| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 9, September 2013, pages 644-647
Endobronchial Metastases of Renal Cell Carcinoma: A Complex Multidisciplinary Treatment
Franco Ravennaa, Valentina Contia, Elisabetta Salviatob, Elisabetta Marangonic, Marco Verric, Michele Paolazzic, Roberto Galeottib, Gaetano Caramoria, d
aDipartimento Emergenza, Unita Operativa di Pneumologia, University of Ferrara, Italy
bDipartimento Diagnostica per immagini e Medicina di Laboratorio, Unita Operativa di Radiologia Vascolare ed Interventistica, from Azienda Ospedaliera Universitaria di Ferrara Arcispedale S. Anna, Italy
cUnita Operativa di Anestesia e Rianimazione Universitaria, Italy
dCorresponding author: Gaetano Caramori, Centro per lo Studio delle Malattie Infiammatorie Croniche delle Vie Aeree e Patologie Fumo Correlate dell’Apparato Respiratorio (CEMICEF; formerly termed Centro di Ricerca su Asma e BPCO), Sezione di Malattie dell’Apparato Respiratorio, University di Ferrara, Via Savonarola 9, 44121 Ferrara, Italy
Manuscript accepted for publication July 5, 2013
Short title: Endobronchial Metastases of Renal Cell Carcinoma
doi: https://doi.org/10.4021/jmc1371w
| Abstract | ▴Top |
We report a case of endobronchial metastases of renal cell carcinoma, treated with rigid bronchoscopy and laser resection followed by bronchial artery embolization, in a 56-year-old Caucasian man, presenting with dyspnea, cough, and hemoptysis. Computed tomography of the chest and flexible bronchoscopy showed a large mass under the tracheal carina causing complete occlusion of the left main bronchus and subtotal (90%) occlusion of the right main bronchus, with saving of the homolateral lobar bronchi. The right main bronchus stenosis was removed during rigid bronchoscopy using neodymium-doped yttrium aluminum garnet laser and mechanical disruption. The procedure caused persistent bleeding, for this reason the right main bronchus was selectively intubated and bronchial arterial embolization was performed with arrest of the bleeding. After 3 days of Intensive Care Unit stay a bronchoscopy performed a day later documented the complete reopening of the right main bronchus. In conclusion, bronchial arterial embolization should be considered as another treatment option in endobronchial metastases of highly vascularized tumors such as renal cell carcinoma that often cause bleeding during their endoscopic resection.
Keywords: Bronchial artery embolization; Interventional bronchoscopy; Renal cell carcinoma; Bleeding; Rigid bronchoscope
| Introduction | ▴Top |
Interventional bronchoscopy, including laser resection and stent placement, is an established palliative treatment for malignant diseases obstructing trachea and/or the larger bronchi [1, 2]. Laser resection is usually used and considered safe in most instances. However, extreme caution should be taken, particularly in highly vascularized tumors, to avoid uncontrollable massive bleeding and some subsets of endobronchial tumors have the higher risk of bleeding [3]. Endobronchial metastases of extrapulmonary solid malignant tumors are rare with breast, colon and renal carcinomas as the most frequent causes [4, 5]. There is no universally accepted approach to the management of endobronchial metastases. We describe here the case of a patient with bilateral main bronchi obstruction secondary to metastases of renal cell carcinoma, which is a neoplastic tissue hypervascular and hemorrhagic, treated by interventional bronchoscopy followed by bronchial artery embolization to arrest the persistent bleeding at the end of the endoscopic procedure.
| Case Report | ▴Top |
A 56-year-old man, former smoker (37 pack-years), working as a blacksmith was admitted in the 2012 to our ward. His past medical history was characterized by glucose-6-phosphate dehydrogenase deficiency and right nephrectomy for a clear cell renal carcinoma (Grade II) in 1992. The post-operative follow up was regular until 2001 when a solitary chest mass (32 mm × 32 mm) was detected using chest computed tomography in the right upper lobe. A wedge resection of this mass performed in another hospital revealed the presence of a metastases of the clear cell renal carcinoma. The referral oncologist did not start at the time any treatment of the pulmonary lesion.
