| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 6, December 2011, pages 289-291
Isolated Optic Chiasmal Neuritis Secondary to Varicella-Zoster Virus Infection
Hiromasa Tsudaa, c, Kozue Tanakaa, Shuji Kishidaa, Noriko Ozakib
aDepartment of Neurology, Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital, 3-18-22, Honkomagome, Bunkyo-ku, 113-8677 Tokyo, Japan
bDepartment of Ophthalmology, Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital,3-18-22, Honkomagome, Bunkyo-ku, 113-8677 Tokyo, Japan
cCorresponding author: Department of Neurology, Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital. 3-18-22, Honkomagome, Bunkyo-ku, 113-8677, Tokyo, Japan. E-mail:
Manuscript accepted for publication October 5, 2011
Short title: Isolated Optic Chiasmal Neuritis
doi: https://doi.org/10.4021/jmc378w
| Abstract | ▴Top |
A 49-year-old woman without contributory medical history presented with zoster in the left-sided second cervical dermatome, and underwent oral valaciclovir at 3000 mg/day. Five days later, bitemporal hemianopia developed. Corrected visual acuities were spared, and funduscopic findings demonstrated no abnormalities in both eyes. Varicella-zoster virus (VZV) viremia was proved by the polymerase chain reaction test. Cerebrospinal fluid examination findings were normal. Cranial and orbital magnetic resonance imaging demonstrated no abnormalities. Thereafter, under 7 days of intravenous aciclovir at 1500 mg/day, bitemporal hemianopia gradually improved. This is a first reported case of isolated optic chiasmal neuritis secondary to VZV infection.
Keywords: Acyclovir; Bitemporal hemianopia; Chiasmitis (chiasmopathy); Optic chiasmal syndrome; VZV viremia
| Introduction | ▴Top |
It is well known that varicella-zoster virus (VZV) may cause optic neuritis and retinitis [1, 2]. However, there has been only one reported case of optic chiasm involvements in addition to optic neuritis and retinitis caused by VZV infection [1]. Here, we describe a first reported case of isolated optic chiasmal neuritis (OCN) secondary to VZV viremia.
| Case Report | ▴Top |
A 49-year-old woman without contributory medical history presented with persistent pain and scatteredvesicular cutaneous eruptions in the left-sided second cervical dermatome on February 2011. She was diagnosed as having zoster by the dermatologist, and oral valaciclovir at 3000 mg/day was initiated. Five days later, she complained of visual field defect in both eyes, which gradually worsened. Therefore, she was admitted to our Neurologic Ward. The zoster skin lesions were improved, and no other abnormalities like erythema, discoid rash or photosensitivity disorder were noted. General examination findings were normal. Corrected visual acuity was 1.5, and critical flicker fusion frequency was within normal ranges in both eyes. Confrontational visual fields suggested a defect in the temporal field of both eyes and Goldmann perimetry confirmed a bitemporal heminopsia (Fig. 1). In both eyes, the diameter of the pupil was 3 mm in the lightened room. Light and near reflexes were prompt in either eye. There was no relative afferent papillary defect. Restriction of eye movements was not observed. Palpebral fissure was 9 mm in both eyes. Funduscopic findings did not demonstrate any abnormalities in either eye. Other than a mild sensory disturbance in the region of the left second cervical dermatome, the remainder of the neurologic examination was normal. In the laboratory examinations of the blood, complete blood counts, blood chemistry, erythrocyte sedimentation rate, prothrombin time, activated partial thromboplastin time, thyroid function, angiotensin coverting enzyme level, and vitamin B12 level were within normal ranges. Both the serological test for syphilis and treponema pallidum hemagglutination were negative. In the blood, the polymerase chain reaction (PCR) test of VZV was positive, though IgM titer of mumps virus, cytomegalovirus (CMV), and Epstein-Barr virus (EBV) were all negative. On the immunological examination, despite a slight elevated titer of anti-nuclear antibody at 1: 80, anti-Smith antibody, anti-double-stranded DNA antibody, and perinuclear anti-neutrophil cytoplasmic antibody were all negative. In the complement tests, the levels of C3, C4 and CH50 were within normal ranges. Urinary examination demonstrated normal findings. The cerebrospinal fluid (CSF) was watery clear appearance. The CSF examination demonstrated an initial pressure at 130 mmH2O, cell counts at 3 /mm3 (all was mononucleocyte), glucose level at 60 mg/dl, and total protein concentration at 20 mg/dl. The cytological examination, the culture test, oligoclonal IgG band, and the PCR test of VZV resulted in negative study in the CSF. Chest roentgen and electrocardiogram findings were normal. Not only cranial and orbital magnetic resonance imaging (MRI) but also cranial magnetic resonance angiography demonstrated no abnormalities. Then, she was considered as having isolated OCN secondary to VZV viremia. Under 7 days of intravenous aciclovir at 1500 mg/day, her bitemporal hemianopia gradually improved.
