| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 9, September 2013, pages 612-615
Inferior Vena Cava Filter Thrombosis in Protein-S Deficiency Patient due to Withdrawal of Anticoagulation Therapy After operation
Chang-Bae Sohna, b, Sea-Won Leea, Su-Hong Kima
aCardiovascular center, Department of Internal Medicine, Busan Veterans Hospital, Busan, Republic of Korea
bCorresponding author: Chang-Bae Sohn, Cardiovascular center, Department of Internal Medicine, Busan Veterans Hospital, Busan, Republic of Korea
Manuscript accepted for publication July 18, 2013
Short title: Inferior Vena Cava Filter Thrombosis
doi: https://doi.org/10.4021/jmc1417w
| Abstract | ▴Top |
In protein S deficiency, if there was recurrent thrombotic event, ongoing anti-coagulation therapy should be administered. Especially, in case of life threatening recurrent pulmonary embolism, prophylactic inferior vena cava (IVC) filter with anti-coagulation therapy may be considered. But until now, there is no definite guideline for anti-coagulation therapy duration about recurrent thrombotic events in protein S deficiency patients. A 64-year old male patient who already was diagnosed with protein S deficiency accompanied with recurrent pulmonary embolism and was performed IVC filter was referred to our hospital due to manage both leg edema after operation. In the abdominal CT, we could find IVC filter thrombosis occurred to withdrawal anti-coagulation therapy for 2 weeks after spine operation. So we performed catheter-based procedure with anti-coagulation therapy and successfully treated IVC filter thrombosis.
Keywords: Inferior vena cava; Filter thrombosis; Protein S deficiency; Pulmonary embolism
| Introduction | ▴Top |
For the last 30 years, inferior vena cava (IVC) filters have widely been used to prevent pulmonary embolism. A pulmonary embolism is a serious acute disease that causes pulmonary function insufficiency and right ventricular failure as blood clot generated from lower cardiac arrhythmia blocks pulmonary artery, which may progress to a hemodynamic compromise.
To treat and prevent this pulmonary artery thrombosis, anticoagulation therapy using a Vitamin K antagonist is primary used, but if it relapses repetitively or has other risk factors, to prevent a systemic embolization, the IVC filter is used.
Protein S acts as a supplementary factor of Protein C and blocks the activation of Factors Va and VIIIa, showing an anticoagulant action, and lacking it may cause a repetitive thrombopoiesis. So in case of protein S deficiency, a continuous anticoagulant therapy is necessary. The authors have experienced and treated IVC filter thrombosis due to the withdrawal of anticoagulant therapy after the operation in the patient having an IVC filter inserted in order to treat recurrent pulmonary embolism in Protein S deficiency patient, so now it is being reported with reviews of literature.
| Case Report | ▴Top |
A 64-year-old male patient complaining of both legs pitting edema lasting for 2 weeks was transferred to our hospital emergency room from another hospital. The patient was diagnosed with an acute pulmonary embolism in April 2010 and treated, and in the examination of the disease of the cause for thrombosis carried out at the time, Protein S activity was reduced to 34%, which was confirmed to be Type 2 Protein S deficiency. Then, anticoagulation therapy was carried out in the outpatient clinic using a Vitamin K antagonist for 6 months, and anti-platelet therapy continued shifting to Aspirin.
In September 2011, the patient complaining of labored respiration visited our hospital's emergency room, and we performed the echocardiography at the time, dilatation and hypokinesia of the right ventricle was not observed, but a slight pulmonary artery high blood pressure (right ventricular systolic pressure; 45 mmHg) was identified, which increased to D-dimer 2.44 µg/mL, and in a chest CT scan, and in the right pulmonary artery, pulmonary embolism recurrence could be identified. It was diagnosed as a recurrent acute pulmonary embolism by Protein S deficiency, and an anticoagulation therapy using heparin was resumed, and then for relapse prevention, an IVC filter was inserted, and a lifelong anticoagulation therapy with Vitamin K antagonist was planned and outpatient treatment continued.
