| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 4, April 2022, pages 183-187
Endoscopic Ultrasound-Guided Rendezvous for Biliary Obstruction in Patient With Prior Whipple Surgery
Mohammad Arfeena, Nicholas M. McDonaldb, Mohammad Bilalb, c
aDepartment of Gastroenterology, Franciscan Health Olympia Fields, Olympia Fields, IL 60461, USA
bDivision of Gastroenterology & Hepatology, Minneapolis VA Medical Center, University of Minnesota, Minneapolis, MN 55417, USA
cCorresponding Author: Mohammad Bilal, Division of Gastroenterology & Hepatology, Minneapolis VA Medical Center, University of Minnesota, Minneapolis, MN 55417, USA
Manuscript submitted November 11, 2021, accepted March 17, 2022, published online March 25, 2022
Short title: EUS Rendezvous in Post-Whipple Patients
doi: https://doi.org/10.14740/jmc3842
| Abstract | ▴Top |
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy remains a challenging procedure even for the more experienced endoscopists. We present a unique case of an ERCP performed in a patient with prior Whipple surgery, where biliary access was obtained via an endoscopic ultrasound (EUS)-guided rendezvous technique, and cannulation was ultimately done using a modified therapeutic endoscope with successful biliary drainage.
Keywords: EUS rendezvous; ERCP; Post-Whipple; Surgically altered anatomy
| Introduction | ▴Top |
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy remains a challenging procedure even for experienced endoscopists. Challenges include accessing the biliary (afferent) limb, cannulation of the ampulla or hepaticojejunostomy often in suboptimal orientations, and the need for alternative endoscopes other than the conventional duodenoscope. In patients with prior Whipple surgery, a conventional duodenoscope can be used; however, in cases when the conventional duodenoscope cannot reach the biliary limb or the hepaticojejunostomy, the use of a conventional colonoscope, thin (pediatric) colonoscope and single-balloon enteroscopy-assisted ERCP has been reported [1, 2]. In select cases, even when the biliary limb is intubated, biliary cannulation may not be possible due to the factors mentioned above. Here we present a unique case of an ERCP performed in a patient with prior Whipple surgery where ERCP and biliary decompression was performed with assistance of endoscopic ultrasound (EUS) rendezvous approach.
| Case Report | ▴Top |
Investigations
A 72-year-old male with a prior history of extrahepatic cholangiocarcinoma status post a Whipple surgery 12 months prior and currently undergoing chemotherapy (on capecitabine and oxaliplatin) presented to the oncologist with painless jaundice.
Laboratory evaluation revealed a total bilirubin of 31.1 mg/dL (range 0.2 to 1.2 mg/dL). Patient had normal bilirubin levels 1 month prior to current presentation. Magnetic resonance cholangiopancreatography was performed and showed diffuse dilation of the biliary tree with an abrupt cut off at the level of the hepaticojejunal anastomosis suggestive of a stricture or recurrence of tumor (Fig. 1). Peritoneal carcinomatosis was also seen.
