| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 1, Number 1, August 2010, pages 37-38
Development of Takayasu Arteritis Despite Existing Treatment of Etanercept and Questionable Paradoxical Effect: Case Report and Review of Literature
Tarek Kteleha, e, Tamim Khromachoub, Sarab Alfatac, Anas Mouchlid
aDepartment of Rheumatology, University of North Dakota, USA
bDepartment of Internal Medicine, Mercer University, USA
cDepartment of Family Medicine, University of North Dakota/MeritCare Health System, USA
dDepartment of Internal Medicine, University of North Dakota/ MeritCare Health System, USA
eCorresponding author: Tarek Kteleh
Manuscript accepted for publication July 14, 2010
Short title: Development of Takayasu Arteritis
doi: https://doi.org/10.4021/jmc2w
| Abstract | ▴Top |
Although glucocorticoids are the standard treatment in patients with Takayasu arteritis, significant data suggest that etanercept, as well as other anti-tumor necrosis factor alpha (anti-TNF) agents, are effective in refractory cases. We report what we believe to be the first case in literature in which a patient who was on active treatment of etanercept for psoriatic arthritis, developed Takayasu arteritis. Although this case report is not intended to conflict with the previous data that support the beneficial role of ant-TNF agents in the treatment of Takayasu arteritis, it does show that a certain patient might still develop Takayasu arteritis despite being on active treatment of etanercept. We also cannot conclude from this case that Takayasu arteritis was triggered by etanercept. However, such a possibility remains in question.
Keywords: Refractory Takayasu arteritis; Etanercept; Paradoxical
| Case Report | ▴Top |
We present a 44-year-old woman who had unexplained visual changes, lightheadedness, and bilateral upper extremity weakness for 6 months in addition to an episode of presyncope. She also reported diaphoresis and fever. The visual changes are described as ‘very bright, foggy, and blurred vision in both eyes’. She also mentioned improvement of her vision when she lays flat with resolution of her ‘foggy’ vision. Her past medical history is significant for anemia, diabetes mellitus, psoriasis and psoriatic arthritis. Her family history is significant for psoriasis.
She was receiving a treatment of etanercept 50 mg subcutaneously on a weekly basis over the last two years for psoriatic arthritis. She was eventually admitted to the hospital for further work up of her symptoms. On admission, physical exam showed normal vital signs and was unremarkable except for decreased visual acuity and bilateral carotid bruits.
Her laboratory tests showed ESR 47 mL/hr, CRP 1.06 mg/dL, and negative ANA and ANCA tests. CT scan of the brain without contrast did not show any evidence of neoplasm, ischemic change or hemorrhage. MRI of the brain showed nonspecific white matter changes. The ophthalmologist’s report revealed mild diffuse ischemic edema in the macula. Carotid ultrasound was consistent with high-grade stenosis of the left internal carotid artery (ICA), and probable external carotid occlusion on the right. An angiogram of the aortic arch and upper arteries and cerebral angiogram were done and showed diffuse long segment near-occlusive stenosis involving the common carotid arteries bilaterally (Fig. 1), left and proximal right subclavian arteries (Fig. 2) and limited flow to the left anterior cerebellar circulation suggestive of Takayasu arteritis. The patient had angioplasty of left and right common carotid artery with marked improved intracranial flow.
