| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 11, Number 7, July 2020, pages 201-203
Pigmented Villonodular Synovitis Around the Elbow Joint That Required Upper Arm Amputation
Yuichi Onoa, c, Naohisa Miyakoshia, Hiroyuki Tsuchiea, Hiroyuki Nagasawaa, Hiroshi Nanjob, Yoichi Shimadaa
aDepartment of Orthopedic Surgery, Akita University Graduate School of Medicine, 1-1-1 Hondo, Akita 010-8543, Japan
bDivision of Clinical Pathology, Akita University Hospital, 44-2 Hasunuma Hiroomote, Akita 010-8543, Japan
cCorresponding Author: Yuichi Ono, Department of Orthopedic Surgery, Akita University Graduate School of Medicine, 1-1-1 Hondo, Akita 010-8543, Japan
Manuscript submitted May 22, 2020, accepted June 12, 2020, published online June 29, 2020
Short title: PVNS Around the Elbow
doi: https://doi.org/10.14740/jmc3503
| Abstract | ▴Top |
Pigmented villonodular synovitis (PVNS) is a relatively rare benign proliferative disorder of the synovium, and it commonly occurs in the knee joint. A unique case of huge PVNS originating around the elbow joint that required upper arm amputation is reported. A 74-year-old woman had a 5-month history of right elbow pain and noticed a mass measuring 8 × 5 cm on the olecranon side. She had a past history of undergoing tumor resection and flap surgery 9 years earlier, diagnosed as a giant cell tumor involving the right elbow region. She had chronic renal failure, with a shunt on the right forearm. On magnetic resonance imaging, the tumor around the elbow joint showed low signal intensity on T1-weighted images and low to high intensity on T2-weighted images. It was thought that it was difficult to preserve the limb because of the size of the tumor and the shunt blood vessel. Therefore, upper arm amputation was performed. The histological diagnosis was PVNS. There was no recurrence of PVNS postoperatively. In the treatment of PVNS, initial surgery with complete resection of the synovial membrane and careful postoperative follow-up are considered important.
Keywords: Pigmented villonodular synovitis; Upper arm amputation; Tumor of soft tissue
| Introduction | ▴Top |
Pigmented villonodular synovitis (PVNS) is a relatively rare benign proliferating disorder of the synovium, and it commonly occurs in the joints, with the knee joint being involved most frequently, followed by the hip, ankle, and shoulder joints [1]. Elbow joint involvement is uncommon in PVNS [2]. A unique case of a huge PVNS originating around the elbow joint that required upper arm amputation is presented, along with a review of the literature.
| Case Report | ▴Top |
A 74-year-old woman presented at our outpatient clinic due to slight pain of the right elbow persisting for 5 months. She noticed a mass of the right elbow 11 years earlier, and she had a past history of undergoing tumor resection and flap surgery at another hospital 9 years earlier, and the mass was diagnosed as a giant cell tumor. On pathological examination, the margin of the resected tumor was diagnosed as intralesional resection. However, she did not go to the hospital postoperatively. On physical examination, there was a poorly mobile mass measuring 8 × 5 cm on the olecranon side of the right elbow joint. She had diabetes mellitus and chronic renal failure, with a shunt on the right forearm. On magnetic resonance imaging (MRI), this tumor around the elbow joint showed low signal intensity on T1-weighted images and low to high intensity on T2-weighted images. After administration of gadolinium contrast, it was enhanced irregularly. A needle biopsy was performed, and histopathologic examination showed a giant cell tumor resembling the pathological findings 9 years earlier, with no malignancy.
The tumor gradually grew larger and formed ulcers. The tumor was present almost over the entire circumference of the upper arm and invaded the humerus, with the shunt blood vessel in the right forearm. Therefore, it seemed that it was difficult to preserve the limb, and upper arm amputation was performed. Pathological examination showed invasive proliferation to the synovial membrane, osteoclast-like giant cells, proliferation of round cells, and hemosiderin accumulation between cells (Fig. 1). In addition, lesions were continuous from the periosteum and proliferated invasively in the dermis. The histological diagnosis was PVNS. The patient’s postoperative course was uneventful. There was no recurrence of PVNS at the most recent follow-up 2 years after surgery.
