| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 12, Number 10, October 2021, pages 386-390
Giant Uterine Leiomyoma With Surgical Difficulty
Suzanna Mongana, Antonius Wibowoa, b
aDepartment of Obstetrics and Gynecology, Faculty of Medicine, Sam Ratulangi University - Prof R.D. Kandou Hospital, Manado 95163, North Sulawesi, Indonesia
bCorresponding Author: Antonius Wibowo, Department of Obstetrics and Gynecology, Faculty of Medicine, Sam Ratulangi University - Prof R.D. Kandou Hospital, Magnolia Residence, Ticoalu Mandagi Road No. 17, Manado 95163, North Sulawesi, Indonesia
Manuscript submitted August 1, 2021, accepted August 23, 2021, published online September 29, 2021
Short title: Difficult Surgery of Giant Uterine Myoma
doi: https://doi.org/10.14740/jmc3764
| Abstract | ▴Top |
Uterine leiomyoma is a benign gynecological tumor of the uterine myometrium layer in the female reproductive system, with clinical incidence in approximately 25% of women. In rare instances, it is possible for it to grow into a giant uterine leiomyoma (weighing 11.4 kg or more). Surgery on a giant mass is challenging because the enlargement mass affects the normal anatomical position of the internal genital organs. We report a case of a giant uterine leiomyoma with surgical difficulty. A 45-year-old woman came to the gynecology outpatient department referred from a district hospital with a suspected malignant ovarian cyst. The signs and symptoms were enlargement of the abdomen in the last 15 years, abdominal pain, and menstrual blood clots. An abdominal pelvic computed tomography (CT) scan with contrast revealed a regular cystic mass with multiple solid components and thick septa, probably from the adnexa. The biochemical examination revealed an increase in CA-125 serum (102.6 U/mL) with a risk of malignancy index (RMI) score of 308. Considering the size of the mass, fixed to the abdomen with umbilical hernia and suspicions of uterine or ovarian malignancy, the patient was planned for a laparotomy with collaborating digestive surgeon and urologist. The intraoperative findings were enlargement of the uterus with cystic degeneration of the leiomyoma at the posterior wall of the uterus. Due to the size of the mass, the anatomical position of the internal genital organs was deviated. The ovaries and fallopian tubes were normal, and total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed. The mass measured 57 × 51 cm in size and 26 kg in weight. Histopathological examination revealed a uterine leiomyoma with cystic degeneration.
Keywords: Giant uterine leiomyoma; Total hysterectomy; Salpingo-oophorectomy
| Introduction | ▴Top |
Uterine leiomyoma is considered as the most common benign gynecological tumor of the uterine myometrium layer in the female reproductive system [1, 2]. Based on its clinical incidence, it is found in approximately 25% of women with increasing prevalence throughout reproductive age and decreasing prevalence after the menopause [2]. The pathogenesis of leiomyomas is currently dilemmatic, nonetheless hormonal stimulation of estrogen, progesterone, and other growth factors plays a significant role. Based on its location, leiomyomas are classified into: subserosa, intramural, and submucosal [3]. Smaller leiomyomas are more prevalent; nevertheless, in rare instances, it is possible for them to grow into giant myoma (weighing 11.4 kg or more) [2, 4]. In cases of giant uterine leiomyoma, evidence-based guidelines for management are limited to conservative management. The increase in leiomyoma size often complicates surgery, which often leads to total or subtotal hysterectomy [5]. We present a case of a giant uterine leiomyoma that we managed, diagnosed and surgically managed in Prof. Dr. R.D. Kandou Hospital in Manado.
| Case Report | ▴Top |
Investigations
A 45-year-old nulligravida patient came to our obstetrics and gynecology outpatient department at Prof R. D. Kandou Hospital Manado with a referral letter from a primary health clinic and diagnosed with questionable ovarian cysts. The patient had an enlarged abdomen accompanied by intermittent lower abdominal pain, and difficulty breathing, especially in the supine position that had progressed since approximately 15 years ago. The patient denied having any history of weight loss, non-menstrual vaginal bleeding, or any problems regarding micturition or defecation. The patient had a history of controlled hypertension with routine oral medications. The patient was not yet married, she experienced her first menstrual period at the age of 13 years with a regular cycle that lasts for 5 - 6 days, changed tampons 6 - 7 times a day, and denied having menstrual pain, with her last menstrual period on April 26, 2019. Vital signs and general examinations were unremarkable. Abdominal examination revealed a mobile cystic mass at the tip of the xiphoid process, another mass was also visible protruding from the umbilicus, and no lymph nodes were palpable. Gynecological examination of the hymen and lower reproductive tract was unremarkable.