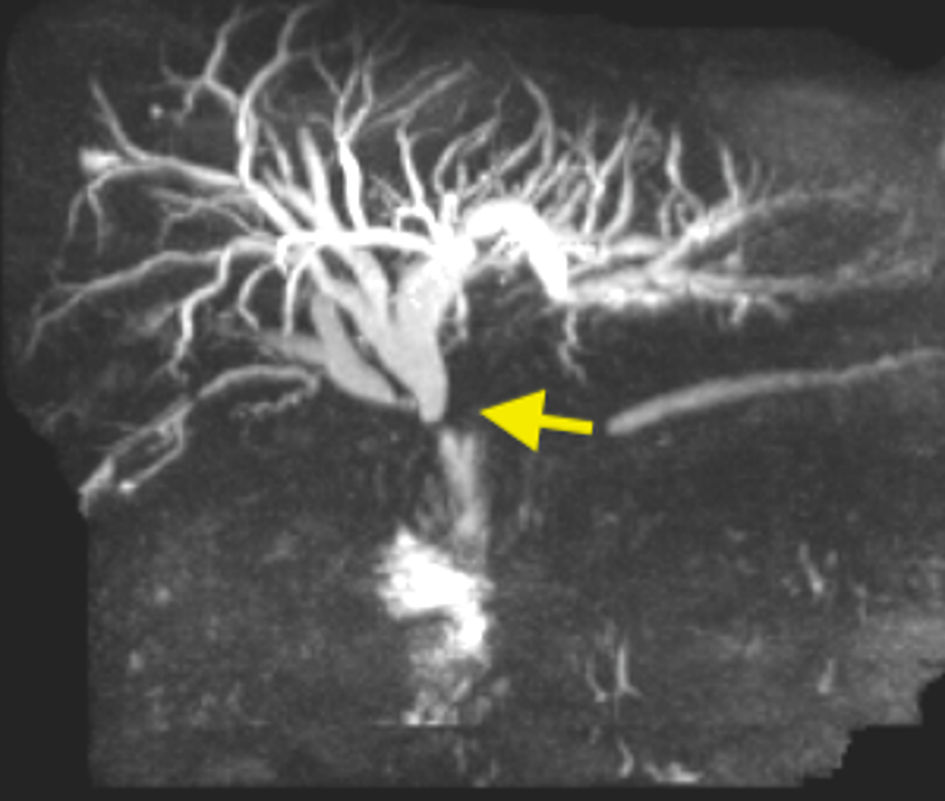 Click for large image | Figure 1. Magnetic resonance cholangiopancreatography showing abrupt cut off at the level of the hepaticojejunal anastomosis (arrow) with diffuse biliary dilation. |
Diagnosis
Based on the results of the above investigations the diagnosis of a high-grade stenosis or stricture of the hepaticojejunal anastomosis was made.
Treatment
Gastroenterology was consulted and decision was made to proceed with ERCP. A traditional duodenoscope was utilized; however, the afferent limb was unable to be intubated. A modified therapeutic endoscope (1T; GIF-1TH190 Olympus, Center Valley, PA) was then used. The afferent limb was intubated and confirmed with the presence of suture material (Fig. 2). However, despite extensive interrogation, the hepaticojejunal anastomosis was not able to be identified. The decision was made to perform an EUS-guided rendezvous to obtain biliary access. A linear echoendoscope (GF-UCT180 Olympus, Center Valley, PA) was used and a left intrahepatic biliary radical was identified and punctured using a 19-gauge fine needle aspiration needle (Fig. 3). Biliary duct access was confirmed by aspiration of bile. Contrast was injected which showed diffuse dilation of the entire biliary tree with an abrupt cut off at the hepaticojejunal anastomosis (Fig. 4). No contrast was seen filling in the jejunum suggestive of a complete stenosis at the hepaticojejunal anastomosis. Then, a 0.025-inch and 450-cm long straight guidewire was placed across the hepaticojejunostomy stricture; and the echoendoscope was removed and the guidewire left in place (Fig. 5). The modified therapeutic endoscope with a clear distal attachment cap was then inserted to the afferent limb; and the hepaticojejunal anastomosis was identified by visualizing the guidewire entry point in the jejunum. There was complete stenosis of the hepaticojejunostomy anastomosis. The hepaticojejunal anastomosis was then cannulated next to the guidewire using a biliary balloon extraction catheter pre-loaded with a guidewire. Cholangiogram demonstrated intrahepatic biliary dilation and a focal stenosis at the level of the hepaticojejunostomy suggestive of recurrent cholangiocarcinoma. An uncovered metal stent (10 mm in diameter and 4 cm length) was successfully placed across the hepaticojejunal anastomosis (Fig. 6).
