| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 3, March 2016, pages 81-83
Lactate Dehydrogenase and Ferritin Levels: A Clinical Clue for Early Diagnosis of Disseminated Histoplasmosis in HIV Patients
Fnu Zarlashta, b, Mohamed Ramadana, Munaf Almoadhena, Katherine Lina, Misbahuddin Khajaa, Riyad Basira
aLincoln Hospital and Mental Health Center, Medical Intensive Care Unit, Bronx, NY, USA
bCorresponding Author: Fnu Zarlasht, Lincoln Hospital and Mental Health Center, Medical Intensive Care Unit, 1765 Townsend Avenue, Bronx, NY 10453, USA
Manuscript accepted for publication May 06, 2015
Short title: LDH in Disseminated Histoplasmosis
doi: http://dx.doi.org/10.14740/jmc2173w
| Abstract | ▴Top |
Histoplasmosis is the most common endemic mycosis in AIDS and often mimics other opportunistic infections. Previous studies have indicated a correlation between early biomarkers and histoplasmosis. In our case, we present an AIDS patient presenting with fever and pulmonary symptoms, found to have histoplasmosis along with markedly elevated lactate dehydrogenase (LDH) and ferritin.
Keywords: Histoplasmosis; HIV; Human immunodeficiency syndrome; Lactate dehydrogenase; Ferritin
| Introduction | ▴Top |
Patients with acquired immunodeficiency syndrome are susceptible to many opportunistic infections. Histoplasma capsulatum is the most common endemic mycosis in AIDS and it represents the AIDS defining illness in 50% of affected patients [1-3]. It continues to cause severe morbidity and mortality and unfortunately can mimic many other opportunistic infections. Diagnostic tests often take weeks to yield a result and treatment usually begins with a high clinical suspicion in immunocompromised patients. Pneumocystis pneumonia (PCP), in particular, presents similarly both symptomatically as well as radiographically to histoplasmosis. Any marker that can lead to early differentiation and appropriate treatment will be of great use to physicians. Here we report a case of an AIDS patient who presented with fever and pulmonary symptoms, who was found to have an initial lactate dehydrogenase (LDH) level of 1,100 IU/L, a ferritin level of 5,203 IU/L and a positive sputum smear for histoplasmosis.
| Case Report | ▴Top |
Patient is a 28-year-old male, HIV positive not on HAART, who initially presented with altered mental status, cough productive of brownish sputum and decreased oral intake.
A month prior, patient presented to the ED with complaints of headache, generalized body aches and nausea and vomiting for 3 weeks associated with fevers and chills. Lumbar puncture (LP) was negative for infection. CT of head showed evidence of sinusitis and patient was discharged home on augmentin. As per family, since discharge, patient continued to have poor appetite and progressively worsened in 24 h, becoming confused, unable to recognize family members and refusing to talk or leave the bed. For the past several weeks, he continued to experience fevers and had a cough productive of sputum.
In the ED, patient’s vital signs were as follows: temperature 102 °F, HR 128 bpm, BP 105/63 mm Hg, and RR 24. He was non-verbal, agitated and in distress. He became severely tachypneic, hypotensive, unable to follow commands, with no evidence of focal neurological deficits. He was admitted to the ICU where an endotracheal tube was placed to protect his airways and a central line was placed to start him on vasopressors.
Initial labs showed LDH 1,175 IU/L and CD4 count 4/mm3. LP performed did not show any acute infection. Chest X-ray showed diffuse interstitial infiltrates. CT of brain revealed two foci of edema in the left parietal lobe not seen on previous CT the month prior. During the hospital course, patient became progressively hypotensive. He was started on empiric treatment for PCP, community acquired pneumonia and toxoplasmosis pending lab workup.
A bronchoscopy was performed and sputum samples were sent for analysis. Initial report came back negative for PCP and positive for candida (normal colonizer) and histoplasmosis (Fig. 1). Treatment for PCP was discontinued and patient was started on amphotericin to cover for histoplasmosis. Urine histoplasmosis antigen was sent to confirm the diagnosis. Patient completed the treatment with anti-fungal therapy and improved very well (Fig. 2). Now he is back to baseline.
