bronchial atresia in literature in order to exclude other possible pathologies [4, 12, 13]. We performed bronchoscopy to the case who had findings of infection. The result was normal. The other patient refused to have bronchoscopy. On the basis of these information we diagnosed our patients with thorax CT.
Although it may be asymptomatic, dyspnea, recurrent infections and cough, fever and hemoptysis may be recorded. It may rarely cause pneumothorax [8]. Hyperinflation of the obstructed lung segment and check valve mechanism is held responsible [6, 11]. It may be associated with congenital cystic adenomatoid malformation and pectus excavatum [9, 14, 15].
In conclusion, bronchocele is benign and asymptomatic and may be diagnosed radiologically. Bronchoscopy may be done to exclude associating pathologies. Nevertheless an obstructing tumoral mass should be kept in mind in case an obstruction is determined.
| References | ▴Top |
- Achenbach S, Giesler T, Ropers D, Ulzheimer S, Derlien H, Schulte C, Wenkel E, et al. Detection of coronary artery stenoses by contrast-enhanced, retrospectively electrocardiographically-gated, multislice spiral computed tomography. Circulation. 2001;103(21):2535-2538.
doi pubmed - Gerber BL, Coche E, Pasquet A, Ketelslegers E, Vancraeynest D, Grandin C, Van Beers BE, et al. Coronary artery stenosis: direct comparison of four-section multi-detector row CT and 3D navigator MR imaging for detection—initial results. Radiology. 2005;234(1):98-108.
doi pubmed - Sakarya ME, Ceran S, Koç O, Ozbek O,KarabekmezLG, Odev K. Bronchocele: DemonstrationBy 3D Volume Rendering Imaging with Multidetector Computed Tomography: Case Report. Turkiye Klinikleri J Med Sci. 2011;31(1):251-255. (in Turkish).
doi - Laroia AT, Thompson BH, Laroia ST, van Beek E, Jr. Modern imaging of the tracheo-bronchial tree. World J Radiol. 2010;2(7):237-248.
doi pubmed - Gipson MG, Cummings KW, Hurth KM. Bronchial atresia. Radiographics. 2009;29(5):1531-1535.
doi pubmed - Aronberg DJ, Sagel SS, Jost RG, Levitt RG. Oat cell carcinoma manifesting as a bronchocele. AJR Am J Roentgenol. 1979;132(1):23-25.
doi pubmed - Raza SA, Alexakis C, Creagh M, Lawrence DR, Wood M. Primary pulmonary mucinous cystadenocarcinoma presenting as a complex bronchocele: a case report. J Med Case Rep. 2009;3:8581.
doi pubmed - Yoon YH, Son KH, Kim JT, Baek WK, Kim KH, Lee KH, Han HS. Bronchial atresia associated with spontaneous pneumothorax: report of a case. J Korean Med Sci. 2004;19(1):142-144.
doi pubmed - Cappeliez S, Lenoir S, Validire P, Gossot D. Totally endoscopic lobectomy and segmentectomy for congenital bronchial atresia. Eur J Cardiothorac Surg. 2009;36(1):222-224.
doi pubmed - Psathakis K, Eleftheriou D, Boulas P, Mermigkis C, Tsintiris K. Congenital bronchial atresia presenting as a cavitary lesion on chest radiography: a case report. Cases J. 2009;2(1):17.
doi pubmed - Wang Y, Dai W, Sun Y, Chu X, Yang B, Zhao M. Congenital bronchial atresia: diagnosis and treatment. Int J Med Sci. 2012;9(3):207-212.
doi pubmed - Ward S, Morcos SK. Congenital bronchial atresia—presentation of three cases and a pictorial review. Clin Radiol. 1999;54(3):144-148.
doi - Daoud B, Moncada R, Ali J. Lung mass in a smoker. Chest. 2001;119(3):947-949.
doi pubmed - Discioscio V, Feraco P, Bazzocchi A, Femia R, Romeo C, Fasano L, Pacilli AM, et al. Congenital cystic adenomatoid malformation of the lung associated with bronchial atresia involving a different lobe in an adult patient: a case report. J Med Case Rep. 2010;4:164.
doi pubmed - Shepherd FJ. III. Some Remarks on the Symptoms of Bronchocele and the Results of Operative Treatment. Ann Surg. 1899;30(5):564-570.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