In February 2013, the patient was carried out the 7 - 12th T-spine inter-body infusion operation on February 22, 2013 at another hospital for the 9 and 10th thoracic spine compression fracture because of fall down during exercising and ankylosing spondylitis, and after the operation, anticoagulation therapy had been withdrawn. Since March 1, 2013 about 3 weeks after the withdrawal of the anticoagulation therapy, patient had progressed both leg edema, an IVC filter thrombus was found on chest CT (phase 3 dynamic study CE) (Fig. 1) and D-dimer was checked over 10.0 µg /mL at another hospital, and the patient was transferred to our hospital to continue the further management. In the peripheral blood examination carried out in our hospital, white blood cells were 7,890/mm3 (Neutrophil 56.9%) and hemoglobin was 10.2 g/dL, platelet 350,000/mm3, and in the serum biochemical examination, AST/ALT were 28/22 IU/L, blood urea nitrogen was 18 mg/dL, and creatinine was 1.0 mg/dL. hs-CRP 3.95 mg/dL and had increased to D-dimer 3.66 µg /mL.
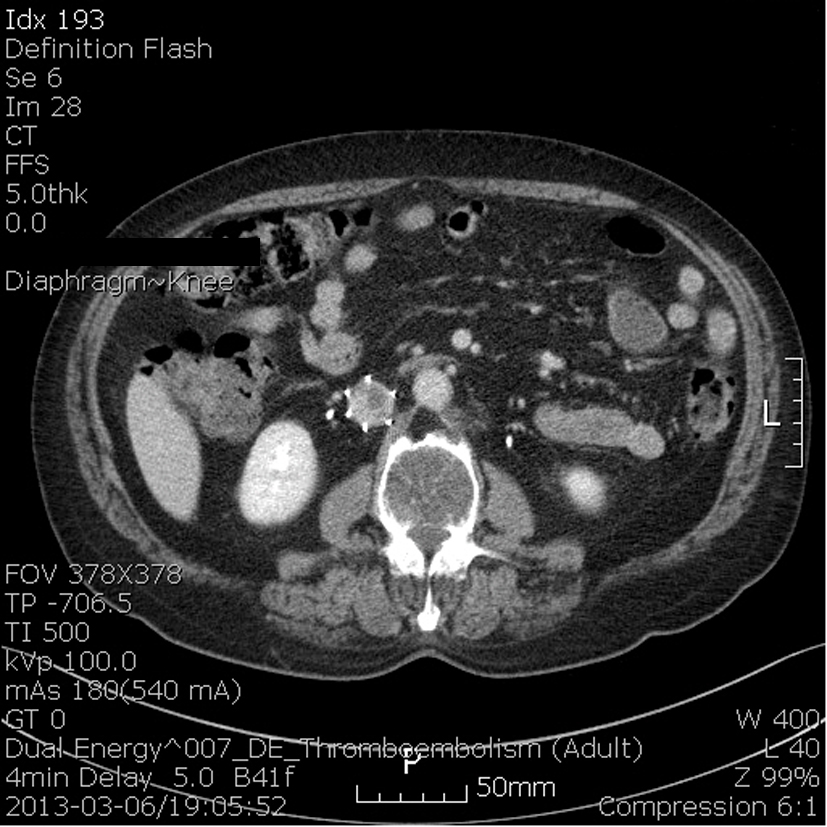 Click for large image | Figure 1. Abdomen computer tomography shows intraluminal filling defect in IVC filter. |
For the treatment, using low molecular weight heparin (Enoxaparin sodium; 1 mg/kg, twice a day; clexane, Sanofi-Aventis, Maison Alfort, France), and then we performed peripheral intervention for the IVC filter thrombus found on abdomen & pelvis enhanced CT on March 18, 2013. The IVC filter already got endothelialization, so could not be removed, and thrombus aspiration was not made, so a mechanical thrombectomy using a pigtail catheter was carried out through a rolling technique (Fig. 2, 3). Later, we continued both the aspirin and warfarin using once a day and it was maintained at INR 1.5 - 1.7. The patient showed improvement in both leg edemas after the treatment, and a state of improved thrombus in f/u abdomen CT was identified (Fig. 4). Then, the patient was transferred to another hospital to continue aftercare of post-operation of T-spine 7th - 12th inter-body infusion.