 Click for large image | Figure 1. Microscopic slide of histoplasmosis: sputum samples were positive for candida (normal colonizer) and histoplasmosis. |
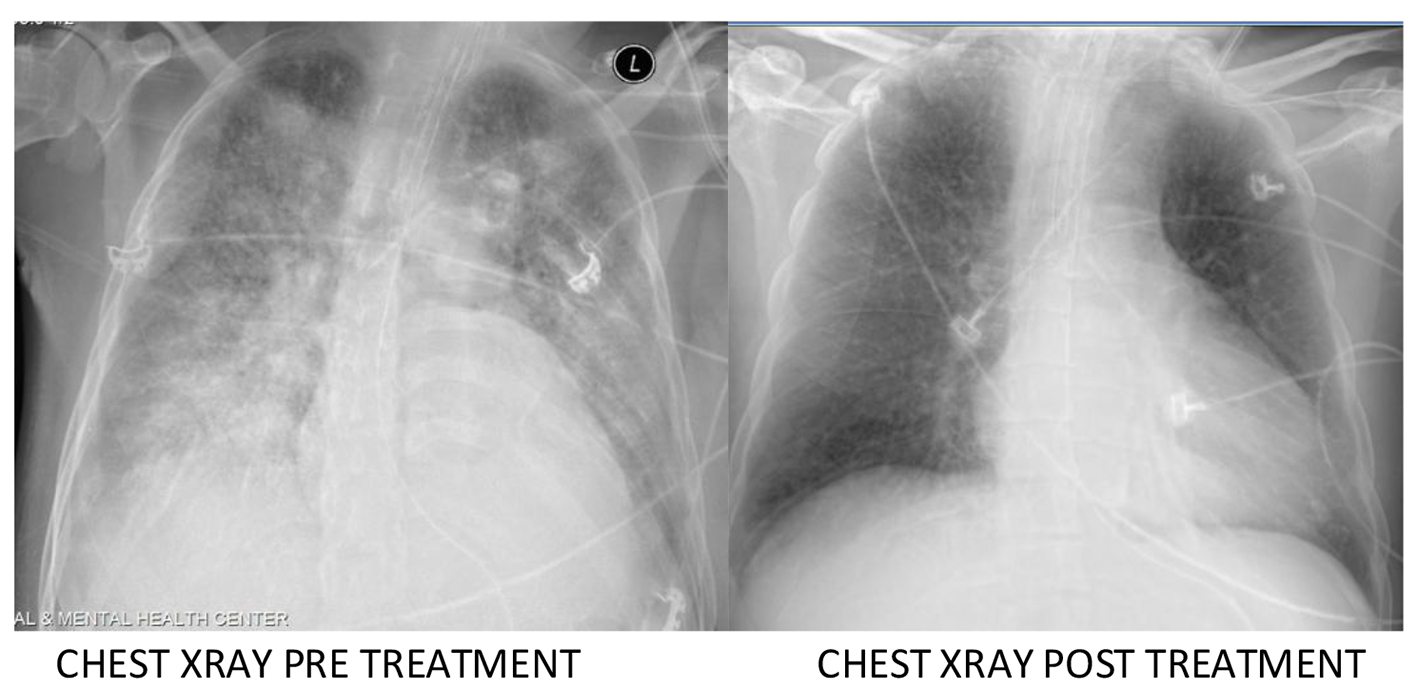 Click for large image | Figure 2. Chest X-ray for pre-treatment and post-treatment. |
| Discussion | ▴Top |
Histoplasmosis is a rare disease which is usually seen in immune-compromised patients or in people who are prone to it due to their professions.
There are several presentations of histoplasmosis like pulmonary involvement, pericarditis, myositis, dermatologic involvement, and CNS diseases, and histoplasmosis can be a challenging disease if not treated properly.
