| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 1, Number 1, August 2010, pages 18-20
Mucinous Tubular and Spindle Cell Carcinoma of the Kidney: Four New Cases
Amel Trabelsia, Soumaya Ben Abdelkrima, d, Olfa Gharbib, Nadia Beiziga, Wafa Jomaaa, Dajla Abbassi Bakirc, Badreddine Srihaa
aDepartment of pathology, Farhat Hached hospital, 4000 Sousse, Tunisia
bDepartment of medical oncology, Farhat Hached hospital, 4000 Sousse, Tunisia
cDepartment of radiology, Farhat Hached hospital, 4000, Sousse, Tunisia
dCorresponding author: Address: Farhat Hached Hospital, 4000 Sousse, Tunisia
Manuscript accepted for publication July 7, 2010
Short title: Spindle Cell Carcinoma of Kidney
doi: https://doi.org/10.4021/jmc113e
| Abstract | ▴Top |
Mucinous tubular and spindle cell carcinoma of the kidney is a rare and a recently described tumor with a favorable prognosis. Herein, we report four new cases. Four cases of mucinous tubular and spindle cell carcinoma of the kidney were diagnosed in our Department of Pathology (Farhat Hached hospital, Sousse, Tunisia). Histological slides and medical records were reviewed for morphologic and clinical data. The histological diagnosis was established according to the WHO classification system. The 2002 TNM system was used for pathologic staging. The median age of the four patients was 50 years, 2 patients presented with a unilateral flank pain and the tumor was asymptomatic in the 2 other cases. Tumors were well circumscribed on imaging exploration. All patients were treated by nephrectomy (radical in 2 cases and partial in 2 cases). Grossly, tumors presented as well-circumscribed solid masses, contained in the renal capsule in all cases. The mean tumor size was 4.5 cm. The histological diagnosis of mucinous tubular and spindle cell carcinoma was performed in all cases according to the WHO classification system. The four cases were pT1N0M0. The mean follow-up was 31 months and during this period, none of the patients developed recurrence or metastases. Mucinous tubular and spindle cell carcinoma of the kidney is a rare and a distinctive renal tumor with a relatively indolent behavior.
Keywords: Kidney; Mucinous tubular and spindle cell carcinoma; Pathology
| Introduction | ▴Top |
Mucinous tubular and spindle cell carcinoma (MTSCC) is a rare variant of renal cell carcinoma, which has recently been described in case reports or small series [1]. We report four new cases and describe clinical and pathological features of this entity.
| Cases Report | ▴Top |
Four patients with MTSCC of the kidney were diagnosed between 2006 and 2010 in Pathology Department, Farhat Hached hospital, Sousse, Tunisia. Data about clinical and radiological features as well as treatment modalities were extracted from medical records. Histological slides were reviewed and diagnosis of renal MTSCC was based on the criteria established by the WHO classification system [2, 3]. The 2002 pTNM (for pathologic Tumor Lymph Node and Metastasis) classification system was used for pathologic staging [4].
The mean age at diagnosis was 50 years (range: 43 - 56 years). All patients were female without history of genitourinary or renal malignancy. Two patients presented with unilateral flank pain for 2 and 12 months duration. In 2 cases, tumor was asymptomatic and detected on ultrasonography. Imaging exploration (ultrasonography and computed tomography scan) showed a well-circumscribed renal mass (Fig. 1) in all the cases (3 left-sided and 1 right-sided mass).