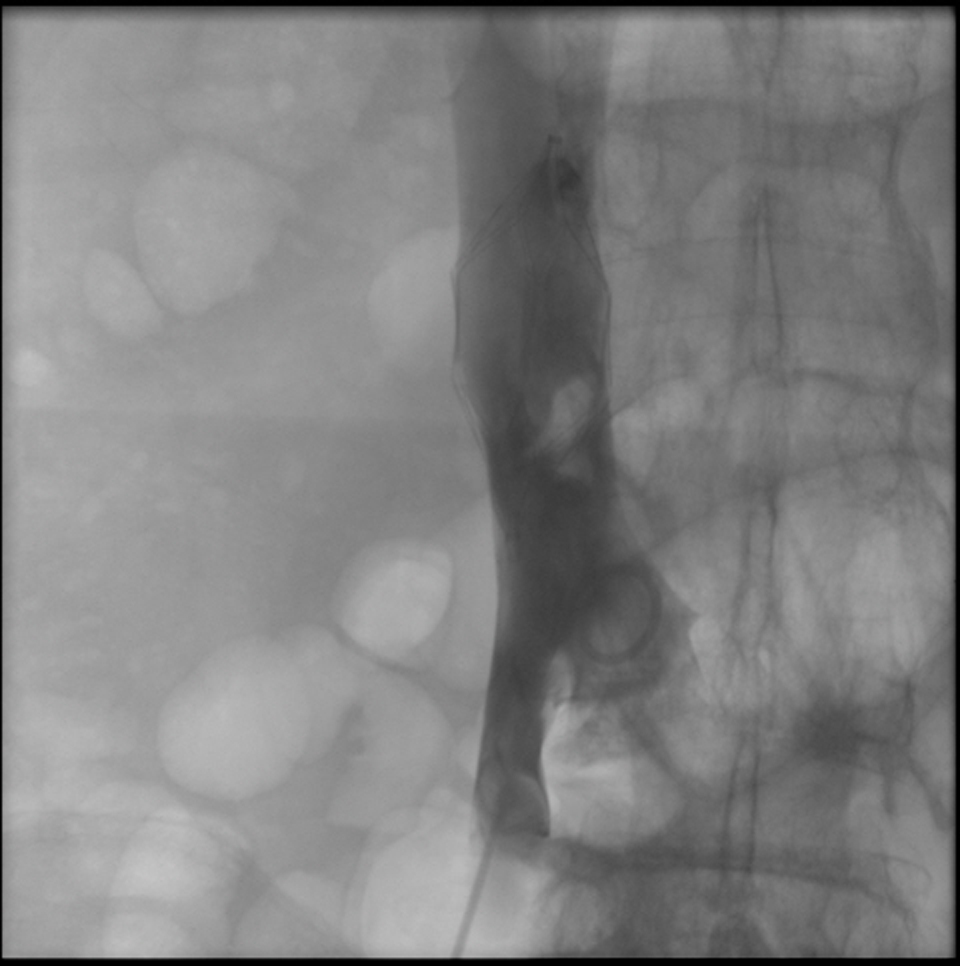 Click for large image | Figure 2. IVC angiography shows thrombus in IVC filter. |
 Click for large image | Figure 3. Mechanical thrombectomy by rolling technique via catheter. |
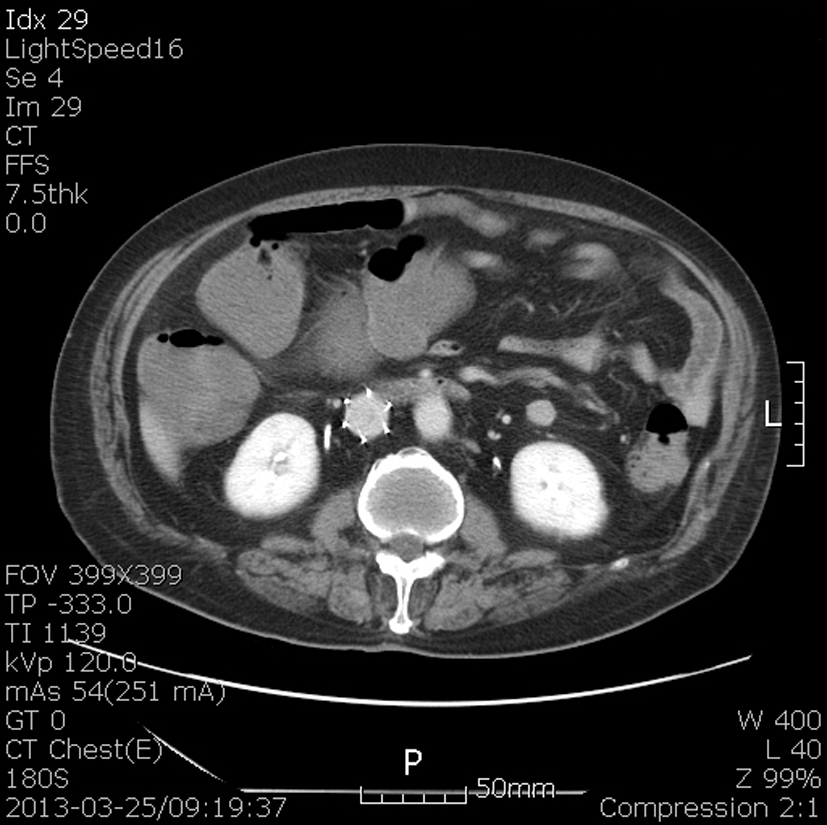 Click for large image | Figure 4. Improvement the thrombus after procedure and anti-coagulation therapy at follow up abdominal computer tomography. |
| Discussion | ▴Top |
An IVC filter is a device that has been used for primary thrombo-prophylaxis for the last 30 years [1]. Especially, it has been in clinical service for trauma, Bariatric surgery, neurosurgery, cancer, intensive care unit populations, and relative contra-indication to anticoagluation patients. A thromboembolic disease is one with high morbidity and mortality, and the number of patients who die from PE annually is 300,000 persons, and especially, there are a lot of incidences in trauma, post operation, cancer and ICU patients [2]. An optimal IVC filter is used as thromboprophylaxis in the patients with such high major thromboembolic risks, and according to Decousus H et al., in 1999 - 2008, in pre-existing DVT patients even though who do not have definite DVT or PE currently, prophylactic insertion of IVC filter rate was doubled [3].
The IVC filter thrombosis is a disease in which a thrombus occurs in an IVC filter at 2.9 - 22% [4]. The thrombus within the IVC filter may appear in various aspects from a small asymptomatic thrombus to a critical IVC occlusion. Its symptoms include mild ambulatory leg swelling and limb-threatening ischemia, and among them, with a big thrombus burden, significant lower extremity edema and pain and severe complications such as sensory deficits, venous stasis, or ulceration may occur. Ahmad et al. evaluated the filter thrombosis rates of 1,718 patients who has IVC filter through Computed Tomography (CT) and as a result, some degree of IVC filter thrombosis was observed in 18.6% of all patients. The vast majority (> 98%) of these patients were asymptomatic, and total occlusion of the filter-bearing IVC was seen only in 2% of the patients who had a filter thrombus (< 0.4% of all patients) [5].
For the evaluation of IVC filter thrombosis, Doppler US is considered preferentially. And yet, Doppler US has a limit in the IVC filter evaluation, so usually, to find IVC filter thrombosis, contrast-enhanced CT is used as the 1st diagnostic modality. By contrast-enhanced CT, the location and extent of clot burden and the degree of occlusion can be analyzed. In addition, Venography can be used to confirm and for intervention even though it was the invasive.
