| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 9, September 2014, pages 505-508
Occult Vertebral Osteomyelitis, a Diagnostic Conundrum
Brijesh Patela, c, Adam Formana, Vilma Drelichmanb, Michael Marshalla
aDepartment of Internal Medicine, Providence Hospital and Medical Center, 16001 W Nile Mile Road, Southfield, MI 48075, USA
bDepartment of Infectious Disease, Providence Hospital and Medical Center, 16001 W Nile Mile Road, Southfield, MI 48075, USA
cCorresponding Author: Brijesh Patela, Department of Internal Medicine, Providence Hospital and Medical Center, 16001 W Nile Mile Road, Southfield, MI 48075, USA
Manuscript accepted for publication March 31, 2014
Short title: Occult Vertebral Osteomyelitis
doi: https://doi.org/10.14740/jmc1753w
| Abstract | ▴Top |
Vertebral osteomyelitis is a well-known but uncommon condition. Typical presenting features include fever, back pain with local tenderness and neurologic symptoms. In absence of these typical findings, vertebral osteomyelitis can be difficult to diagnose. Staphylococcus species are the most common causes. In most cases, inflammatory markers are elevated. Blood cultures can be very useful to identify the culprit organism(s). Though various imaging modalities are available, an MRI is considered gold standard for the diagnosis. Our patient presents with non-specific abdominal pain that masqueraded vertebral osteomyelitis leading to paralysis.
Keywords: Vertebral osteomyelitis; WBC scan; Abdominal pain; Pleural effusion
| Introduction | ▴Top |
Vertebral osteomyelitis is a rare (2.4/100,000) condition that can be difficult for the most experienced practitioner to diagnose. Vertebral osteomyelitis may refer to spinal osteomyelitis, spondylodiskitis, septic diskitis or disk-space infection. The course can be acute, subacute or chronic [1].
The main route of infection to the vertebral column is hematogenous spread through the segmental arteries [2]. Other routes of infection include direct extension to the bone after spinal surgery or nearby soft tissue infection [3]. Once the infection takes place in the bone, the patients are at risk of developing complications such as epidural abscess. Bone infections are predominantly caused by pyogenic organisms; however, any organisms can infect bones. Staphylococcus species followed by E. coli are the most common cause of vertebral osteomyelitis.
The most common presenting symptom of vertebral osteomyelitis is back pain. About 86% of vertebral osteomyelitis patients have localized back pain; fever is common in up to 60% of the patients [4]. Tenderness of spine upon percussion over the affected area may be present in up to 20% of epidural abscess patients [5]. Back pain, fever, localized tenderness over the spine, and neurologic symptoms such as paresthesia or paralysis, are “red flag” symptoms for vertebral osteomyelitis. Rare cases of epidural abscesses have been reported as painless or non-specific, abdominal pain, chest pain and pleural effusion [6-9]. These unusual presentations pose a great challenge for clinician to diagnose what is already a rare condition. Therefore, these cases are often missed and patients present in devastated conditions.
| Case Report | ▴Top |
In December 2012, a 43-year-old African-American male presented to our hospital complaining of abdominal pain that has been persistent for 3 days. The patient described pain as “someone kicked him” in the abdomen and rated it at 9/10 intensity. It was located in epigastric region, non-radiating and without aggravating or alleviating factors. The patient had been experiencing bloating and belching, without constipation or vomiting. Past medical history was significant for diabetes, hypertension and osteomyelitis of the left foot. His vital signs were within normal limits. On physical exam, he had decreased breath sounds bilaterally. The distal left foot was erythrematous and slight pururent discharge was draining. A chest X-ray revealed asymmetric pleural effusion (Fig. 1), which was confirmed by CT of the thorax (Fig. 2). Subsequently, he underwent for thoracocentesis reflecting an exudative process and grew no organisms. The laboratory workup showed leukocytosis of 17,000 cells/dL (normal: 4 - 10). The C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were elevated at 78.1 mg/L (normal: 0 - 10) and 126 mm/h (normal: 0 - 15), respectively.
