| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 10, Number 4, April 2019, pages 97-100
Pelvic Peritonitis Caused by Campylobacter rectus Infection: Case Report and Literature Review
Anaelle Veyrinea, Julie Sturquea, Aude-Sophie Zlowodskia, Tom Sourimanta, Maina Le Gala, Frederic Denisa, b, c
aOdontology Department, University Hospital, Tours, France
bEA 75-05 Education, Ethique, Sante, Universite Francois-Rabelais Tours, Faculte de Medecine, Tours, France
cCorresponding Author: Frederic Denis, Odontology Department, University Hospital, Chambray les Tours 37170, France
Manuscript submitted February 27, 2019, accepted March 11, 2019
Short title: Pelvic Peritonitis and Campylobacter rectus
doi: https://doi.org/10.14740/jmc3275
| Abstract | ▴Top |
Campylobacter rectus (CR) is an exclusively oral, Gram-negative anaerobe and mobile bacterium that shows a wide range of virulence factors. A 41-year-old woman came to the emergency department because she felt intense radiating pain in the whole abdomen. A molecular biology analysis rapidly revealed a tubo-ovarian abscess caused by CR. A focal infection of periodontal origin was the most probable; nevertheless the possibility of a cross-contamination from her husband suffering from an active periodontal disease was the subject of discussions. The incidence of focal infections due to CR is probably underestimated. The introduction of molecular biology in common practice should reveal a larger number of CR focal infection cases but more generally speaking of bacteria from the oral cavity.
Keywords: Infection; Extra-oral; Campylobacter rectus; Wolinella recta; Mass spectrometry
| Introduction | ▴Top |
Campylobacter rectus (CR) is an exclusively oral, Gram-negative anaerobe and mobile bacterium that shows a wide range of virulence factors, in particular the flagellum, the proteins in the superficial layer, the repeats-in-toxin (RTX) toxins, the GroEL-like proteins and the lipopolysaccharide [1]. CR is involved as direct or indirect pathogen in periodontal diseases. CR can also be found in the necrotic radicular root canals [2]. CR was isolated in cases of appendicitis for patients who suffered from Barett’s esophagus and extra-oral abscesses [3].
We would report the case of a pelvic peritonitis caused by CR whose origin shall be discussed a posteriori.
| Case Report | ▴Top |
A 41-year-old woman of Caucasian origin came to the emergency department because she had been feeling intense pelvic pain for 10 days that radiated into the whole abdomen accompanied by diarrhea. The medical history is ligation-transection of the Fallopian tubes received 3 months earlier and asthma treated with salbutamol by inhalation.
The clinical examination reveals a fever of 39.5 °C. The abdomen is tense, taut and painful on palpation. The uterus palpation is painful too. The biological analyses confirm the sepsis: leucocytosis (31.4 g/L) with predominant polynuclear neutrophils (85.5%), monocytes (2.36 g/L) and an increased C-reactive protein (414 mg/L).
The pelvic ultrasound shows a complex adnexal mass on the left ovary. A control computed tomography (CT) scan reveals a left tubo-ovarian abscess together with pelvic peritonitis (Fig. 1).