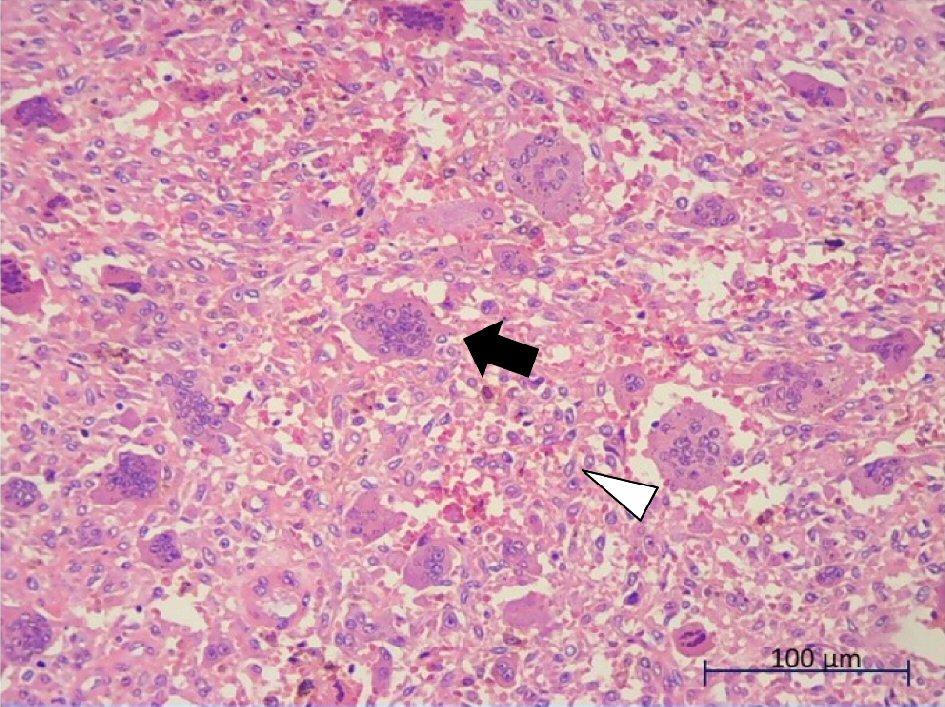 Click for large image | Figure 1. Histopathological findings of a surgically resected specimen on hematoxylin and eosin (H&E) staining (× 200). It shows invasive proliferation to the synovial membrane, osteoclast-like giant cells (arrow), proliferation of round cells (arrowhead), and hemosiderin accumulation between cells. |
| Discussion | ▴Top |
PVNS is a benign proliferative disorder of unknown origin forming nodular or villous changes in joints, synovial capsules, and tendon sheaths [3]. PVNS is one of the benign tumors, so-called fibrohistiocytic tumors, and it is classified as diffuse type in tenosynovial giant cell tumor [4]. It generally has an intra-articular origin, and it shows extensive involvement of the synovial membrane and capsule [5]. PVNS with extra-articular extension is rare [6], and most have been reported to occur in the knee and hip joints [7, 8]. PVNS in the elbow is uncommon, with only 24 cases reported in the literature [9, 10]. Although a few cases of extra-articular giant cell tumor of the tendon sheath occurred at the elbow, there have been no reports of PVNS with extra-articular extension affecting the elbow joint [5].
If it is left untreated, the hypertrophic synovium and multiple soft-tissue masses may lead to continued pain, decreased range of motion, joint destruction, and osteoarthritis [11]. Therefore, operative management, such as open excision or arthroscopic excision, is often required. The recurrence rate after surgical treatment has been reported to be 31-33%, and it is important to completely resect the synovial membrane [12, 13]. However, complete resection is difficult if it occurs within complex joints such as the elbow joint [14]. To minimize the risk of recurrence, several studies have demonstrated a positive response with radiation therapy or adjuvant therapy [13, 15]. However, their effects are still controversial [16]. There are no cases of PVNS that required amputation of a limb. PVNS must be carefully treated because of its invasiveness, though it is not a malignant tumor.
In conclusion, a rare case of PVNS around the elbow joint that required upper arm amputation was presented. In the treatment of PVNS, initial surgery with complete resection of the synovial membrane and careful postoperative follow-up are considered important.