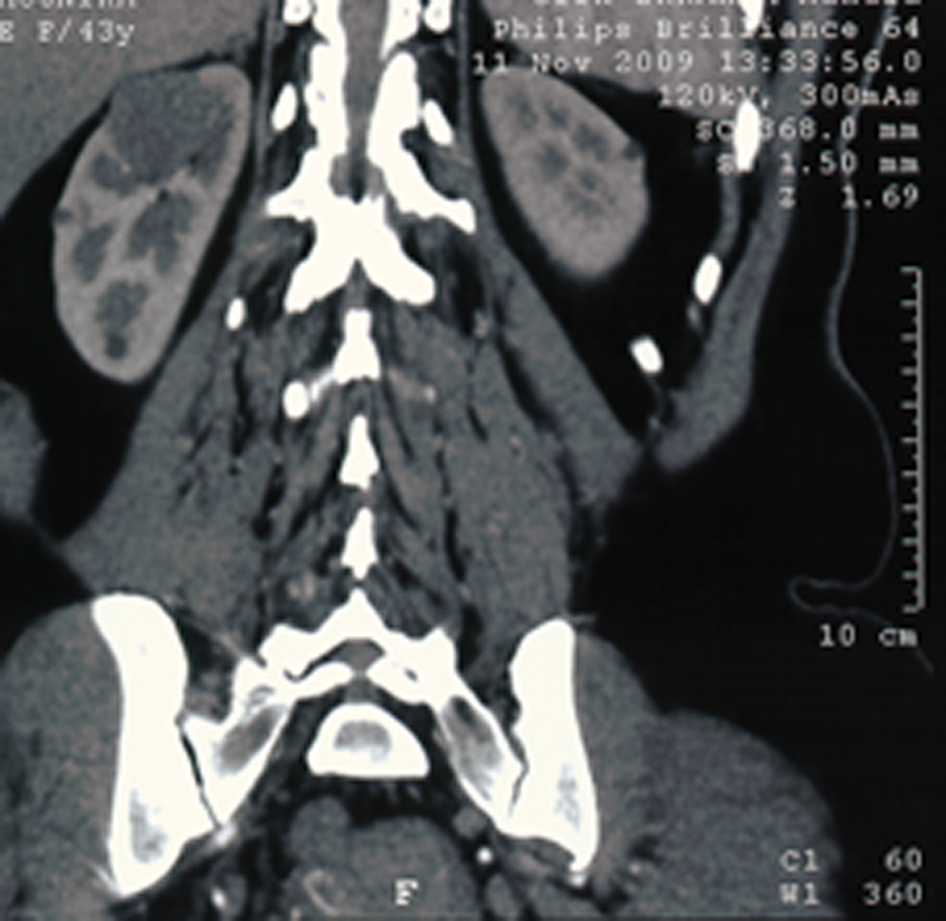 Click for large image | Figure 1. Computed tomography scan: right renal well-defined mass. |
Radical nephrectomy was performed in two cases and partial nephrectomy in the two remaining cases. Macroscopically, tumors presented as solid grayish white well-demarcated unencapsulated nodules with foci of hemorrhage in 2 cases. There was no invasion in the surrounding perinephric fat or in the renal vein in the hilum. The mean tumor size was 4.5 cm (range: 2.5 - 7 cm). The adjacent renal parenchyma was grossly unremarkable. The histological diagnosis of MTSCC was based on the criteria established by the WHO classification system. The microscopic analysis (Figs. 2-4) showed epithelial elements separated by short fascicles of regular spindle cells. Epithelial elements arranged in microtubules and long cords in all cases. These tubules and cords were lined by cuboidal cells with no nuclear atypia. Mucinous change was evident in all cases particularly after alcian blue staining. No mitoses neither areas of necrosis were found. Immunohistochemical stains showed immunoreactivity for cytokeratin 7 and epithelial membrane antigen (EMA). Adjuvant therapy was not performed. No recurrence or metastases have been detected during the follow-up period (mean: 31 months, range: 8 - 72 months). Table Isummarizes the clinical and pathological features and follow-up information of the four cases.