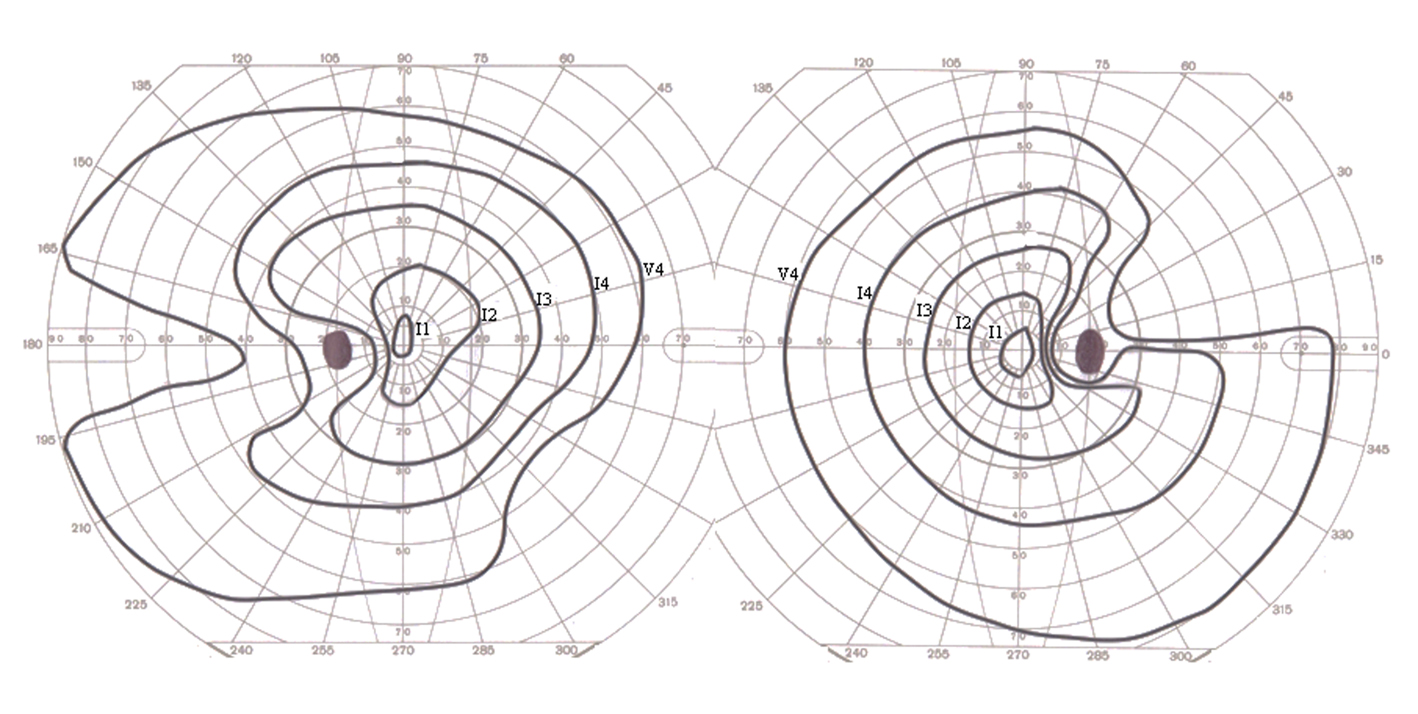 Click for large image | Figure 1. Goldmann perimetry demonstrated bitemporal hemianopia. |
| Discussion | ▴Top |
Visual field defect may be the earliest symptom in patients with lesions involving the optic chiasm [3].Consequently, perimetry is the most important clinical tool for detecting chiasmal lesion, and bitemporal hamianopia is commonly observed [3, 4]. On the other hand, chiasmal involvement may be induced by extrinsic or intrinsic abnormalities [3, 4]. Regarding intrinsic chiasmal lesions, neoplasm [3, 5-7], chiasmal infarction [3, 8, 9], sarcoidosis [3, 10], and OCN [1, 3, 11-19] have been reported. Among them, OCN is a relatively rare symptom consisting of acute visual loss due to chiasmal inflammation [1, 3, 11-19], and commonly occurs as an idiopathic event, either in isolation or in the setting of multiple sclerosis [3, 11]. Furthermore, previous reports have noted that VZV infection, infectious mononucleosis due to EBV [12], CMV infection [13], mumps parotitis [14], Lyme disease [15], neuromyelitis optica [16], systemic lupus erythematosus [17], vitamin B12 deficiency [18], and ethchlorvynol toxicity [19] might induce OCN. Among them, there has been only one reported case of OCN due to VZV infection [1]. This patient was an immunocompromised host [1]. Bitemporal hemianopia with severe bilateral impairment of corrected visual acuities, and retinochoroiditis in the right eye were initially observed [1]. MRI demonstrated involvements of the chiasm and bilateral optic nerves [1]. Antiviral agent was not administered [1]. Then, within a week, retinitis also appeared in the left eye [1]. In 2 days, he became blind [1]. Based on the postmortem examination, infiltration of VZV to the optic nerves as well as retinae was confirmed [1].
