| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 1, Number 1, August 2010, pages 6-7
Epidermoid Cyst of the Testis Misdiagnosed as a Hydrocele: A Case Report
Jessica Harveya, Aidan P. Noonb, d, Steven Beckc, Patrick Cutinhab
aThe University of Sheffield Medical School, Beech Hill Road, Sheffield S10 2RX, UK
bDepartment of Urology, Barnsley Hospital NHSFT, Gawber Rd, Barnsley, South Yorkshire, UK
cDepartment of Pathology, Barnsley Hospital NHSFT, Gawber Rd, Barnsley, South Yorkshire, UK
dCorresponding author: Aidan P. Noon, Department of Urology, Barnsley Hospital NHSFT, Gawber Rd, Barnsley, South Yorkshire, UK
Manuscript accepted for publication July 1, 2010
Short title: Epidermoid Cyst of the Testis
doi: https://doi.org/10.4021/jmc2010.07.109e
| Abstract | ▴Top |
We present a case of a 63 years old patient who presented with a slow-growing, painless testicular swelling clinically diagnosed as a hydrocele. The patient underwent elective hydrocele repair, where it became apparent that the diagnosis of a hydrocele was incorrect. On incision of the presumed hydrocele sac, a caseous material was encountered and no obvious healthy testicle was apparent. An orchidectomy was performed and pathological assessment revealed the lesion to be an epidermoid cyst; a rare benign lesion of the testicle that clinicians should consider when assessing scrotal swellings.
Keywords: Epidermoid cyst; Hydrocele; Orchidectomy
| Introduction | ▴Top |
Benign epidermoid cysts account for around 2% of all testicular tumors. Identified in 1942 their etiology still remains to be confirmed [1]. Although well documented in the literature, this rare lesion may not be considered by clinicians assessing a scrotal lump. This case report illustrates how an epidermoid cyst may be misdiagnosed as a hydrocele on clinical assessment only. It is hoped this case report will inform clinicians about this rare tumor and illustrate the need for ultra-sound assessment of lumps before surgical treatment.
| Case Report | ▴Top |