Diagnosis
Transabdominal sonography revealed a large heterogenous mass that originated from the pelvic region and expanded throughout the whole abdominal cavity with difficulty differentiating the uterus from surrounding structures; no lymph node enlargement was visible. Abdominal and pelvic computed tomography (CT) scan with contrast revealed cystic mass measuring approximately 43 × 41 × 30 cm with clearly demarcated outer layer, multiple solid inner components and thick inner septations; no lymph node enlargement was visible (Fig. 1). Chest X-ray results were unremarkable without any lymph node enlargement. Routine blood workout revealed low hemoglobin concentration (Hb: 8.3 g/dL) and increase in CA-125 marker was noted (CA-125: 102.6 IU/mL). The patient was initially diagnosed with questionable ovarian cyst and umbilical hernia. Exploratory laparotomy surgery with digestive surgeon and urologist supervision was planned after considering the size of the mass (Fig. 2).
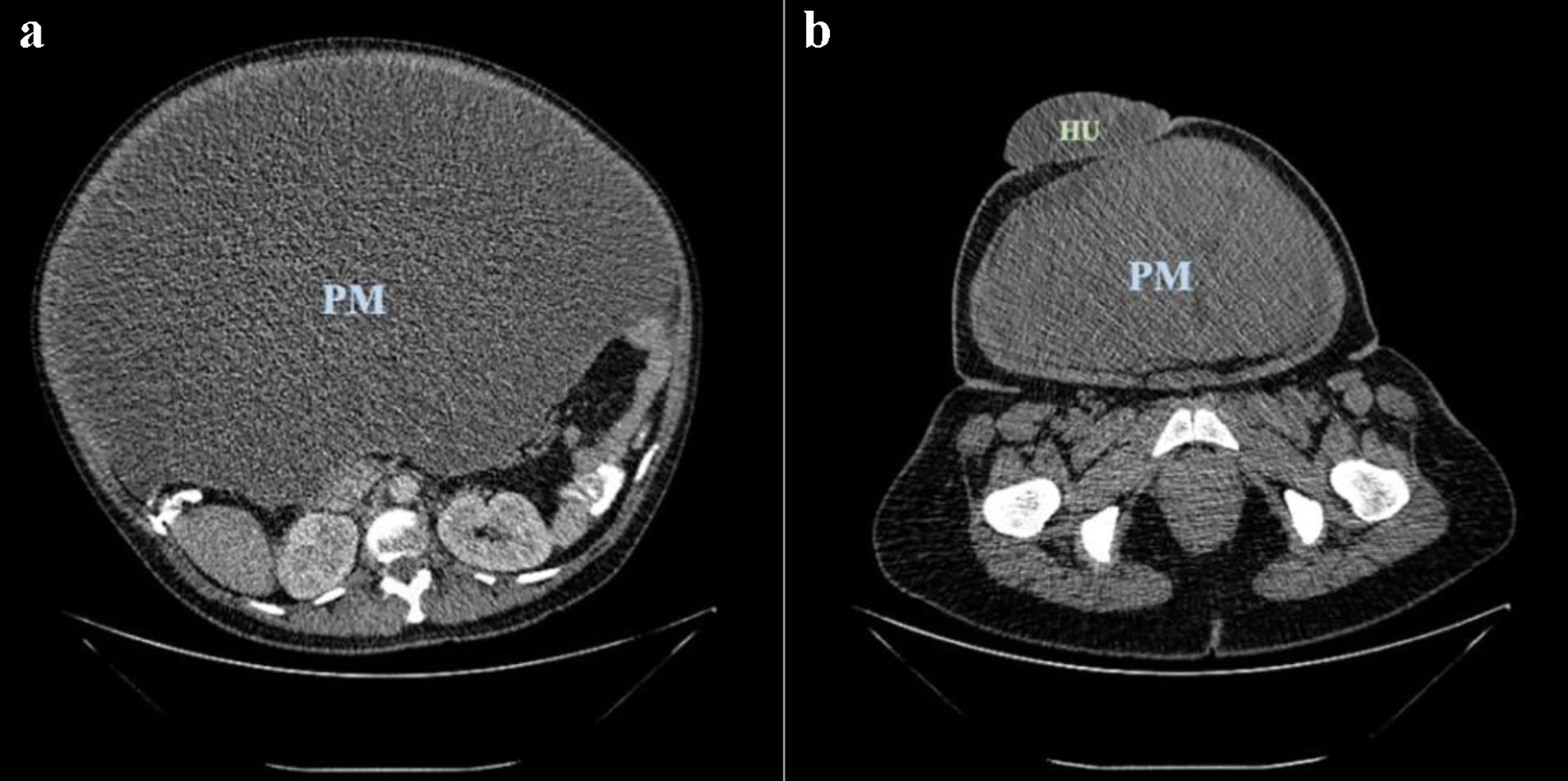 Click for large image | Figure 1. Pelvic mass (PM) (a) and umbilical hernia (HU) (b) seen on abdomen-pelvis computed tomography (CT) scan. |
 Click for large image | Figure 2. Pre-operative view of the patient’s abdomen. |
Treatment
During pre-operative stages, a laparotomy was planned with a digestive surgeon and urologist’s assistance for installation of a ureteral catheter, but the installation was aborted due to intraoperative difficulty. Laparotomy began with an initial median incision that was extended as wide as needed for the mass to be easily manipulated and evacuated. After the peritoneum layer was opened the cystic mass was visibly filling the entire abdominal cavity, cyst decompression was followed with extraction of approximately 200 cc mucinous fluid out of the cysts.