Acknowledgments
None to declare.
Financial Disclosure
The authors declare that there is no funding regarding the publication of this article.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Informed Consent
The patient and/or her family were informed that data from the case would be submitted for publication and gave their consent.
Author Contributions
YO and HT wrote the paper; NM, H. Nagasawa, H. Nanjo, and YS reviewed the paper; all authors gave the final approval.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore). 1980;59(3):223-238.
doi - Aydingoz U, Leblebicioglu G, Gedikoglu G, Atay OA. Pigmented villonodular synovitis of the elbow in a 6-year-old girl. J Shoulder Elbow Surg. 2002;11(3):274-277.
doi pubmed - Orhan Z, Oktas B, Yildirim U. An unusual presentation of peroneal neuropathy secondary to pigmented villonodular synovitis: a case report. Knee Surg Sports Traumatol Arthrosc. 2009;17(5):518-520.
doi pubmed - Fletcher CD, Bridge JA, Hogendoorn PC, Mertens F. WHO classification of tumours of soft tissue and bone. Pathology and genetics of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013.
- Savvidou OD, Mavrogenis AF, Sakellariou VI, Chloros GD, Sarlikiotis T, Papagelopoulos PJ. Extra-articular diffuse giant cell tumor of the tendon sheath: a report of 2 cases. Arch Bone Jt Surg. 2016;4(3):273-276.
- Somerhausen NS, Fletcher CD. Diffuse-type giant cell tumor: clinicopathologic and immunohistochemical analysis of 50 cases with extraarticular disease. Am J Surg Pathol. 2000;24(4):479-492.
doi pubmed - Park KS, Diwanji SR, Yang HK, Yoon TR, Seon JK. Pigmented villonodular synovitis of the hip presenting as a buttock mass treated by total hip arthroplasty. J Arthroplasty. 2010;25(2):333 e339-312.
doi pubmed - Wu CC, Pritsch T, Bickels J, Wienberg T, Malawer MM. Two incision synovectomy and radiation treatment for diffuse pigmented villonodular synovitis of the knee with extra-articular component. Knee. 2007;14(2):99-106.
doi pubmed - Byers PD, Cotton RE, Deacon OW, Lowy M, Newman PH, Sissons HA, Thomson AD. The diagnosis and treatment of pigmented villonodular synovitis. J Bone Joint Surg Br. 1968;50(2):290-305.
doi pubmed - Pimpalnerkar A, Barton E, Sibly TF. Pigmented villonodular synovitis of the elbow. J Shoulder Elbow Surg. 1998;7(1):71-75.
doi - Gu HF, Zhang SJ, Zhao C, Chen Y, Bi Q. A comparison of open and arthroscopic surgery for treatment of diffuse pigmented villonodular synovitis of the knee. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2830-2836.
doi pubmed - Auregan JC, Klouche S, Bohu Y, Lefevre N, Herman S, Hardy P. Treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 2014;30(10):1327-1341.
doi pubmed - de Carvalho LH, Jr., Soares LF, Goncalves MB, Temponi EF, de Melo Silva O, Jr. Long-term success in the treatment of diffuse pigmented villonodular synovitis of the knee with subtotal synovectomy and radiotherapy. Arthroscopy. 2012;28(9):1271-1274.
doi pubmed - Kohyama K, Sugiura H, Yamada K, Hyodo I, Kato H, Kamei Y. Posterior interosseous nerve palsy secondary to pigmented villonodular synovitis of the elbow: case report and review of literature. Orthop Traumatol Surg Res. 2013;99(2):247-251.
doi pubmed - Cassier PA, Gelderblom H, Stacchiotti S, Thomas D, Maki RG, Kroep JR, van der Graaf WT, et al. Efficacy of imatinib mesylate for the treatment of locally advanced and/or metastatic tenosynovial giant cell tumor/pigmented villonodular synovitis. Cancer. 2012;118(6):1649-1655.
doi pubmed - Stephan SR, Shallop B, Lackman R, Kim TW, Mulcahey MK. Pigmented villonodular synovitis: a comprehensive review and proposed treatment algorithm. JBJS Rev. 2016;4(7).
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