In our present patient, no other ophthalmological abnormalities except for bitemporal hemianopia were observed. MRI demonstrated no abnormalities in the vicinity of the optic chiasm. In addition, VZV viremia was proved by the PCR test. She was not an immunocompromised host, and intravenous antiviral agent was immediately initiated when bitemporal hemianopia developed. Therefore, it was considered that infiltration of VZV might not be severe, and be localized to the optic chiasm. In conclusion, we emphasize that this is a first reported case of isolated OCN secondary to VZV viremia.
Conflicts of Interest
No conflict of interest exists.
| References | ▴Top |
- Greven CM, Singh T, Stanton CA, Martin TJ. Optic chiasm, optic nerve, and retinal involvement secondary to varicella-zoster virus. Arch Ophthalmol. 2001;119(4):608-610.
pubmed - Nagel MA, Gilden DH. The protean neurologic manifestations of varicella-zoster virus infection. Cleve Clin J Med. 2007;74(7):489-494, 496, 498-489 passim.
pubmed - Foroozan R. Chiasmal syndromes. Curr Opin Ophthalmol. 2003;14(6):325-331.
pubmed doi - Mejico LJ, Miller NR, Dong LM. Clinical features associated with lesions other than pituitary adenoma in patients with an optic chiasmal syndrome. Am J Ophthalmol. 2004;137(5):908-913.
pubmed doi - Alvord EC, Jr., Lofton S. Gliomas of the optic nerve or chiasm. Outcome by patients' age, tumor site, and treatment. J Neurosurg. 1988;68(1):85-98.
pubmed doi - Arai A, Morishita A, Hanada Y, Aihara H. Solitary metastatic tumor within the optic chiasm—case report. Neurol Med Chir (Tokyo). 2010;50(2):158-161.
pubmed doi - Lee AG, Tang RA, Roberts D, Schiffman JS, Osborne A. Primary central nervous system lymphoma involving the optic chiasm in AIDS. J Neuroophthalmol. 2001;21(2):95-98.
pubmed doi - Lee KF. Ischemic chiasma syndrome. AJNR Am J Neuroradiol. 1983;4(3):777-780.
pubmed - Fabian ID, Greenberg G, Huna-Baron R. Chiasmal stroke following open-heart surgery. J Neuroophthalmol. 2010;30(3):219-221.
pubmed doi - Hosseini H, Tourbah A. Sarcoid related optochiasmatic arachnoiditis: favourable outcome confirmed with MRI. J Neurol Neurosurg Psychiatry. 1999;67(5):690.
pubmed doi - Kawasaki A, Purvin VA. Idiopathic chiasmal neuritis: clinical features and prognosis. Arch Ophthalmol. 2009;127(1):76-81.
pubmed doi - Purvin V, Herr GJ, De Myer W. Chiasmal neuritis as a complication of Epstein-Barr virus infection. Arch Neurol. 1988;45(4):458-460.
pubmed - Pershing S, Dunn J, Khan A, Liao YJ. Cytomegalovirus infection with MRI signal abnormalities affecting the optic nerves, optic chiasm, and optic tracts. J Neuroophthalmol. 2009;29(3):223-226.
pubmed doi - Irioka T, Akaza M, Nakao K, Kanouchi T, Yokota T, Mizusawa H. Chiasmal optic neuritis following mumps parotitis. J Neurol. 2008;255(5):773-774.
pubmed doi - Scott IU, Silva-Lepe A, Siatkowski RM. Chiasmal optic neuritis in Lyme disease. Am J Ophthalmol. 1997;123(1):136-138.
pubmed - Costa RM, Santos AC, Costa LS. An unusual chiasmal visual defect in a patient with neuromyelitis optica: case report. Arq Bras Oftalmol. 2007;70(1):153-155.
pubmed doi - Siatkowski RM, Scott IU, Verm AM, Warn AA, Farris BK, Strominger MB, Sklar EM. Optic neuropathy and chiasmopathy in the diagnosis of systemic lupus erythematosus. J Neuroophthalmol. 2001;21(3):193-198.
pubmed doi - Wilhelm H, Grodd W, Schiefer U, Zrenner E. Uncommon chiasmal lesions: demyelinating disease, vasculitis, and cobalamin deficiency. Ger J Ophthalmol. 1993;2(4-5):234-240.
pubmed - Reynolds WD, Smith JL, McCrary JA, 3rd. Chiasmal optic neuritis. J Clin Neuroophthalmol. 1982;2(2):93-101.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