A 63 years old male presented with a five year history of a slowly enlarging, painless swelling of the left testis. He had been seen in urology clinic one year previously and diagnosed clinically as having a hydrocele. Due to the size of the swelling and associated discomfort the patient now wished to be considered for surgery. Once again clinical examination found a large, lax, soft, non-tender swelling confined to the scrotum. The patient was counselled and scheduled to undergo a hydrocele repair as a day-case procedure.
The procedure was performed under general anaesthetic. The “hydrocele sac” was delivered through a midline scrotal incision. Incision of the presumed tunica vaginalis revealed it to contain green caseous material (Fig. 1). It was not possible intra-operatively to define a healthy or viable testicle separate from the mass. The patient had a normal sized contra-lateral testicle and the decision was taken to perform an orchidectomy. The specimen was sent for pathological assessment.
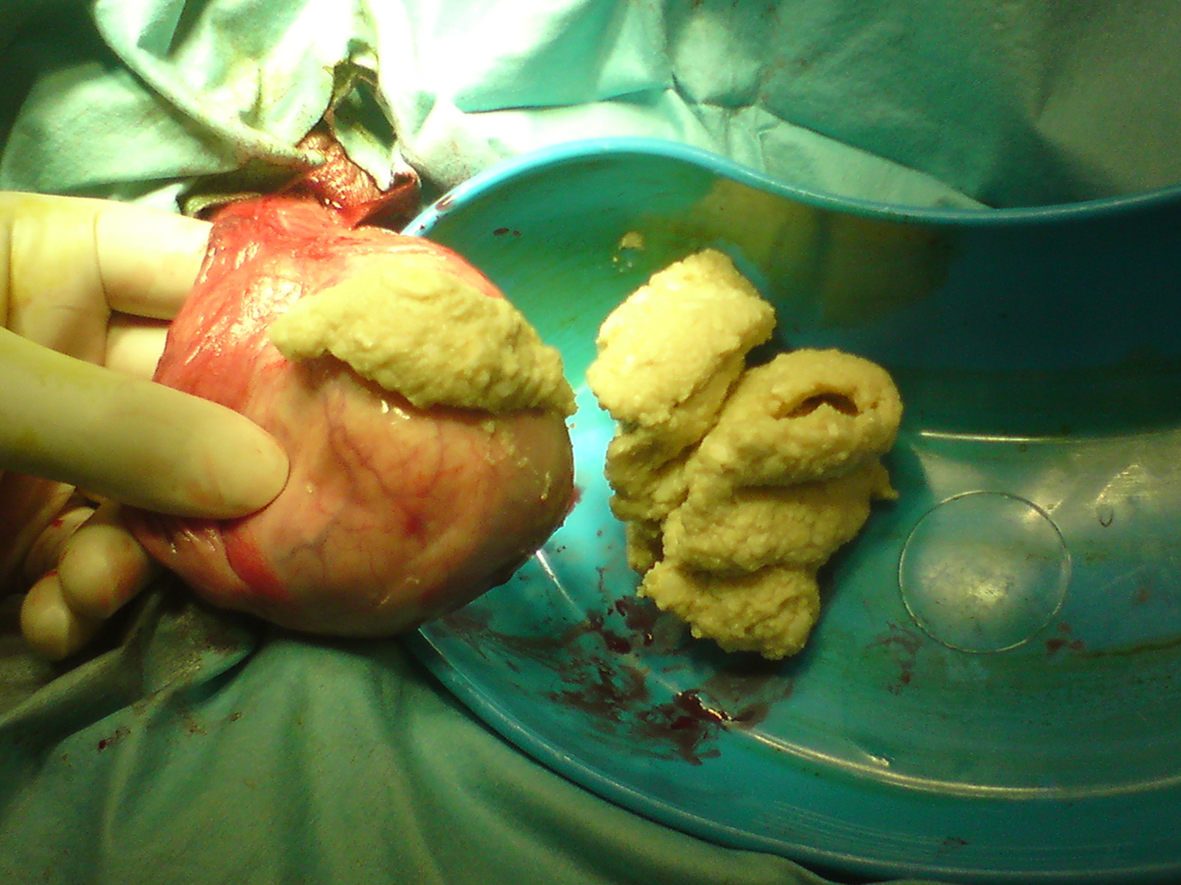 Click for large image | Figure 1. The incised testicular lesion revealed a caseous material. Pathological assessment revealed the lesion to be an epidermoid cyst. |
The specimen consisted of a testicular mass, 110 mm in maximum dimension with a smooth outer surface and a single thin-walled cyst replacing most of the testis. The cyst contained soft, friable, pale material. Microscopy showed a benign epidermoid cyst with no other tissues present (Fig. 2). The patient made a complete recovery.
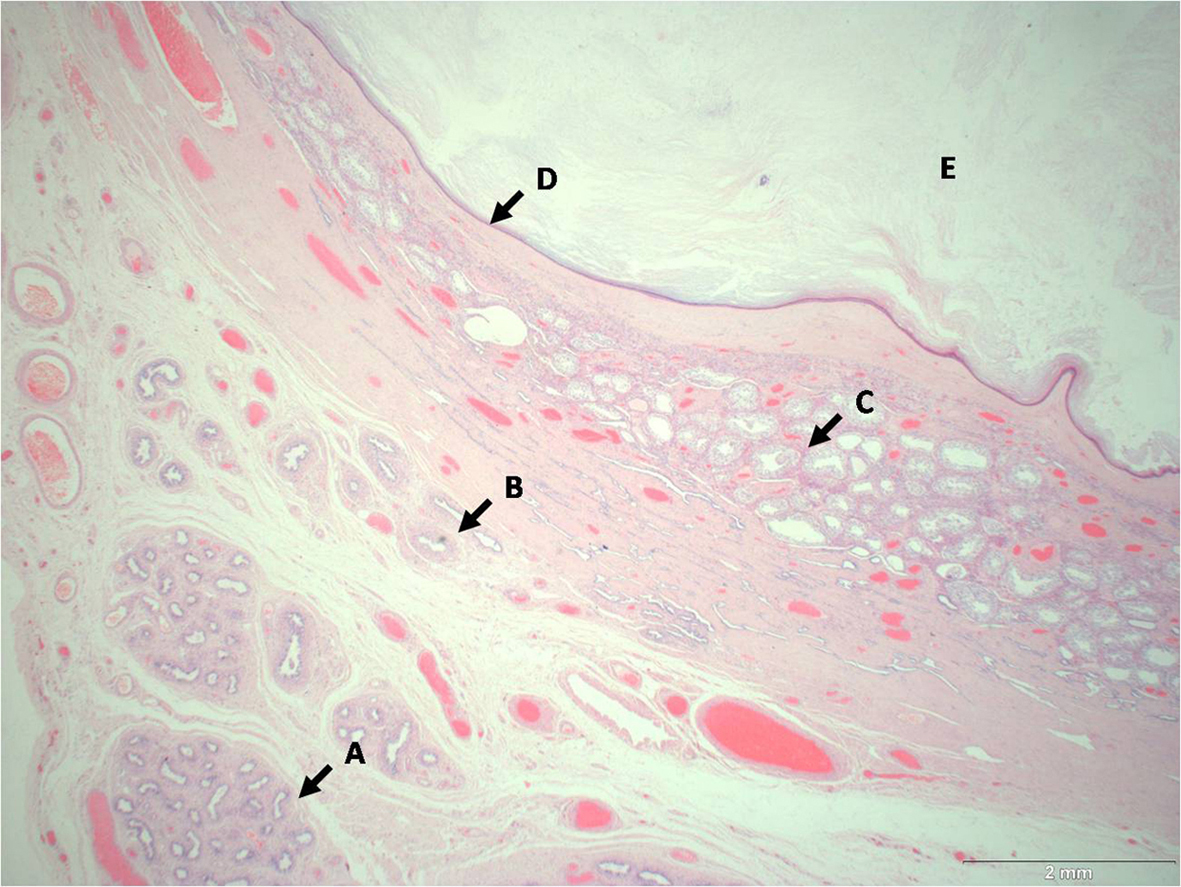 Click for large image | Figure 2. x10 magnification of the H & E stained epidermoid cyst. A: Epididymis; B: Rete Testis; C: Seminiferous tubules; D: Epidermoid cyst wall; E; Cyst contents. |
| Discussion | ▴Top |
Epidermoid cysts (ECs) of the testis are benign ectodermal tumors. They account for approximately 1% of testicular tumors in adults with a peak in the third decade [2]. Price [3] defined them as intra-testicular, squamous, epithelial-lined cysts containing keratinised material with neither teratomatous nor adnexal elements. The main differential diagnosis is a teratoma. ECs occur in a similar age group to teratomas prompting workers to suggest that ECs are monodermal, benign equivalents [3, 4]. However, this assertion remains controversial since others have suggested that ECs are in fact sub-types of germ cell tumors [2]. The testicular tumor markers α-fetoprotein and βHCG, raised with germ cell tumors, are normal with ECs [1]. Usually ECs can be diagnosed by ultrasonography which may reveal a classical onion-ring appearance. Maizlin [1] and Johnson [5] have reported that this sign is non-specific and do not support isolated ultrasonographic diagnosis. If the clinical profile is that of a slow-growing, small, intra-testicular tumor with negative tumor markers within a normal testis, testicular-sparing surgery with follow-up has been advocated in the younger patient [3].
In our case the use of scrotal trans-illumination may have altered the clinical diagnosis of a hydrocele. A pre-operative ultrasound scan again may possibly have identified an EC or at least excluded a simple hydrocoele. The patient could then have been counselled and scheduled for an orchidectomy. As a result of our experience with this case we will have a lower threshold for requesting testicular ultrasound. Patients not undergoing ultrasound prior to hydrocele repair should be counselled in the risk of orchidectomy should unanticipated pathology be encountered.
Conflict of Interest
None.
| References | ▴Top |
- Maizlin ZV, Belenky A, Baniel J, Gottlieb P, Sandbank J, Strauss S. Epidermoid cyst and teratoma of the testis: sonographic and histologic similarities. J Ultrasound Med 2005;24(10):1403-1409; quiz 1410-1401.
pubmed - Shah KH, Maxted WC, Chun B. Epidermoid cysts of the testis: a report of three cases and an analysis of 141 cases from the world literature. Cancer 1981;47(3):577-582.
pubmed doidoi - Heidenreich A, Zumbe J, Vorreuther R, Klotz T, Vietsch H, Engelmann UH. [Testicular epidermoid cyst: orchiectomy or enucleation resection?]. Urologe A 1996;35(1):1-5.
pubmed - Umar SA, MacLennan GT. Epidermoid cyst of the testis. J Urol 2008;180(1):335.
pubmed doi - Johnson JW, Hodge EE, Radwin HM. Epidermoid cyst of testis: a case for orchiectomy. Urology 1987;29(1):23-25.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