During exploration, a mass originating from the posterior uterus was visible with dimensions measuring approximately 57 × 51 × 21 cm and weighing 26 kg on macroscopic examination (Figs. 3 and 4). Histopathological examination of the mass confirmed a uterine leiomyoma with cystic degeneration with normal adnexal structures, bilateral fallopian tubes and ovaries was identified and adhered to the posterior uterine wall.
 Click for large image | Figure 3. Intra-operative view of the patient’s abdomen. |
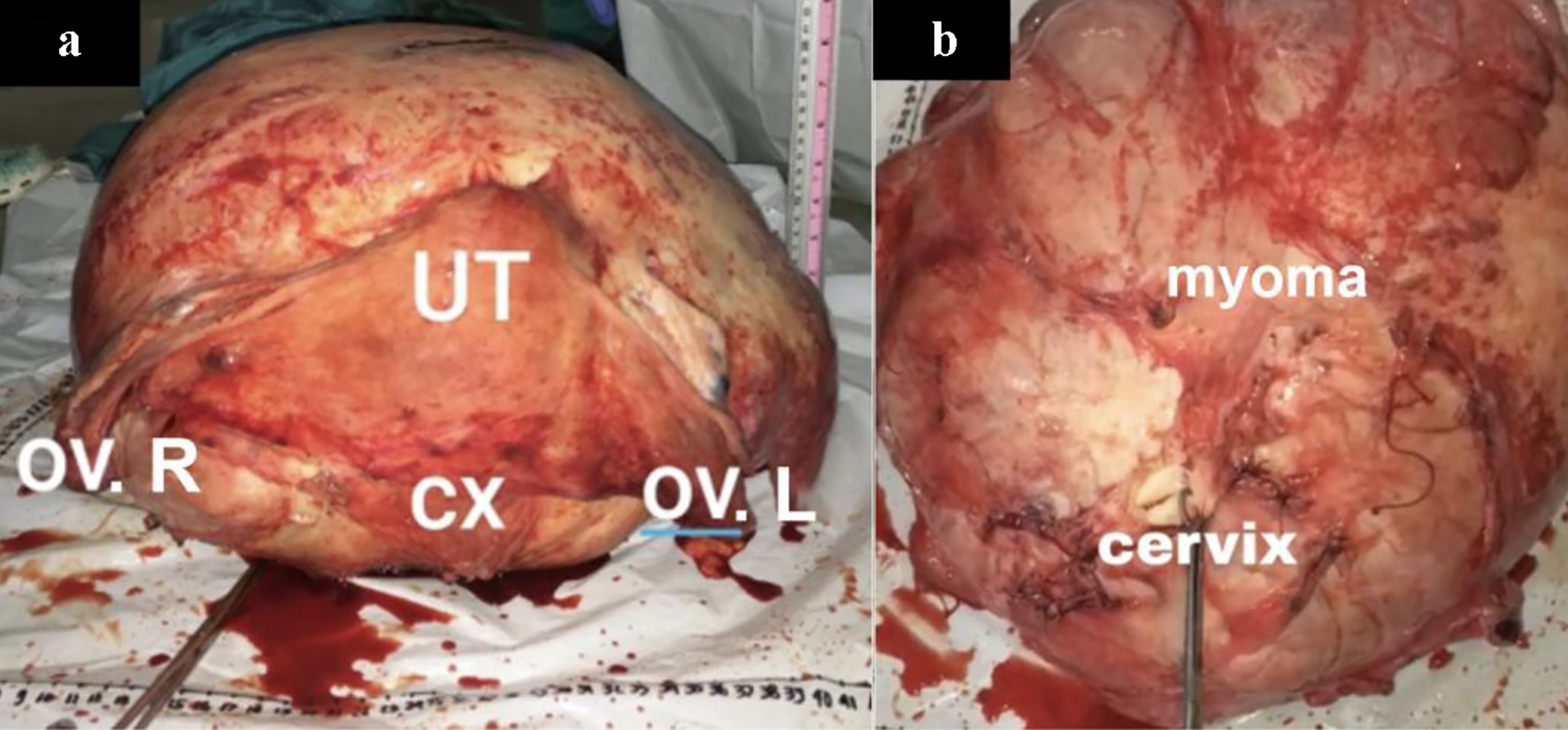 Click for large image | Figure 4. Giant uterine leiomyoma (myoma) after laparotomy evacuation with surrounding pelvic structures: uterus (UT), right ovary (OV. R), left ovary (OV. L), cervix (CX). |
After further consideration of the condition, a total hysterectomy with bilateral salpingo-oophorectomy was later performed with patient consent. Bilateral round ligaments were clamped, excised, and sutured. The vesico-uterine layer was identified and widely excised until the bottom end of the round ligaments. Bilateral ureters were observed when the posterior latum ligament was incised. The bilateral infundibulopelvic ligaments were clamped, incised, and sutured. Bilateral uterine arteries were identified while exploring the ureter to uterine artery intersections, followed with incision and suture. The vaginal vault was identified, clamped, and sutured.
Follow-up and outcomes
Gigantic mass size creates change in pelvic anatomy such as ureteral deviation, which requires caution in performing the laparotomy procedure to prevent complications in adjacent abdominal organs such as ureteral resection, gastrointestinal perforation, etc. After a total hysterectomy with bilateral salpingo-oophorectomy was performed, bleeding evaluation was performed to exclude possibilities of pelvic trauma, followed by umbilical hernia repair by a digestive surgeon. Surgical drainage was installed before wound closure. After surgery, the patient was observed for 5 days and was discharged afterwards without any complaints, and outpatient department follow-up was scheduled for the patient.
| Discussion | ▴Top |