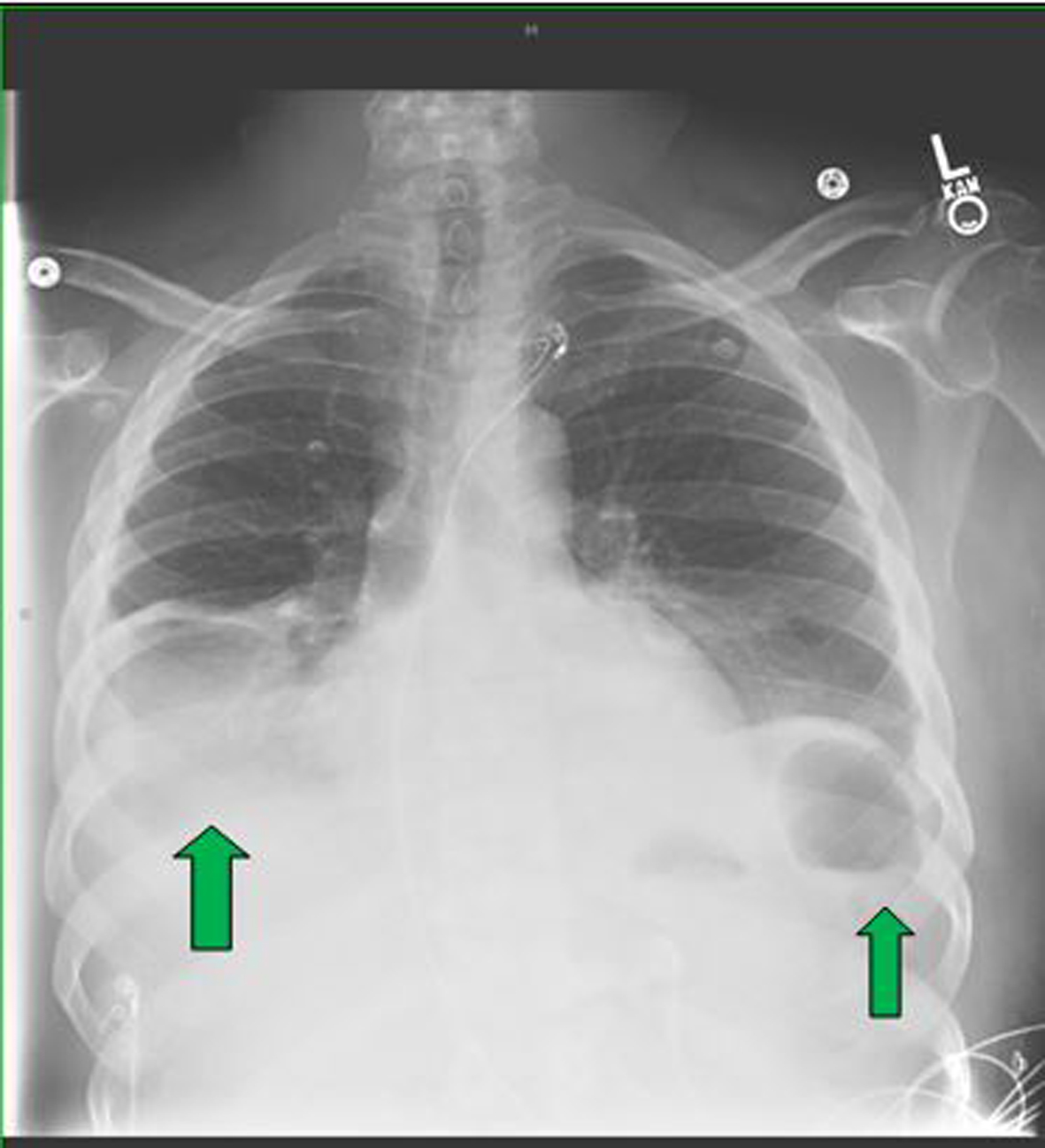 Click for large image | Figure 1. The initial chest X-ray revealed bilateral pleural effusion, markedly greater on the right than the left side (green arrows). |
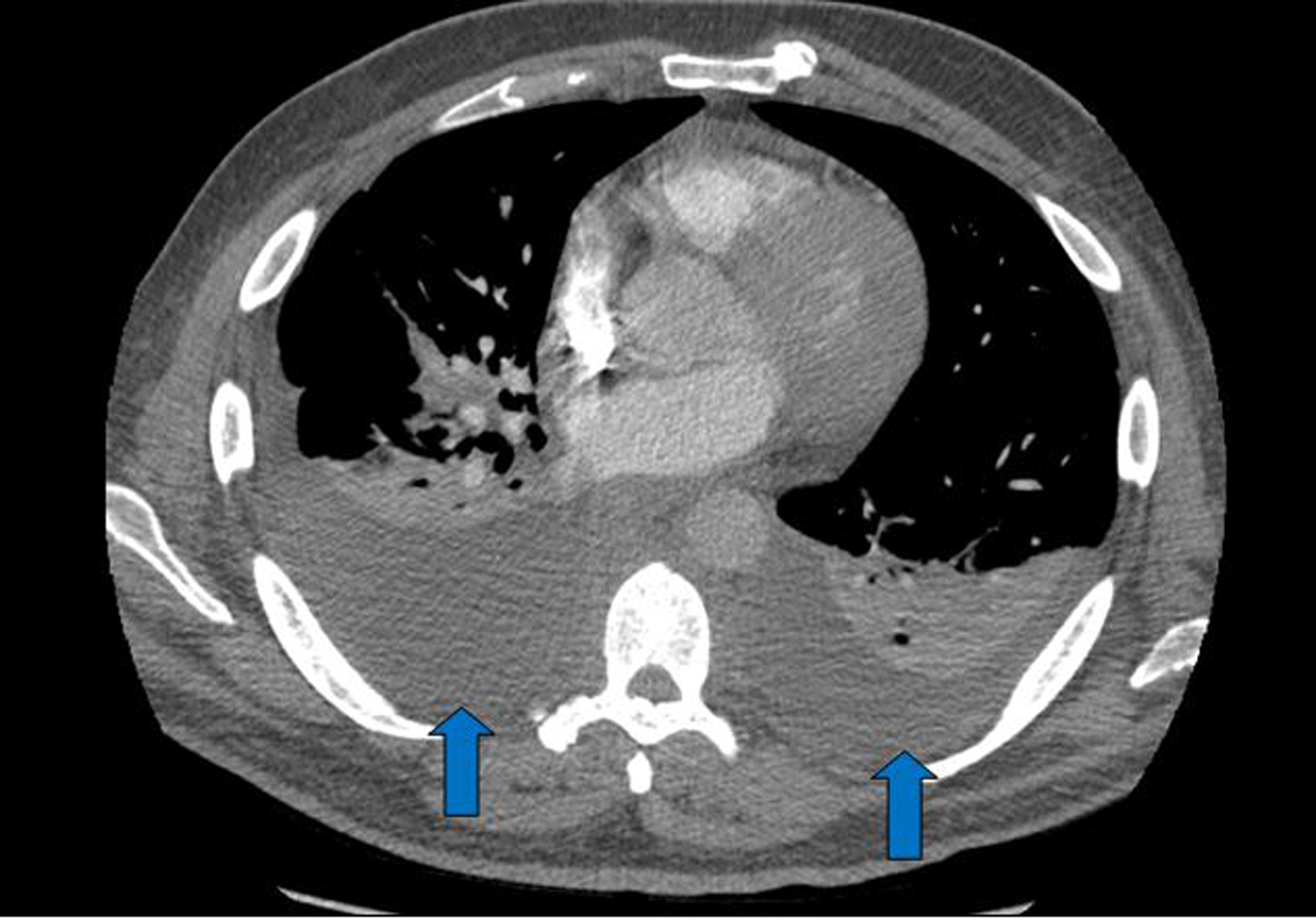 Click for large image | Figure 2. The CT scan revealed asymmetric pleural effusion more on right pleural space than the left (blue arrows). |
For suspected recurrent osteomyelitis of the foot, blood cultures and empirical antibiotics were promptly initiated. Later, the blood cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA). The patient was allergic to vancomycin; therefore, he was started on IV daptomycin based on sensitivity analysis by an infectious disease physician. Despite the antibiotic therapy, he had persistent MRSA bacteremia. The further workup to identify source of infection included transesophageal echocardiography (TEE), indium-111-labeled leukocyte scintigraphy (WBC scan). The latter revealed activity in the left foot but they did not reveal in the spinal column (Fig. 3, 4); similar findings were detected in the bone scan. The TEE was negative for valvular vegetations. The abdominal and chest pain improved. The patient was discharged home with a diagnosis of osteomyelitis and a 6-week course of IV daptomycin.