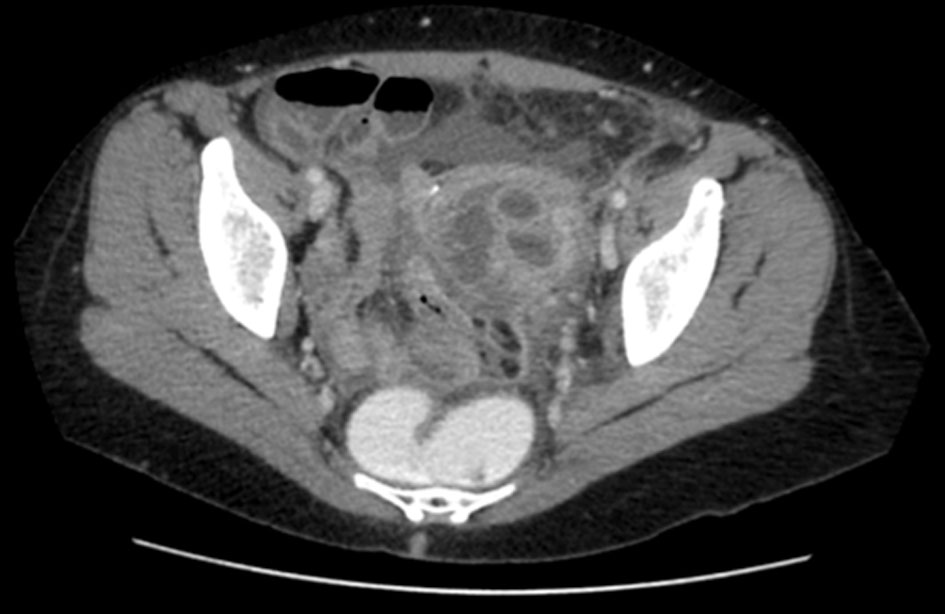 Click for large image | Figure 1. Abdominal CT scan showing a left tubo-ovarian abscess. |
Following her admission to the emergency department the patient underwent surgery with drainage of the tubo-ovarian abscess together with a left partial salpingectomy and then she received a medical treatment with empiric broad-spectrum antibiotics (association of rocephin, metrodinazole, doxycycline and gentamicin) administrated intravenously during 48 h. The mass spectrometry of matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) identified a CR infection and the patient was administrated a targeted antibiotic treatment of intramuscular rocephin (1 g) during 15 days associated with metronidazole per os (1,500 mg) during 21 days.
Following recovery the patient was sent for an odontological assessment in order to check her bucco-dental health and to identify a posteriori the portal of entry of the pathogen. The clinical examination showed a good bucco-dental condition in spite of a generalized stabilized light periodontal chronic disease. The periodontal probing revealed 3 to 4 mm deep pockets with no associated gingival inflammation or bleeding. The radiological examination (Fig. 2) revealed a thickening of the ligaments on two teeth with no symptomatology of an inflammatory peri-radicular lesion of endodontic origin, characterized by apical pain or radiolucent abscess. A periodontal maintenance was undertaken to control this periodontal disease.
 Click for large image | Figure 2. Dental panoramic radiography. |
| Discussion | ▴Top |
As a whole, 15 cases of extra-oral infections with CR were reported in published clinical data, affecting different tissues (Table 1) [4-16]. The patient’s recovery mainly depends upon his general health condition, the site affected by the infection but also a quick identification of CR and the provision of a proper and efficient treatment.
 Click to view | Table 1. Summary of Reported Campylobacter rectus Infections in Data Base |
The identified risk factors associated with an extra-oral infection with CR are a lack of oral hygiene, a periodontal disease or a dental abscess [4-10]. They can be aggravated by immunosuppression induced by health reasons that could potentiate conditions such as diabetes, chronic alcoholism, a cancerous pathology, a kidney failure or neutropenia [4, 6, 8, 10-12]. Finally, an invasive procedure performed close to a site infected with CR contributes to hematogenous spread. Cases of maxillary and cerebral infections were reported following dental avulsions [9, 13], the case of a breast abscess following nipple piercing [11], and a ligation-transection of the Fallopian tubes followed by a tubo-ovarian abscess in the case we are dealing with. Three cases do not have identified risk factors [14-16].
In this case a focal infection of periodontal origin is the most probable even if we cannot formally prove it. Indeed, the targeted antibiotic treatment significantly reduced the bacterial load of this pathogen and had the bacterial analysis of the periodontal pockets of the host at a distance from the infection unnecessary.
In this context, we wanted to check the possibility of a cross-contamination from the patient’s husband. Indeed, the latter’s clinical examination revealed an active periodontal disease with pockets as deep as 5 mm at some sites and with bleeding during associated probing. The bacteria collections into the periodontal pockets were analyzed by mass spectrometry of MALDI-TOF; however the presence of CR was not found.
Even if the hypothesis of a contamination of periodontal origin is the most probable, the concept of a focal infection remains disputable since it is difficult to absolutely prove that an extra-buccal infection has been caused by bacteria from the oral cavity. Animal experimentation and clinical studies put forward several physiopathological mechanisms: bacteremia, intervention of toxins, immunologic mechanisms and/or swallowing of dental plaque [4, 17]. However, it remains difficult to isolate at the same time the same bacteria in the oral cavity and in the infected site with a positive biological analysis.