Giant leiomyoma is a common benign tumor of the uterus with a measured weight greater than 11.4 kg or with a measured diameter greater than 17 cm or with measured dimensions of 33 × 28 × 22 cm [1]. Histopathologic microscopic examination of uterine leiomyoma may reveal four types of degeneration forms: hyalin, cystic, myxoid or red, and dystrophic degenerations. Hyalin degeneration is the most common form of leiomyoma degeneration; in contrast, cystic degeneration only occurs in 4% of cases [6].
Uterine leiomyoma has a potency to grow into extreme sizes when symptoms of abdominal compression occur. Increase in mass volume causes abdominal wall distention, which causes most complaints of patient discomfort. Most leiomyoma cases take decades to progress into giant leiomyoma, which is considered slow; consequently, most patients seek treatment in later stages with non-typical symptoms of mass compression. The combined pre- and post-operative mortality rate comprises 16% of all cases [4, 7].
Pelvic physical examination is an initial method of diagnostic evaluation, nevertheless smaller myoma size increases difficulty in palpating the mass, which may result in underdiagnosed cases. Therefore, additional diagnostic imaging is required to increase diagnostic sensitivity, and to further evaluate number, size, location, and extension of the mass [1]. Ultrasonography is the most preferable initial method of imaging due to it being less invasive and its low cost. CT and magnetic resonance imaging (MRI) are advantageous in further excluding the possibility of other benign or malignant lesions. MRI has a higher specificity compared to CT scan in detecting signs of calcification or necrosis, but it is not widely available and has a higher cost [7]. Tumor markers also play an additional vital role in excluding possibilities of malignancy. Due to each having its own advantages and disadvantages, there is no single best diagnostic modality for giant uterine leiomyoma before a diagnostic laparotomy followed by histopathologic examination is performed. Possible differential diagnosis includes adenomyosis, hematometra, uterine malignancy (carcinoma, sarcoma or carcinosarcoma), retroperitoneal ovarian cysts or ovarian malignancy [8]. In this reported case, the examined tumor marker of CA-125 was 102.6 IU/mL, which is significantly high, with an RMI of 308. After considering the size of the mass and its high ovarian malignant risk, a laparotomy was planned with the assistance of a digestive surgeon and urologist.