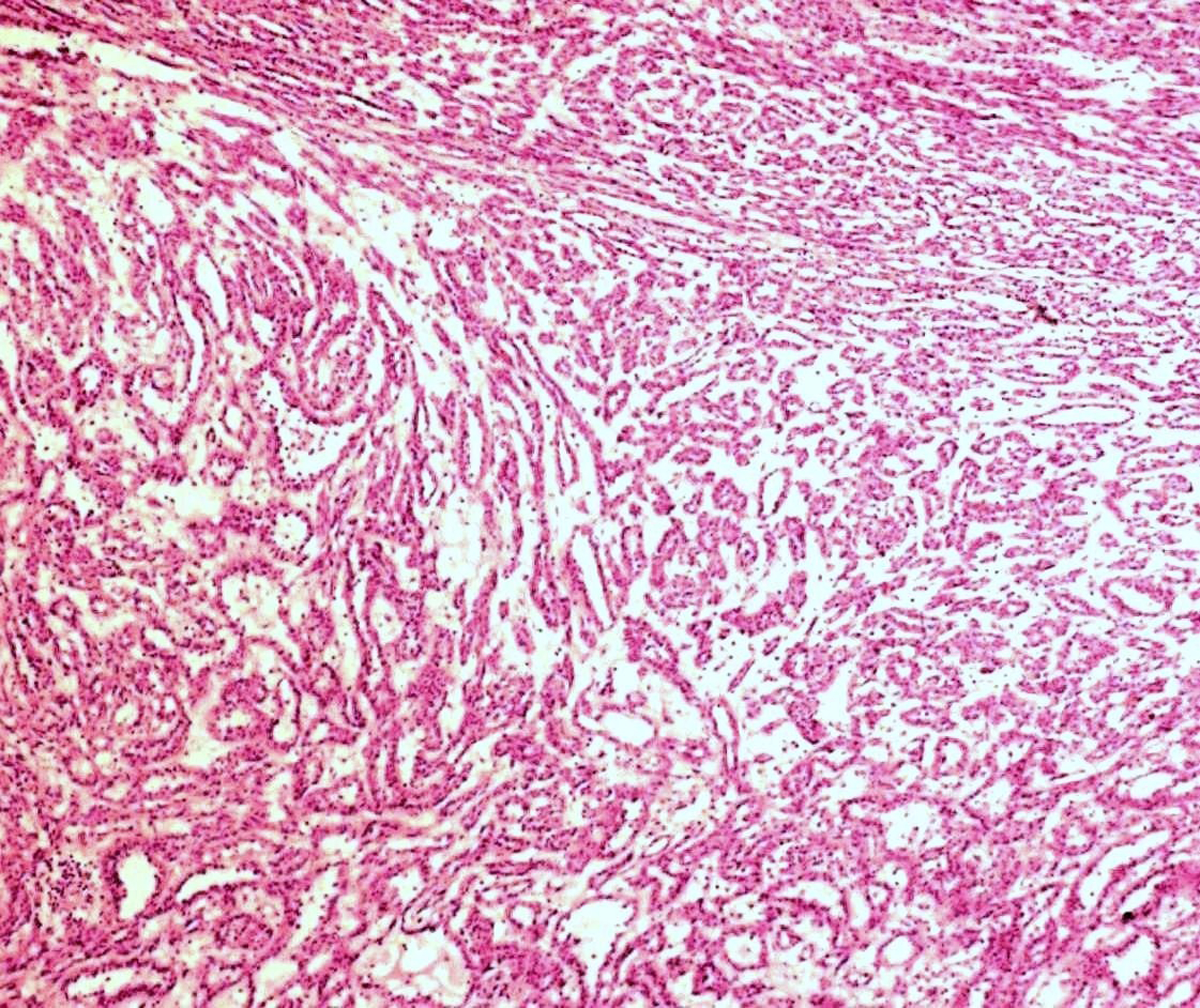 Click for large image | Figure 2. Microtubules and cords of cells making abrupt transition to spindle cell morphology (HE x40). |
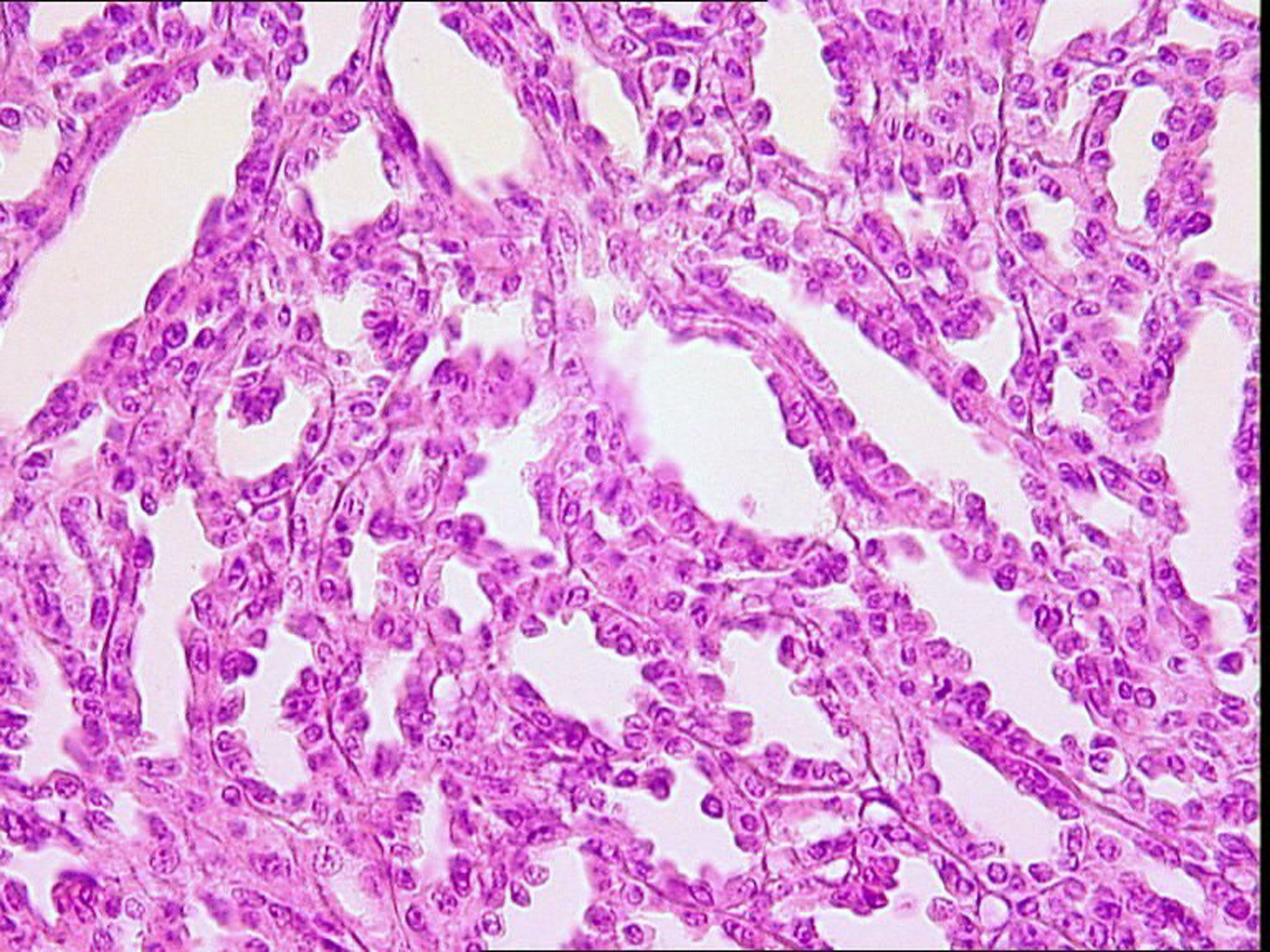 Click for large image | Figure 3. Cuboidal cells lacking atypia (HE x400). |
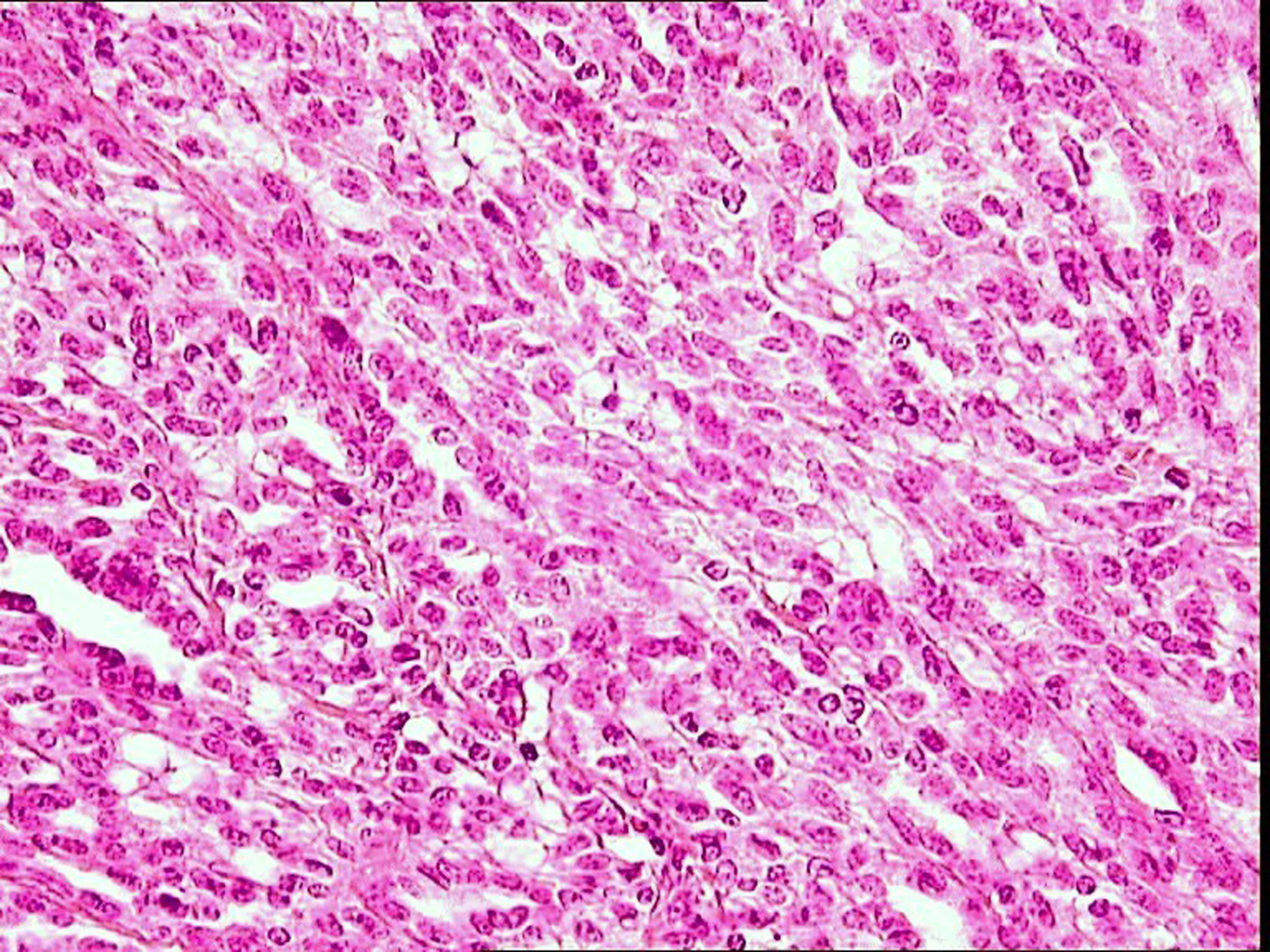 Click for large image | Figure 4. Spindle cells lacking atypia (He x400). |
 Click to view | Table 1. Patients’ Characteristics |
| Discussion | ▴Top |
MTSCC of the kidney is a rare and a recently described tumor. Until now, less than 60 cases have been reported [1]. It occurs in adults, predominantly in women and is typically detected as an asymptomatic renal mass [5]. Two of our patients had an asymptomatic tumor. On ultrasonography and computed tomography, the tumor is well-circumscribed and contained in the renal capsule. Grossly, MTSCC is usually a well-circumscribed tumor which presents as a single firm, homogenous, gray to brown mass at cut surface [6]. All our cases had a well-circumscribed growth on computed tomography scan and on macroscopic examination. The histological diagnosis of