Subsequently in 2006, a vegetating lesion appeared on the left main bronchus associated to mediastinal subcarinal lymphoadenomegaly. The endobronchial lesion was resected in another hospital using rigid bronchoscopy and its histopathological examination confirmed the presence of clear cell renal carcinoma. At this time the patient initiated six cycles of chemotherapy with sunitinib (50 mg/die of sunitinib for four consecutive weeks followed by two weeks without the drug). A new computed tomography scan of the chest performed in the 2009 showed an increased size of the enlarged mediastinal lymph nodes associated with compression of the left main bronchus without associated any parenchyma lesion. In 2010 the patients was admitted to another hospital for the presence of left pleural empyema treated with chest tube. In June 2010 was started the treatment with everolimus (0.75 mg twice a day) but a computed tomography scan of the chest performed in January 2012 demonstrated progression of the endobronchial lesion with complete obstruction of the left main bronchus (Fig. 1), associated with left lung atelectasis containing air bubbles some with air-fluid levels. At the same time a bone scintigraphy revealed the presence of osteolytic metastases in the left iliac wing. In February 2012 the patient was admitted to our University Hospital for the presence of recurring hemoptysis and intense dyspnea. The fiberoptic bronchoscopy showed complete occlusion of the left main bronchus and subtotal (90%) occlusion of the right main bronchus (Fig. 2). To remove the right bronchial obstruction we performed a interventional rigid bronchoscopy associated with neodymium-doped yttrium aluminum garnet laser and mechanical disruption, but this procedure determined persistent, massive, bleeding. At this stage the bronchoscopy was interrupted