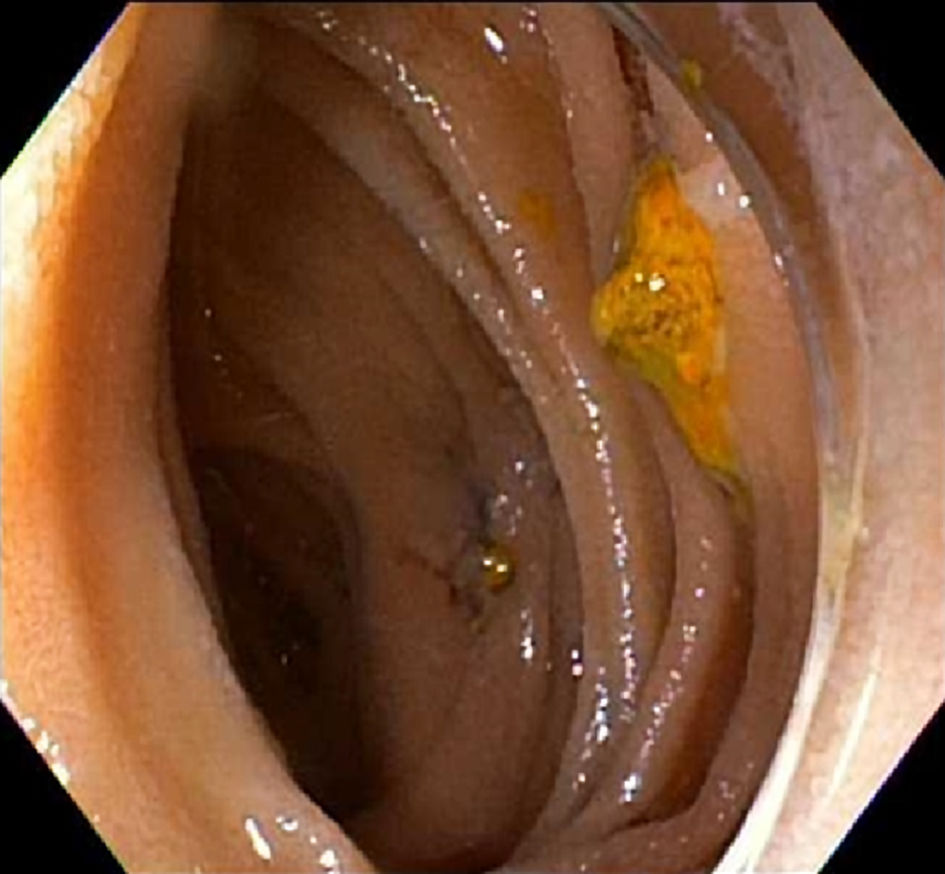 Click for large image | Figure 2. Suture material seen in jejunum suggestive of the biliary (afferent) limb. |
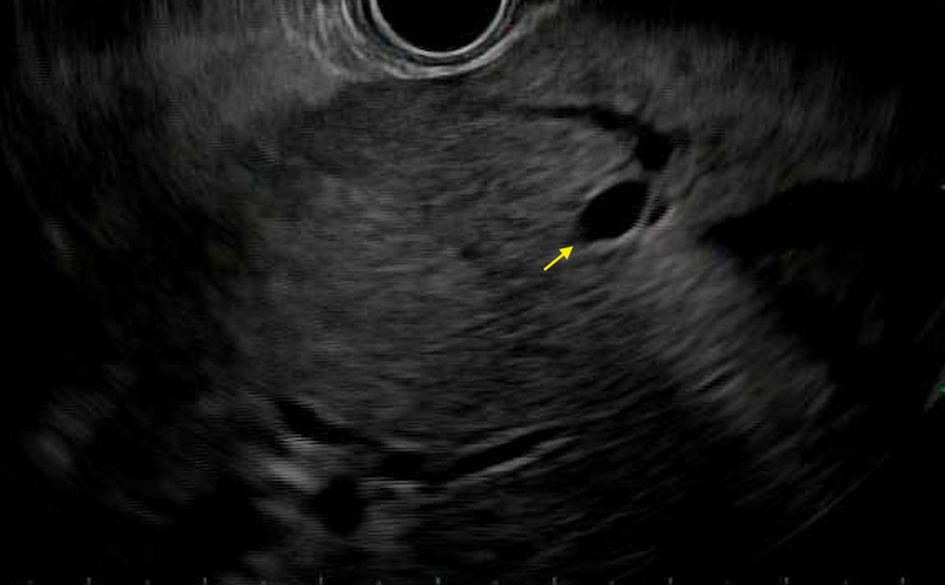 Click for large image | Figure 3. Endoscopic ultrasound showing left intra-hepatic biliary radical (arrow). |
 Click for large image | Figure 4. Contrast injection via echoendoscope showing diffuse dilation of biliary tree with abrupt cut off at the hepaticojejunal anastomosis (arrow). |
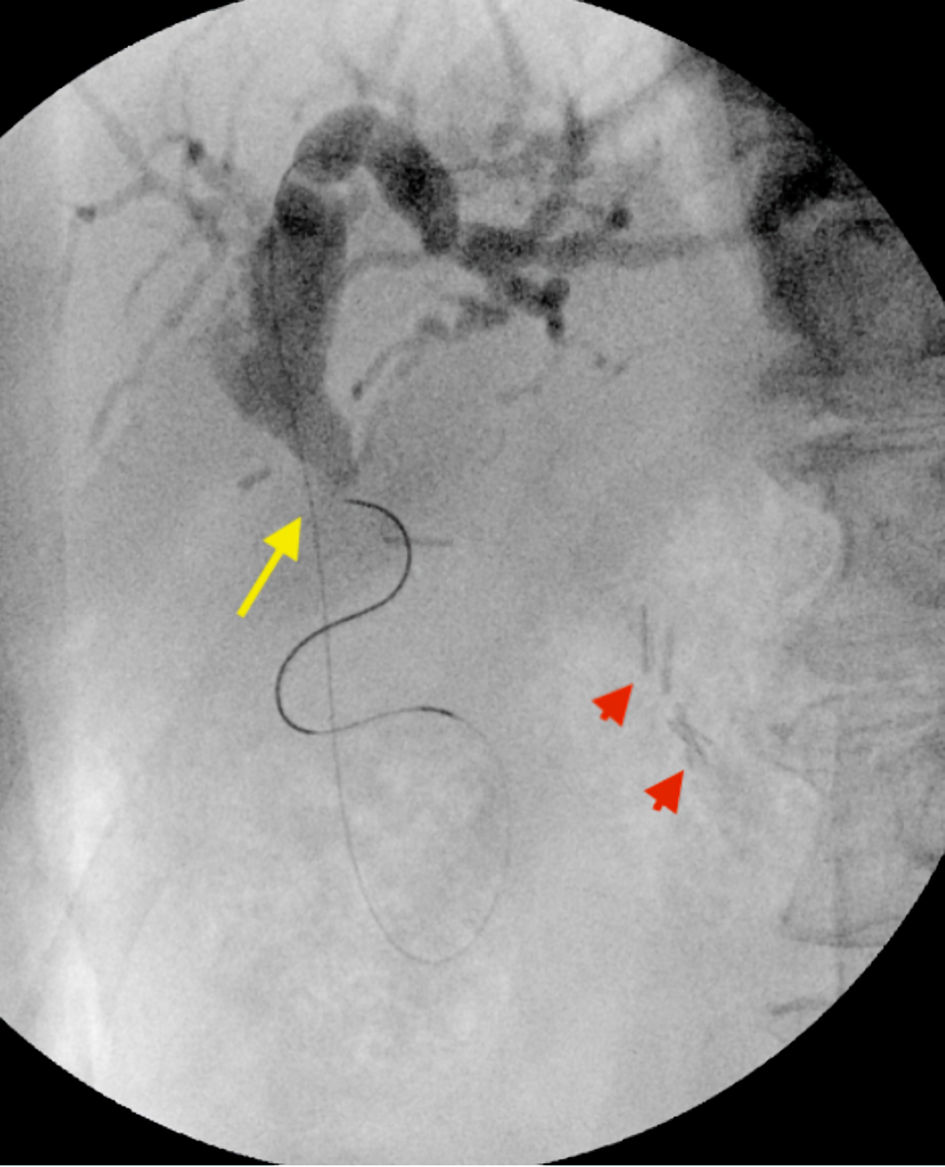 Click for large image | Figure 5. Fluoroscopy showing wire passage across the hepaticojejunal anastomosis into the jejunum (long yellow arrow), with short red arrows highlighting the view of hepaticojejunal anastomosis from the surgical clips. |