MTSCC is based on the criteria established by the WHO classification system. The tumor is composed of cuboidal cells arranged in microtubules and long cords making abrupt transition to spindle morphology. These structures are arrayed in a mucinous or a myxoid stroma that reacts strongly with alcian blue [5]. Nuclear atypia and mitoses are rare in both cuboïdal and spindle cells. Because of the presence of compact tubular architecture, focal papillations and mucin production, the MTSCC has some morphological similarities with papillary renal cell carcinoma particularly type 1 [1]. This tumor can also be confused with the papillary renal cell carcinoma with sarcomatoid change, but in the MTSCC, spindle cells are arranged in parallel bundles with eosinophilic cytoplasm and low grade nuclei [7]. Immunohistochemistry is not helpful in discriminating between papillary renal cell carcinoma and MTSCC and the morphological interpretation is still important in the distinction between these tumors. MTSCC of the kidney must also be distinguished from metanephric adenoma which shows cells having less cytoplasm and appears as a cellular blue tumor on microscopy; but the latter is usually negative for EMA and cytokeratin 7. The renal MTSCC has a relatively indolent behavior and the prognosis is favorable [8]. In our cases, none of the patients developed recurrence or metastases with 31 months' mean follow-up. In summary, MTSCC of the kidney is a rare and distinctive subtype of renal cell carcinoma that must be differentiated from papillary renal cell carcinoma, especially with sarcomatoid change, which has a much poorer prognosis. Recognition of this histological variant is important because it can be mistaken for other neoplasm potentially resulting in suboptimal therapy.
Conflict of Interest
The authors declare no conflict of interests.
| References | ▴Top |
- Geramizadeh B, Salehipour M, Moradi A. Mucinous tubular and spindle cell carcinoma of kidney: a rare case report and review of the literature. Indian J Pathol Microbiol 2009;52(4):514-516.
pubmed doi - Lopez-Beltran A, Scarpelli M, Montironi R, Kirkali Z. 2004 WHO classification of the renal tumors of the adults. Eur Urol 2006;49(5):798-805.