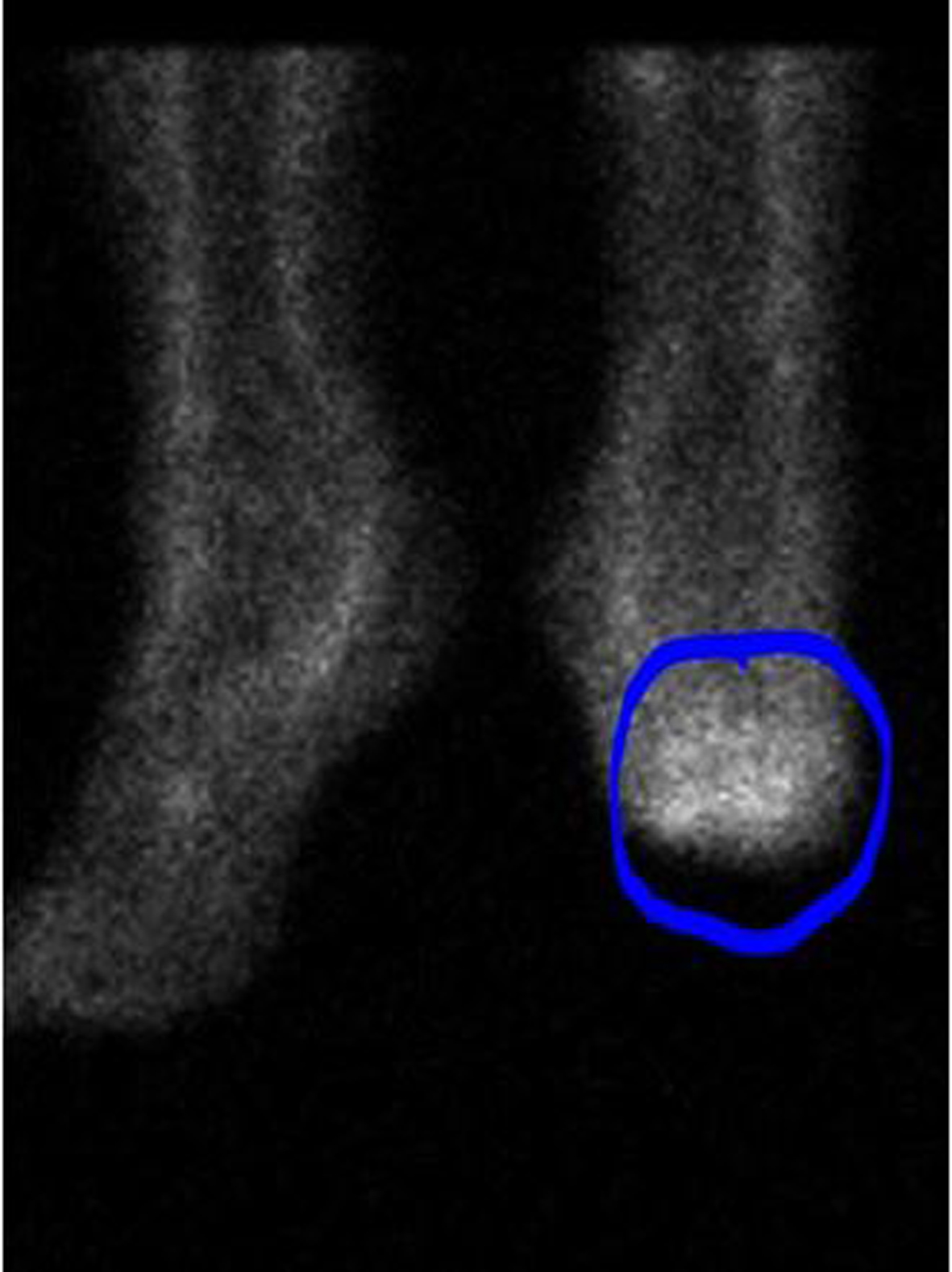 Click for large image | Figure 3. The WBC scan showed increased tracer activity in the left foot suggesting active inflammation (blue circle). |
 Click for large image | Figure 4. The whole body WBC scan did not reveal any tracer activity in the body. |
In February 2013, the patient returned to the emergency department complaining of similar abdominal pain. The patient stated he was constipated. He had not had a bowel movement in 5 days. During the hospitalization he had no back pain, no fever and no neurologic deficits. As the hospital course progressed, his pain improved. On day 5, the patient complained of abrupt loss of sensation and motor function of bilateral lower extremities below T8 level. At this time, an emergent MRI of the spine was ordered for suspected spinal cord etiology. The MRI revealed epidural abscess and vertebral osteomyelitis (Fig. 5). He was emergently taken to operating room by the neurosurgical team. After 2 weeks, he was discharged to rehabilitation facility with no improvement in his neurologic deficit.
 Click for large image | Figure 5. The emergent MRI scan showed T7-8 discitis and osteomyelitis associated with epidural phlegmon resulting in cord compression and edema (red arrows). |
| Discussion | ▴Top |
The diagnosis of vertebral osteomyelitis requires high index of suspicion. Early diagnosis is imperative to prevent devastating sequelae. In the absence of the “red flag” symptoms, clinicians may miss an opportunity to diagnose vertebral osteomyelitis. Our case highlights an unusual presentation of vertebral osteomyelitis that was masqueraded by recurrent abdominal pain. The exact mechanism behind the patient’s exudative pleural effusion without organisms is unclear, though direct extension from infected vertebral body and sympathetic process are considered possible etiology [8].