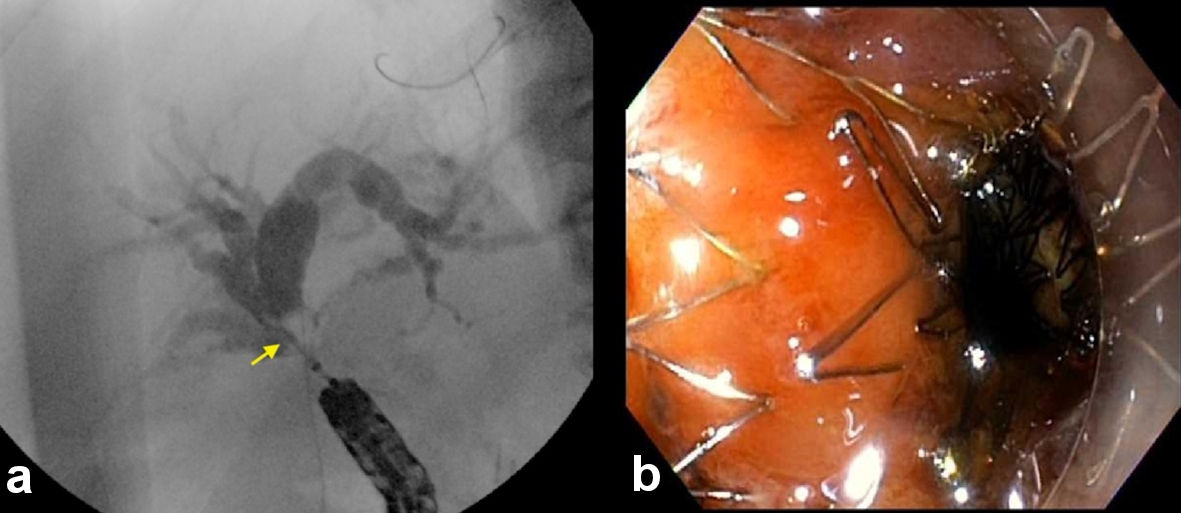 Click for large image | Figure 6. (a) Fluoroscopic view showing cannulation of the hepaticojejunal anastomosis using the modified therapeutic gastroscope (arrow). (b) Endoscopic view post placement of uncovered metal stent across the hepaticojejunal anastomosis (right). |
Follow-up and outcomes
The patient was observed in the hospital following the procedure and discharged on postoperative day 1. No procedural and anesthesia-related adverse events were noted. The patient’s total bilirubin levels were normal on 8 weeks’ follow-up.
| Discussion | ▴Top |
EUS rendezvous approach for biliary and pancreatic duct access was initially reported by Mallery et al in 2004. Since the initial reports, EUS rendezvous has been an essential tool in the arsenal of advanced endoscopists in instances of failed biliary cannulation during ERCP [3]. Traditionally there are three routes of access for EUS rendezvous, the trans-gastric puncture of the intrahepatic bile duct as was demonstrated in our case, as well as trans-duodenal puncture of the extrahepatic bile duct either from the proximal duodenum or the second part of the duodenum.
When attempting ERCP in patients with surgically altered anatomy several unique challenges exist depending on the surgical procedure the patient has undergone. Krutsri et al summarized these into three main challenges: accessing the afferent limb, reaching the ampulla or biliopancreatoenteric anastomosis, and then ultimately cannulating the desired duct in the new post-surgical orientation [4].