pubmed doi - Srigley JR. Mucinous tubular and tubular and spindle cell carcinoma. WHO classification of tumors In: Eble JN, Sauter G, Epstein JL, Sesterhenn IA (eds). Tumors of the genitourinary and male genital organs. IARC, Washington DC, USA.
- Greene FL, Page DL, Flemming ID, et al editors. AJCC staging manual, 6th ed. New York: Springer - Verlag, 2002.
- Eble JN. Mucinous tubular and spindle cell carcinoma and post-neuroblastoma carcinoma: newly recognised entities in the renal cell carcinoma family. Pathology 2003;35(6):499-504.
pubmed doi - Paner GP, Srigley JR, Radhakrishnan A, Cohen C, Skinnider BF, Tickoo SK, Young AN, et al. Immunohistochemical analysis of mucinous tubular and spindle cell carcinoma and papillary renal cell carcinoma of the kidney: significant immunophenotypic overlap warrants diagnostic caution. Am J Surg Pathol 2006;30(1):13-19.
pubmed doi - Fleming S. Recently recognized epithelial tumours of the kidney. Curr Diagn Pathol 2005;11:162-169.
- Kumari N, Chhabra P, Dewan U, Jain M. Renal mucinous tubular and spindle cell carcinoma. Indian J Pathol Microbiol 2009;52(3):400-402.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