This patient’s treatment was consistent with the literature on giant uterine leiomyoma management, in which the management option depends on other factors, which include age, type of lesion, severity of symptoms, malignancy probability, and fertility conservation [9, 10]. Indications for surgical management include abnormal uterine bleeding that does not resolve after conservative treatment, secondary iron deficiency to chronic bleeding anemia, severe abdominal pain due to mass compression that reduce the patient’s quality of life, and suspicion of malignancy.
Surgical management of this patient’s tumor (diameter > 25 cm) was challenging due to massive blood loss caused by increased vascularization and possibilities of post-operative complications, which include trauma of urinary tract or gastrointestinal infection, and hematoma. Pre-operative assessment of the patient must be performed thoroughly, in order to prevent possible intra-operative and post-operative complications [7, 9]. Proper skin excision has to be performed in order to effectively manipulate the mass and examine the upper abdominal region [4, 9]. En-bloc evacuation reduces bleeding risk. Potential bleeding sources include collateral circulation, arterio-venous shunting, and tumor size must be properly managed, since it is prone to hypovolemic shock due to anemia and poor nutritional status. Pelvic anatomical distortion due to uterine abnormality may increase injury risk in adjacent gastrointestinal and urinary structures [9].
Strict post-operative hemodynamic and breathing evaluation is necessary to evaluate evidence of bleeding origin. If fluid and blood product resuscitation fail to re-stabilize the patient’s condition, surgical re-exploration is urgently necessary. Precise perioperative management with multidisciplinary patient care is fundamental in preventing morbidity and mortality and accelerating recovery [1, 4].
In conclusion, giant uterine leiomyoma is a rare case in practice and management remains a challenge. Management depends on individual factors such as the patient’s desire to conserve fertility. Careful pre-operative assessment and multidisciplinary efforts are necessary to prevent further operative complications, morbidity, and mortality. The extreme size of mass complicates surgery due to pelvic anatomy distortion; therefore, proper understanding of pelvic anatomy and teamwork is necessary to ensure surgery success.
Acknowledgments
The authors would like to acknowledge the valuable input and support from the doctors, paramedics, and sonographers from the Department of Obstetrics and Gynecology, Faculty of Medicine, Sam Ratulangi University - Prof. R. D. Kandou Hospital, Manado.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Written informed consent was obtained from the patient.
Author Contributions
All authors contributed a specific role in the conception and editing of the manuscript. Suzanna Mongan performed the patient’s care; provided substantial contributions in the conception and design of the manuscript; critically revised the article and gave final approval of the version to be published. Antonius Wibowo made substantial contributions to acquisition of data, analysis and interpretation of data, and critical revision of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Kalyan S, Sharma S. Giant uterine leiomyoma: a case report with literature review. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2018;7(11):4780.
doi - Mulayim B. Unaware of a large leiomyoma: A case report with respect to unusual symptoms of large leiomyomas. Ann Med Surg (Lond). 2015;4(4):431-433.
doi pubmed - American Association of Gynecologic Laparoscopists (AAGL): Advancing Minimally Invasive Gynecology Worldwide. AAGL practice report: practice guidelines for the diagnosis and management of submucous leiomyomas. J Minim Invasive Gynecol. 2012;19(2):152-171.
doi pubmed - Steward RG, Denhartog HW, Katz AR. Giant uterine leiomyomata. Fertil Steril. 2011;95(3):1121 e1115-1127.
doi pubmed - Wronski K. Giant uterine leiomyoma-case report and review of literature. New Medicine. 2014;18:89-91.
- Della Rossa MG, Santana BN, Verdejo-Arias MR, Cardenas EV, Arranz JP. Uterine reconstruction due to a giant myoma. a case report and literature review. Open Journal of Obstetrics and Gynecology. 2016;6(01):64.
doi - Alam IP, Newaz R. A case of giant fibroid uterus. Bangladesh Journal of Obstetrics & Gynaecology. 2012;27(1):27-30.
doi - Aydin C, Eris S, Yalcin Y, Sen Selim H. A giant cystic leiomyoma mimicking an ovarian malignancy. Int J Surg Case Rep. 2013;4(11):1010-1012.
doi pubmed - Panayotidis C, Salleh S, Martin JE, Hirsh P, Wynn J. Giant uterine leiomyomas: dilemmas in surgical management. Gynecological Surgery. 2006;3(1):37-40.
doi - Vilos GA, Allaire C, Laberge PY, Leyland N. SOGC Clinical practice guideline N 318. The Management of Uterine Leiomyomas. 2003 [updated 2015 Feb].
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