There are two forms of the Whipple procedure, the standard Whipple procedure and the pylorus preserving Whipple. In a standard Whipple the gastric antrum, gallbladder, distal common bile duct, head of the pancreas, duodenum, proximal jejunum and regional lymph nodes are resected with reconstruction consisting of pancreaticojejunostomy, hepaticojejunostomy, and gastrojejunostomy [2]. This is as opposed to the pylorus-preserving Whipple resection in which the stomach, pylorus and first 3 - 4 cm of the duodenum are preserved [2]. Depending on the position of the jejunal loop relative to the mesocolon the length of the afferent limb can vary from 40 to 60 cm [2].
In patients with long afferent limbs, access to the afferent limb is typically obtained using either a thin (pediatric) colonoscope, conventional colonoscope, or balloon enteroscopy-assisted ERCP due to the length of the limbs [5]. However, the therapeutic success rate remains variable [4]. Once the biliary limb is intubated and the hepaticojejunal anastomosis is identified, biliary cannulation can still be challenging due to the orientation of the anastomosis and lack of elevator mechanism if using an endoscope other than the traditional duodenoscope. Additionally, challenges can include the inability to use common ERCP instruments which may not be compatible with colonoscopes or balloon enteroscopes.
Another challenge was encountered in this case with the inability to identify the hepaticojejunostomy due to complete stricturing. If hepaticojejunostomy cannot be identified or cannulated, alternate endoscopic approaches include EUS-guided hepaticogastrostomy, EUS-guided biliary access and anterograde stent placement, and EUS-guided rendezvous approach to gain biliary access followed by ERCP, and eventually interventional radiology-guided percutaneous biliary drainage. EUS-guided rendezvous approach in patients with Whipple procedure has been reported for pancreatic duct access but is not often described in the literature to obtain biliary access. The advantage of this approach over EUS hepaticogastrostomy is the better safety profile. According to studies, EUS-guided hepaticogastrostomy has variable adverse events rates typically in the 10-30% range [6, 7]. Compared to anterograde stent placement via EUS, this approach is safer, because there is no need for dilation of the gastric wall tract and puncture site into the biliary tree, and less chance for stent mal-deployment since the stent is deployed under endoscopic guidance. EUS-guided rendezvous should be considered in instances when the afferent limb is reached easily but the hepaticojejunostomy cannot be identified due to significant stricturing as was the case in our report. Lastly, while we used EUS-guided rendezvous for malignant obstruction, EUS rendezvous should be the preferred approach in patients with benign disease because EUS-guided hepaticogastrostomy and anterograde stent placement are only indicated in malignant disease. Another approach in these situations could be using a forward viewing echoendoscope and approach the biliary tree closer to the hepaticojejunal anastomosis; however, the forward viewing echoendoscope is not widely available across the USA [8].
In this case we were also able to use the modified therapeutic endoscope, which allowed for a significant advantage in manipulating the scope as opposed to a longer and more cumbersome colonoscopes or balloon enteroscope. In patients with pancreaticoduodenectomy or other surgical alterations with short afferent limbs, a modified therapeutic endoscope may be a reasonable alternative to colonoscopes or balloon enteroscopes, and can allow for more maneuverability leading to a greater chance of successful cannulation.
One notable disadvantage of using a forward viewing endoscope as opposed to a duodenoscope is difficulty in cannulating due to tangential view of the papilla or biliary anastomosis [4]. Wang et al in their study were able to demonstrate a modest increase in successful cannulation when using a clear distal attachment plastic cap fitted to the scope [9]. This was another technique successfully utilized in gaining biliary access in this case. The hepaticojejunal anastomosis is typically identifiable with a forward viewing scope; however, in cases of stenosis like in the described case it can become substantially more difficult to identify the anastomosis, and use of a cap can potentially assist in this scenario. Another challenge that is posed by using a standard gastroscope or balloon enteroscope is the inability to pass the majority of accessories needed during the ERCP down the narrower working channel; use of a modified therapeutic endoscope offers the ability to utilize a wider array of ERCP devices, ultimately allowing for deployment of an uncovered metal stent in this case.