and the right main bronchus was selectively intubated and selective arterial embolization was performed to arrest the bleeding (Fig. 3, 4). At the end of this intervention the patient was hospitalized for three days in our Intensive Care Unit. After his clinical improvement a flexible bronchoscopy showed the complete reopening of the right main bronchus (Fig. 5). The patient was then discharged to home without respiratory symptoms but after three months he was again admitted our hospital in hemorrhagic shock secondary to massive hemoptysis and deceased in our ward after two days.
 Click for large image | Figure 1. Computed tomography scan of the chest showing the tracheal carina (circle) with complete obstruction of the left main bronchus (arrow 1) and stenosis of the right main bronchus (arrow 2). |
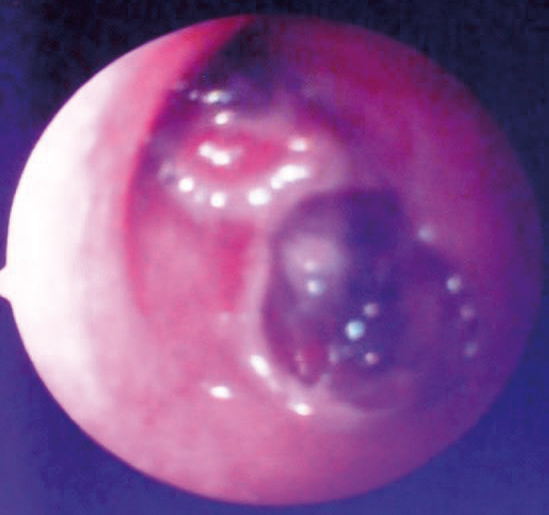 Click for large image | Figure 2. Endoscopic view of the main bronchi before laser resection. |
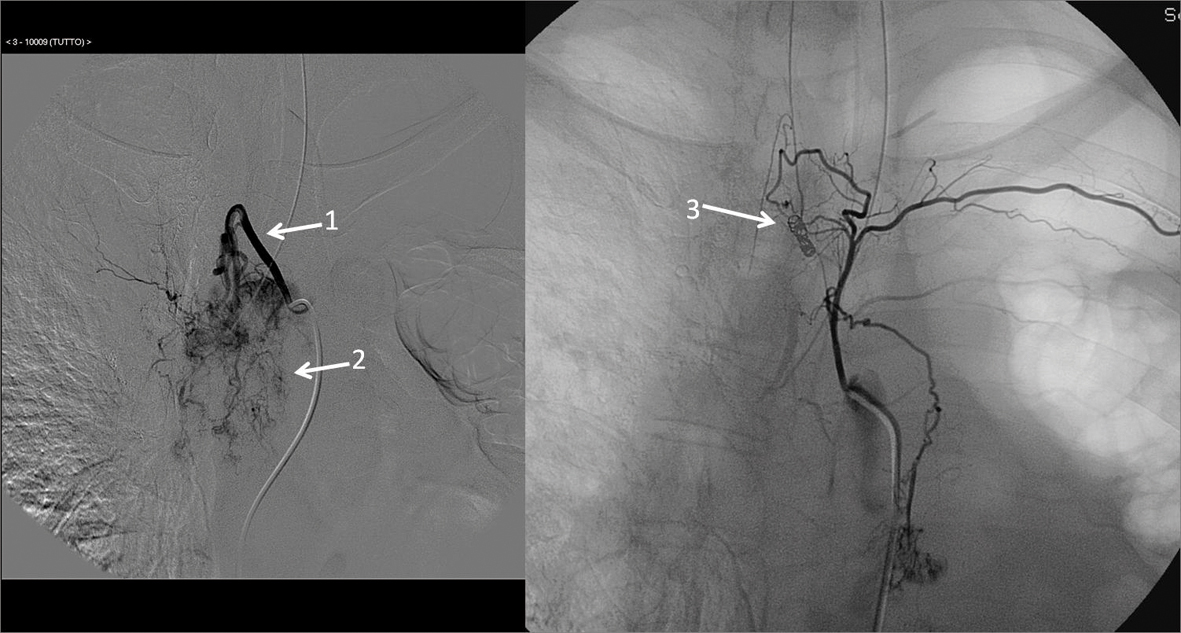 Click for large image | Figure 3. Right intercostal bronchial artery (arrow 1) that supply the neoplasm (arrow 2). Superselective bronchial artery embolization of the right main bronchus with injection of microbeads (250 - 300 micron) and the positioning of four platinum spirals compatible with magnetic resonance imaging (arrow 3). |
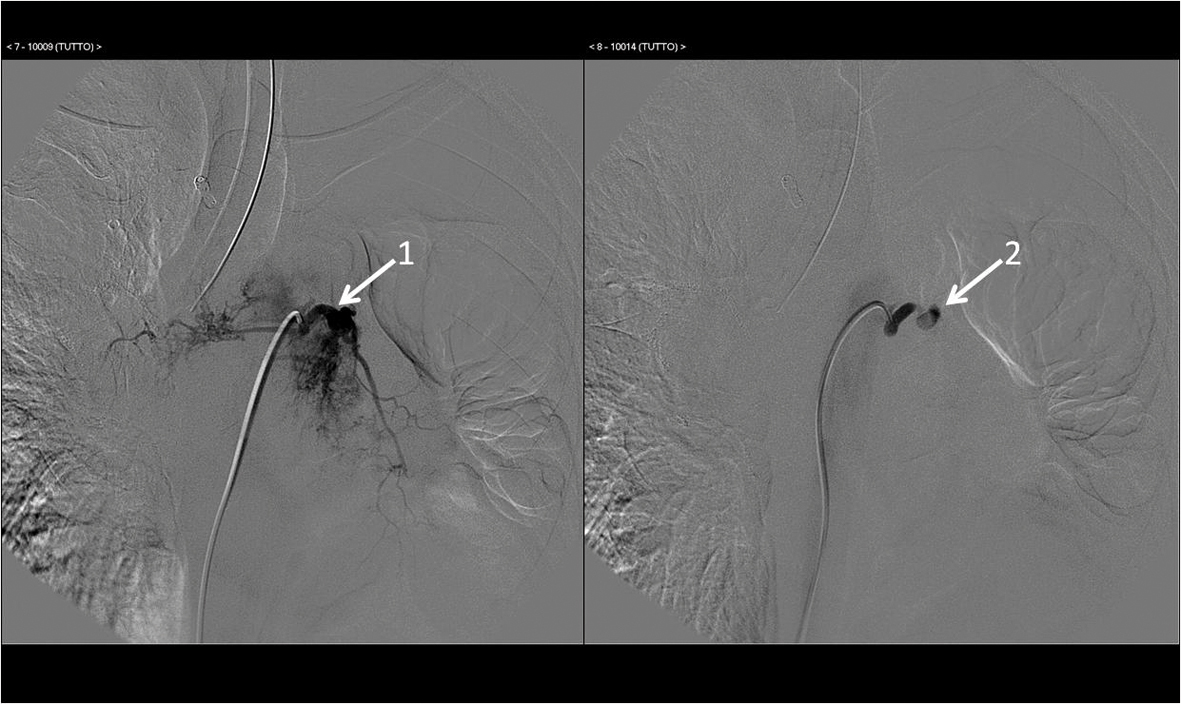 Click for large image | Figure 4. Upper left bronchial artery before (arrow 1) and after (arrow 2) selective embolization of with microbeads (250 - 300 micron). |
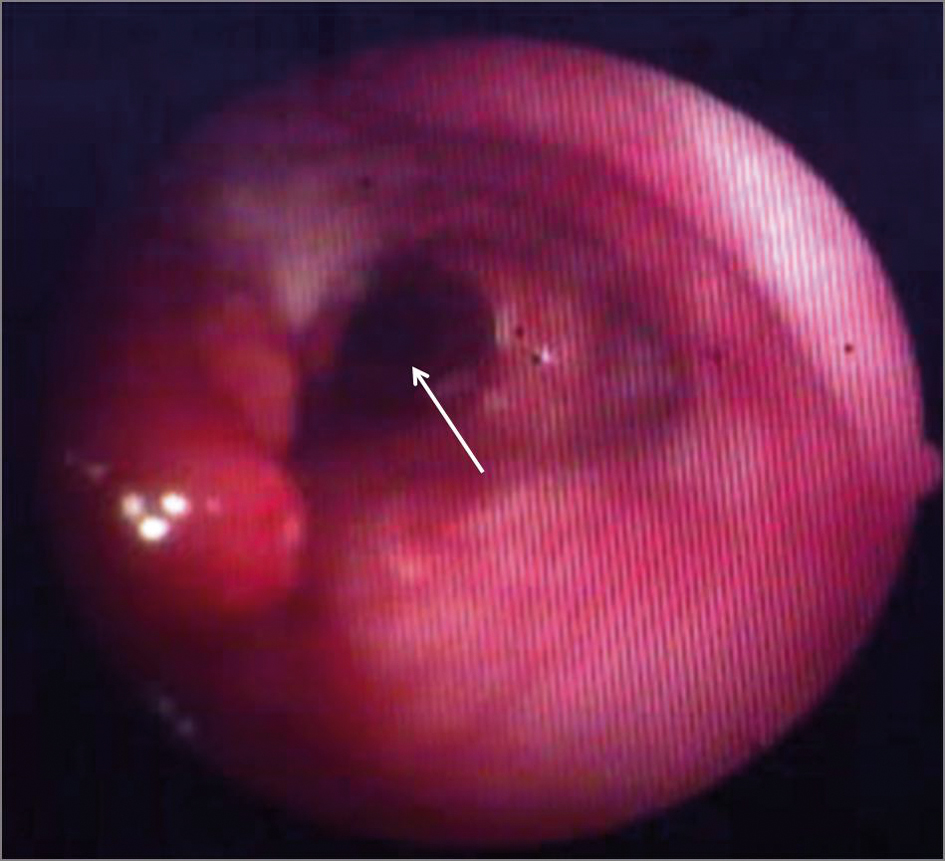 Click for large image | Figure 5. Flexible bronchoscopy showing the complete reopening of the right main bronchus (arrow). |
| Discussion | ▴Top |