Accurate and early diagnosis of vertebral osteomyelitis depends on appropriate diagnostic testing. A complete blood count is reasonable initial step. In most cases, vertebral osteomyelitis may show neutrophil-predominant leukocytosis, which has low sensitivity for the diagnosis [1]. In contrast, inflammatory markers such as ESR and CRP are highly sensitive. The most preferred diagnostic modality is an MRI of the spine which has a 90% accuracy [10]. Cases in which an MRI is contraindicated, a CT scan or gallium-67 citrate scan can be performed. Of the two, gallium-67 citrate scan is about 92-100% accurate [1, 11], while a CT scan is even less sensitive than an MRI. WBC scan have lesser utility in vertebral osteomyelitis [1] because of non-specific neutropenic defect [12].
Blood cultures in vertebral osteomyelitis patients play an important role. A positive blood culture can be seen in up to 30-78% of the patients [1]. When positive, it can guide clinician to identify culprit microorganism and choose appropriate antibiotics.
The treatment plan for vertebral osteomyelitis patient should include controlling pain, treating infection and preventing neurologic sequelae. An early identification of the microorganism(s) is utmost important for a definitive antibiotic treatment, though empirical antibiotics should be initiated. Guidelines on vertebral osteomyelitis are not currently available, but a standard course of antibiotics should be for 4 - 6 weeks [13]. The surgical approach may be indicated in patients with abscess formation, instability of the spine, neurologic deficit, severe pain, failed conservative management or there is a need for bone biopsy [1, 14].
Conclusion
Our patient presented with a rare constellation of symptoms of osteomyelitis which led to devastating consequences. Practitioners should consider osteomyelitis in differential diagnosis when patients present with non-specific abdominal pain and exudative pleural effusion. Our case highlights that tagged WBC scans offer low yield in diagnosing vertebral osteomyelitis. MRI is the gold standard for diagnosis.
Acknowledgments
None.
Conflict of Interest
None.
| References | ▴Top |
- Zimmerli W. Clinical practice. Vertebral osteomyelitis. N Engl J Med. 2010;362(11):1022-1029.
doi pubmed - Wiley AM, Trueta J. The vascular anatomy of the spine and its relationship to pyogenic vertebral osteomyelitis. J Bone Joint Surg Br. 1959;41-B:796-809.
pubmed - McHenry MC, Easley KA, Locker GA. Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin Infect Dis. 2002;34(10):1342-1350.
doi pubmed - Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum. 2009;39(1):10-17.
doi pubmed - Priest DH, Peacock JE
Jr . Hematogenous vertebral osteomyelitis due to Staphylococcus aureus in the adult: clinical features and therapeutic outcomes. South Med J. 2005;98(9):854-862.
doi - Sohatee MA, Shields DW. Painless vertebral osteomyelitis: an unusual presentation. BMJ Case Rep. 2013;2013
- Landa C, Giddings S, Reddy P. Chest pain? An unusual presentation of vertebral osteomyelitis. Case Rep Med. 2013;2013:416498.
- Bass SN, Ailani RK, Shekar R, Gerblich AA. Pyogenic vertebral osteomyelitis presenting as exudative pleural effusion: a series of five cases. Chest. 1998;114(2):642-647.
doi pubmed - Noy ML, George S. Unusual presentation of a spinal epidural abscess. BMJ Case Rep. 2012;2012
- Palestro CJ, Love C, Miller TT. Infection and musculoskeletal conditions: Imaging of musculoskeletal infections. Best Pract Res Clin Rheumatol. 2006;20(6):1197-1218.
doi pubmed - Hadjipavlou AG, Cesani-Vazquez F, Villaneuva-Meyer J, Mader JT, Necessary JT, Crow W, Jensen RE,
et al . The effectiveness of gallium citrate Ga 67 radionuclide imaging in vertebral osteomyelitis revisited. Am J Orthop (Belle Mead NJ). 1998;27(3):179-183.
pubmed - Palestro CJ, Torres MA. Radionuclide imaging in orthopedic infections. Semin Nucl Med. 1997;27(4):334-345.
doi - Roblot F, Besnier JM, Juhel L, Vidal C, Ragot S, Bastides F, Le Moal G,
et al . Optimal duration of antibiotic therapy in vertebral osteomyelitis. Semin Arthritis Rheum. 2007;36(5):269-277.
doi pubmed - Chen WH, Jiang LS, Dai LY. Surgical treatment of pyogenic vertebral osteomyelitis with spinal instrumentation. Eur Spine J. 2007;16(9):1307-1316.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