Conclusions
The incidence of focal infections with CR is probably underestimated because investigations are only conducted occasionally, due to the culture conditions and the cost. The introduction of molecular biology in common practice should reveal a larger number of CR focal infection cases but more generally speaking of bacteria in the oral cavity.
Acknowledgments
The authors thank Micheneau Christelle for his help with English language correction.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Patient agreed with publication of this case report.
Author Contributions
All the authors revised the manuscript, and approved the final content of the manuscript.
| References | ▴Top |
- LaGier MJ, Threadgill DS. Identification of novel genes in the oral pathogen Campylobacter rectus. Oral Microbiol Immunol. 2008;23(5):406-412.
doi pubmed - Ihara H, Miura T, Kato T, Ishihara K, Nakagawa T, Yamada S, Okuda K. Detection of Campylobacter rectus in periodontitis sites by monoclonal antibodies. J Periodontal Res. 2003;38(1):64-72.
doi pubmed - Debruyne L, Gevers D, Vandamme P. Taxonomy of the family Campylobacteraceae. Campylobacter. 2008;3-25.
doi - Spiegel CA, Telford G. Isolation of Wolinella recta and Actinomyces viscosus from an actinomycotic chest wall mass. J Clin Microbiol. 1984;20(6):1187-1189.
pubmed - Harvey P, Bayardelle P, Belanger R, Fortin L. Sacroiliitis and septicemia caused by Campylobacter rectus and Actinomyces odontolyticus. Can J Infect Dis. 1994;5(3):133-136.
doi pubmed - Mahlen SD, Clarridge JE, 3rd. Oral abscess caused by Campylobacter rectus: case report and literature review. J Clin Microbiol. 2009;47(3):848-851.
doi pubmed - Lam JY, Wu AK, Ngai DC, Teng JL, Wong ES, Lau SK, Lee RA, et al. Three cases of severe invasive infections caused by Campylobacter rectus and first report of fatal C. rectus infection. J Clin Microbiol. 2011;49(4):1687-1691.
doi pubmed - Ogata T, Urata T, Nemoto D, Hitomi S. Thoracic empyema caused by Campylobacter rectus. J Infect Chemother. 2017;23(3):185-188.
doi pubmed - Martiny D, Dauby N, Konopnicki D, Kampouridis S, Jissendi Tchofo P, Horoi M, Vlaes L, et al. MALDI-TOF MS contribution to the diagnosis of Campylobacter rectus multiple skull base and brain abscesses. New Microbes New Infect. 2017;19:83-86.
doi pubmed - Noel A, Verroken A, Belkhir L, Rodriguez-Villalobos H. Fatal thoracic empyema involving Campylobacter rectus: A case report. Anaerobe. 2018;49:95-98.
doi pubmed - Han XY, Tarrand JJ, Rice DC. Oral Campylobacter species involved in extraoral abscess: a report of three cases. J Clin Microbiol. 2005;43(5):2513-2515.
doi pubmed - Walter HL, Perloff S, Jungkind D, Measley R. A campylobacter rectus subdural empyema. lnfect Dis Clin Pract. 2008;16:332-334.
doi - Leo QJ, Bolger DT, Jr. Septic cavernous sinus thrombosis due to Campylobacter rectus infection. BMJ Case Rep. 2014;2014.
- Marrie TJ, Kerr E. Brain abscess due to Wolinella recta and Streptococcus intermedius. Can J Infect Dis. 1990;1(1):31-34.
doi - de Vries JJ, Arents NL, Manson WL. Campylobacter species isolated from extra-oro-intestinal abscesses: a report of four cases and literature review. Eur J Clin Microbiol Infect Dis. 2008;27(11):1119-1123.
doi pubmed - Kakuta R, Hidaka H, Yano H, Okamoto M, Ozawa D, Endo S, Kaku M, et al. First report of severe acute otitis media caused by Campylobacter rectus and review of the literature. J Infect Chemother. 2016;22(12):800-803.
doi pubmed - Gendron R, Grenier D, Maheu-Robert L. The oral cavity as a reservoir of bacterial pathogens for focal infections. Microbes Infect. 2000;2(8):897-906.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