We report here the use of emergency bronchial artery embolization to arrest massive bleeding complicating an interventional laser bronchoscopy on endobronchial metastases of renal cell carcinoma, hypervascular tumor. This is a well-accepted and effective treatment for massive and recurrent hemoptysis despite may occasionally cause severe and sometimes life-threatening side effects like spinal cord infarction, transverse myelitis, myocardial infarction [6].
In conclusion, we advice clinicians to pre alert the interventional radiologists of the potential necessity to perform emergency bronchial artery embolization to arrest persistent massive bleeding during endoscopic palliative treatment of large airways obstruction due to metastatic renal cell carcinoma.
Funding
This work has been funded by Fondo di Ateneo per la Ricerca (FAR 2009, 2010, 2011) (ex 60%) Universita di Ferrara (to GC) and an educational grant from the Azienda Ospedaliera Universitaria di Ferrara, Arcispedale S. Anna, Italy.
Conflict of Interest
None.
| References | ▴Top |
- Folch E, Mehta AC. Airway interventions in the tracheobronchial tree. Semin Respir Crit Care Med. 2008;29(4):441-452.
doi pubmed - Seijo LM, Sterman DH. Interventional pulmonology. N Engl J Med. 2001;344(10):740-749.
doi pubmed - Morice RC, Ece T, Ece F, Keus L. Endobronchial argon plasma coagulation for treatment of hemoptysis and neoplastic airway obstruction. Chest. 2001;119(3):781-787.
doi pubmed - Katsimbri PP, Bamias AT, Froudarakis ME, Peponis IA, Constantopoulos SH, Pavlidis NA. Endobronchial metastases secondary to solid tumors: report of eight cases and review of the literature. Lung Cancer. 2000;28(2):163-170.
doi - Sorensen JB. Endobronchial metastases from extrapulmonary solid tumors. Acta Oncol. 2004;43(1):73-79.
doi pubmed - Sopko DR, Smith TP. Bronchial artery embolization for hemoptysis. Semin Intervent Radiol. 2011;28(1):48-62.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