There has been no treatment reported for IVC filter-related thrombosis until now and mostly it is treated by endovascular management [6]. Anticoagulation therapy should immediately start in the most symptomatic patients if there is no contraindication. In 1988, Angel et al. reported a catheter-directed thrombolysis and an adjunctive balloon angioplasty [7], and in 1994, Hansen et al. reported pulse-spray technique using thrombolysis for the first time [4]. In addition, if there is neointimal hyperplasia, balloon venoplasty can be considered, and if there is a chronic occlusion, there is a method of stent insertion as an alternative method [8]. Recently, endovascular thrombectomy using Angiojet system or Trellis system can be used, and if there is an excessive symptom in a state in which an endovascular intervention is impossible, surgical venous thrombectomy or bypass surgery may be considered.
Protein S is a glycoprotein containing r-carboxylated glutamic acid, and 60% of Protein S is combined with C4b binding Protein and 40% is combined with activated Protein C, irreversibly inactivating Factors Va and VIIIa to control the action of thrombin. Protein S deficiency occurring by Protein S gene mutations are divided into three types. They are defined as follows: In Type 1, both total Protein S level and free Protein S level and activity have been reduced; Type 2 has a normal free Protein S level, but its activity has been reduced; and Type 3 has a normal total Protein S level but its free Protein S has been reduced and its activity has fallen [8].
Sanson et al. reported that in 70 persons with asymptomatic Protein S deficiency, the annual thromboembolic event was 0.4% [9]. According to the 2008 ESC guideline, if there is a reversible risk factor to prevent relapse in pulmonary embolism patient, anticoagulation therapy is recommended for 3 months, and if other risk factors are accompanying or there is no special risk factor, it is instructed that anticoagulation therapy should be carried out for more than 3 months, but if there is a Protein S deficiency, for a thromboembolic event, there is no clear guideline for using a vitamin K antagonist yet.
In this case, for recurrent pulmonary embolism due to Protein S deficiency, a lifelong anticoagulation therapy has been carried out and prophylactic IVC filter was inserted. But for spine operation, anticoagulation therapy had been stopped for 2 weeks and then the IVC filter thrombosis occurred. Both leg edema and large burden IVC filter thrombus on CT angiography were observed, so anticoagulation therapy was restarted and catheter-based intervention was carried out to succeed in treatment and improve the symptoms. In this case, since there is a past history of the irreversible risk factor of Type 2 Protein S deficiency and a recurrent pulmonary embolism, later, the lifelong anticoagulation therapy should continue using a vitamin K antagonist.
| References | ▴Top |
- Wehrenberg-Klee E, Stavropoulos SW. Inferior vena cava filters for primary prophylaxis: when are they indicated? Semin Intervent Radiol. 2012;29(1):29-35.
doi pubmed - Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ, 3rd. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158(6):585-593.
doi pubmed - Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prevention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338(7):409-415.
doi pubmed - Hansen ME, Miller GL, 3rd, Starks KC. Pulse-spray thrombolysis of inferior vena cava thrombosis complicating filter placement. Cardiovasc Intervent Radiol. 1994;17(1):38-40.
doi pubmed - Ahmad I, Yeddula K, Wicky S, Kalva SP. Clinical sequelae of thrombus in an inferior vena cava filter. Cardiovasc Intervent Radiol. 2010;33(2):285-289.
doi pubmed - Tarry WC, Makhoul RG, Tisnado J, Posner MP, Sobel M, Lee HM. Catheter-directed thrombolysis following vena cava filtration for severe deep venous thrombosis. Ann Vasc Surg. 1994;8(6):583-590.
doi pubmed - Angle JF, Matsumoto AH, Al Shammari M, Hagspiel KD, Spinosa DJ, Humphries JE. Transcatheter regional urokinase therapy in the management of inferior vena cava thrombosis. J Vasc Interv Radiol. 1998;9(6):917-925.
doi - Golarz SR, Grimsley B. Use of Wall stent to exclude a thrombosed inferior vena cava filter. Ann Vasc Surg. 2010;24(5):690 e695-697.
- Sanson BJ, Simioni P, Tormene D, Moia M, Friederich PW, Huisman MV, Prandoni P, et al. The incidence of venous thromboembolism in asymptomatic carriers of a deficiency of antithrombin, protein C, or protein S: a prospective cohort study. Blood. 1999;94(11):3702-3706.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