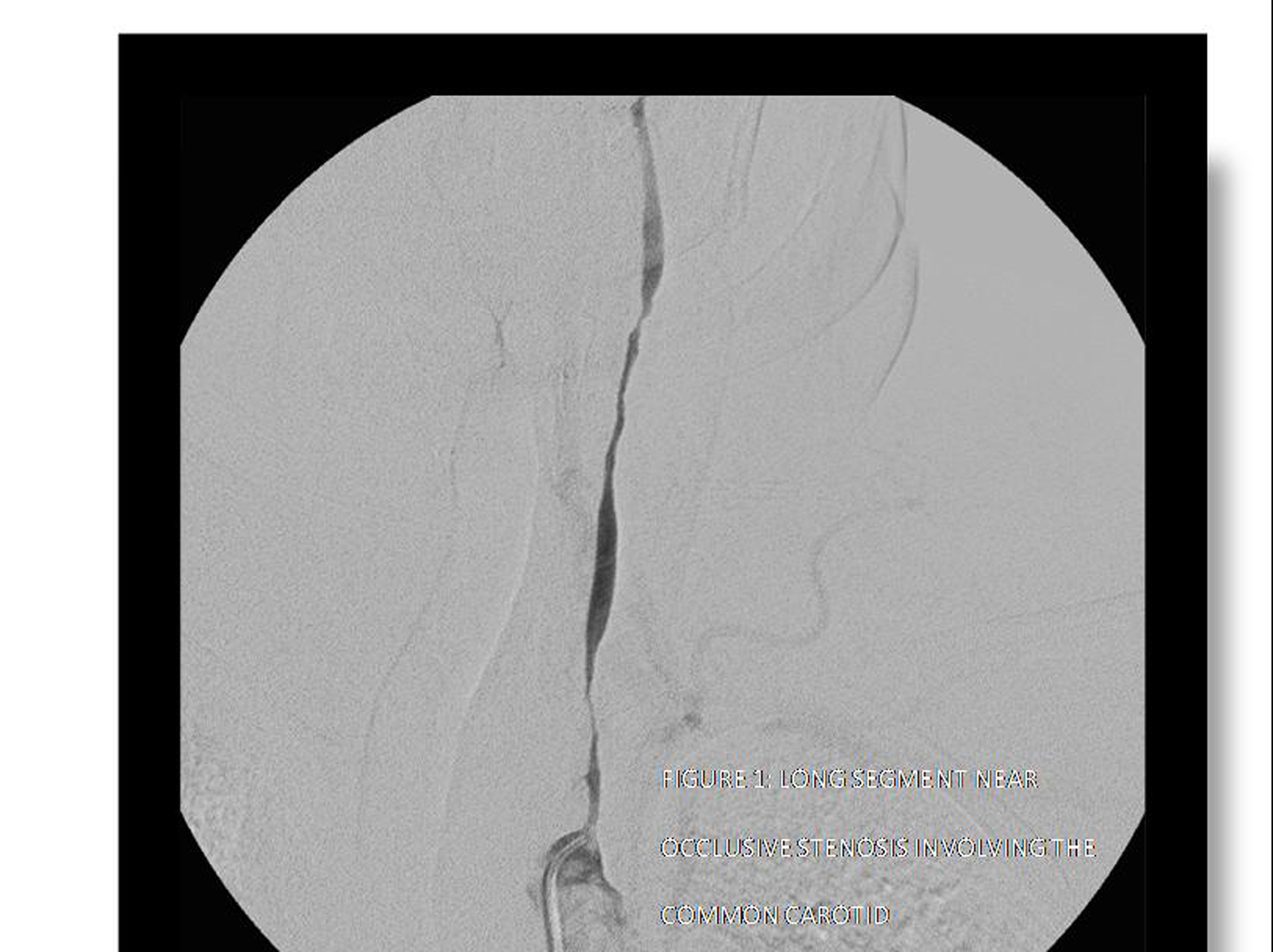 Click for large image | Figure 1. Long segment near occlusive stenosis involving the common carotid. |
 Click for large image | Figure 2. Proximal right subclavian occlusion. |
The patient was seen by a rheumatologist who agreed with the diagnosis of Takayasu arteritis given the visual symptoms, elevated sedimentation rate and the arterial stenosis of the major aortic artery branches (carotid and subclavian) on the angiogram.
The patient was started on Plavix 75 mg and prednisone 1mg/kg after 3 days of intravenous 1000 mg.
In a follow-up visit 3 weeks later, her labs showed sedimentation rate of 12 mL/hr and CRP 0.16 mg/dL. Clinically the patient has had improvement of her neurological symptoms but continues to have some foggy vision. She was referred again to interventional radiology for further angioplasties in order to improve her vision. She continued to be on etanercept for psoriatic arthritis but there was a discussion about discontinuing the drug as it was not clear if it had a relation in triggering the Takayasu arteritis in this case.
| Discussion | ▴Top |
Takayasu arteritis (TA) is a chronic disease characterized by inflammation of large vessels, primarily the aorta and its primary branches. Individuals of any race, gender, or age may be affected by TA, but it is most common in young Asian females. Glucocorticoids are the standard treatment in patients with Takayasu arteritis [1]. Significant data supported by several articles suggest that etanercept, as well as other anti-tumor necrosis factor alpha (anti-TNF) agents, are effective treatment for refractory cases of Takayasu arteritis [2-4]. Despite such data, we report what we believe to be the first case in literature to show that Takayasu arteritis can, indeed, develop in a patient who is actively receiving etanercept. An important question remains to be answered: could the etanercept in this case have played a role in triggering Takayasu arteritis in the patient? The answer for such a link, needs further case reports to be answered clearly. Such paradoxical relation has been reported in literature. For example, we do know for a fact that etanercept is an effective, FDA approved drug for psoriasis treatment [5, 6], yet, it has been reported to trigger psoriasis in many patients [7].
| References | ▴Top |
- Kerr GS. Takayasu's arteritis. Rheum Dis Clin North Am 1995;21(4):1041-1058.
pubmed - Hoffman GS, Merkel PA, Brasington RD, Lenschow DJ, Liang P. Anti-tumor necrosis factor therapy in patients with difficult to treat Takayasu arteritis. Arthritis Rheum 2004;50(7):2296-2304.
pubmed doi - Della Rossa A, Tavoni A, Merlini G, Baldini C, Sebastiani M, Lombardi M, Neglia D, et al. Two Takayasu arteritis patients successfully treated with infliximab: a potential disease-modifying agent? Rheumatology (Oxford) 2005;44(8):1074-1075.
pubmed doi - Molloy ES, Langford CA, Clark TM, Gota CE, Hoffman GS. Anti-tumour necrosis factor therapy in patients with refractory Takayasu arteritis: long-term follow-up. Ann Rheum Dis 2008;67(11):1567-1569.
pubmed doi - Iyer S, Yamauchi P, Lowe NJ. Etanercept for severe psoriasis and psoriatic arthritis: observations on combination therapy. Br J Dermatol 2002;146(1):118-121.
pubmed doi - Leonardi CL, Powers JL, Matheson RT, Goffe BS, Zitnik R, Wang A, Gottlieb AB. Etanercept as monotherapy in patients with psoriasis. N Engl J Med 2003;349(21):2014-2022.
pubmed doi - Collamer AN, Guerrero KT, Henning JS, Battafarano DF. Psoriatic skin lesions induced by tumor necrosis factor antagonist therapy: a literature review and potential mechanisms of action. Arthritis Rheum 2008;59(7):996-1001.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