There are several available tests used to aid in the diagnosis of histoplasmosis: culture, serology, antigen testing and direct microscopy [4]. The simplest and most rapid test is direct visualization of the organism on microscopy. In our patient, initial BAL sputum stain was read as positive for candida and later corrected to H. capsulatum. As an inexpensive and useful test in endemic resource limited areas, H. capsulatum can often be confused with Candida glabrata, Penicillium marneffei and amastigote forms of Trypanosoma cruzi under direct microscopy [5]. The advantage of this test, while not a sensitive test, is that it provides a cheap and rapid diagnosis when positive.
The gold standard for diagnosing histoplasmosis is culture of blood, respiratory samples or other tissues. Unfortunately, cultures can take up to 4 - 6 weeks and are dependent on disease burden [5]. Antigen detection in serum, urine, CSF and BAL fluid is a sensitive diagnostic marker for histoplasmosis but again generally takes over a week to yield a diagnosis as in our patient [4]. Treatment should not be delayed pending such tests and high clinical suspicion in conjunction with helpful biomarkers can help aid physicians in choosing an early treatment.
Previous cases (Table 1) have discussed markedly elevated LDH and ferritin correlated with clinical and radiographic pictures to point towards a diagnosis of histoplasmosis [6]. A previous case-control study found a cutoff level of 600 IU/L to have a sensitivity and specificity of 50% and 89%, respectively in the diagnosis of histoplasmosis [7]. In our patient, an initial LDH > 600 IU/L could have led us to consider histoplasmosis over PCP prior to confirmatory testing and earlier treatment.
 Click to view | Table 1. Literature Review Showing Relation of LDH With Disseminated Histoplasmosis |
We believe that there is a strong correlation between disseminated histoplasmosis and LDH, and strongly recommend that early anti-fungal therapy after ruling out PCP should be considered.
It should also be noted that elevated LDH has also been associated with many other illnesses that can affect AIDS patients, including but not limited to PCP, bacterial pneumonia, toxoplasmosis, and tuberculosis [8]. When dyspnea is the only presenting symptom, LDH has a greater specificity for PCP and histoplasmosis.
Conclusion
In this report, we emphasize on the importance of LDH and ferritin in diagnosing histoplasmosis earlier, in HIV patients. An early diagnosis helps in preventing shock and decreasing mortality/morbidity.
In summary, histoplasmosis is a very important opportunistic infection in AIDS patients but early diagnosis can often be difficult. Early biomarkers which can be rapidly detected can lead physicians to consider one differential over another, especially when many opportunistic infections can present similarly to histoplasmosis and help in preventing prolonged hospitalization by starting treatments earlier.
| References | ▴Top |
- Hage CA, Wheat LJ, Loyd J, Allen SD, Blue D, Knox KS. Pulmonary histoplasmosis. Semin Respir Crit Care Med. 2008;29(2):151-165.
doi pubmed - Wheat LJ, Chetchotisakd P, Williams B, Connolly P, Shutt K, Hajjeh R. Factors associated with severe manifestations of histoplasmosis in AIDS. Clin Infect Dis. 2000;30(6):877-881.
doi pubmed - Baddley J. Epidemiology and clinical manifestations of histoplasmosis in HIV-infected patients. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA (accessed on December 10, 2014).
- Wheat LJ, C Kauffman. Diagnosis and treatment of pulmonary histoplasmosis. In: UpToDate, Post TW (Ed), UpToDate, Walthma, MA. (accessed on December 9, 2014).
- Couppie P, Aznar C, Carme B, Nacher M. American histoplasmosis in developing countries with a special focus on patients with HIV: diagnosis, treatment, and prognosis. Curr Opin Infect Dis. 2006;19(5):443-449.
doi pubmed - Diaz-Fuentes G, Shin C, Menon L. Disseminated histoplasmosis in patients with the human immunodeficiency virus (HIV) in a nonendemic area in New York. The Internet Journal of Infectious Diseases. 2005;5:2.
- Adeel A. Butt, MD, Stephanie Michaels et al. Serum ldh level as a clue to the diagnosis of histoplasmosis. AIDS Read. 2002;12:7.
- Quist J, Hill AR. Serum lactate dehydrogenase (LDH) in Pneumocystis carinii pneumonia, tuberculosis, and bacterial pneumonia. Chest. 1995;108(2):415-418.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