There have been several cases published in the literature of endoscopic retrograde pancreatography (ERP) or pancreatic ERCP. Endoscopic access of the pancreatic duct in these patients often presents similar challenges as to biliary access. A commonly described technique in these cases has been the EUS rendezvous technique. Itoi et al demonstrated two cases of successful pancreatic duct stent placement using an EUS-guided rendezvous approach and single balloon enteroscopy in post-pancreaticoduodenectomy patients [10]. In the publication of Mallery et al of their experience with EUS rendezvous in 2004, two of the described cases involved pancreatic duct access using an EUS rendezvous technique [3]. Kinney et al described attempted ERCP in 10 patients after pancreaticoduodenectomy, unassisted successful cannulation of the pancreatic duct, and therapy was achieved in only one patient. In the remaining nine patients either percutaneous or EUS-guided rendezvous techniques were required to achieve successful therapeutic intervention [11]. However, the use of EUS rendezvous for biliary access in patients with prior Whipple surgery has not been reported.
In this case several techniques were employed to allow for successful completion of the procedure and therapeutic intervention. Use of a shorter endoscope with a clear distal attachment plastic cap allowed for greater maneuverability of the endoscope, better positioning and better visualization of the biliary anastomosis. In addition, the modified therapeutic endoscope with a wider working channel allowed for use and deployment of an uncovered mental stent across the strictured hepaticojejunostomy. Finally, use of the EUS rendezvous technique allowed for visualization and access of a difficult to locate stenosed hepaticojejunostomy. Some or all of these techniques in combination can be utilized to increase successful engagement of the biliary tree in patients with post-surgical anatomy and allow for a high rate of successful therapeutic intervention.
Learning points
Use of a therapeutic upper endoscope can allow for therapeutic interventions using standard ERCP catheters, additional the shorter length of the endoscope allows for more maneuverability and stability. Addition of a clear plastic cap to the end of the endoscope can further augment stability and positioning relative to the biliary anastomosis. The EUS rendezvous technique can significantly increase the success of difficult ERCP in patients with surgically altered anatomy allowing for greater chances of successful therapeutic intervention. If the intra-hepatic biliary tree has been accessed but the guidewire fails to pass into the jejunum, then anterograde stent placement across the hepaticojejunal anastomosis or an EUS-guided hepaticogastrostomy can be considered.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors report no conflict of interest related to this manuscript.
Informed Consent
Informed consent was obtained.
Author Contributions
MA, NM and MB were involved in concept design, drafting, editing and reviewing the manuscript.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Chahal P, Baron TH, Topazian MD, Petersen BT, Levy MJ, Gostout CJ. Endoscopic retrograde cholangiopancreatography in post-Whipple patients. Endoscopy. 2006;38(12):1241-1245.
- Lichtenstein DR. Post-Surgical Anatomy and ERCP. Techniques in Gastrointestinal Endoscopy. 2007;9:114-124.
- Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: Report of 6 cases. Gastrointest Endosc. 2004;59(1):100-107.
- Krutsri C, Kida M, Yamauchi H, Iwai T, Imaizumi H, Koizumi W. Current status of endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. World J Gastroenterol. 2019;25(26):3313-3333.
- Shimatani M, Takaoka M, Tokuhara M, Miyoshi H, Ikeura T, Okazaki K. Review of diagnostic and therapeutic endoscopic retrograde cholangiopancreatography using several endoscopic methods in patients with surgically altered gastrointestinal anatomy. World J Gastrointest Endosc. 2015;7(6):617-627.
- Nakai Y, Sato T, Hakuta R, Ishigaki K, Saito K, Saito T, Takahara N, et al. Long-term outcomes of a long, partially covered metal stent for EUS-guided hepaticogastrostomy in patients with malignant biliary obstruction (with video). Gastrointest Endosc. 2020;92(3):623-631.e621.
- Paik WH, Park DH. Outcomes and limitations: EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2019;8(Suppl 1):S44-S49.
- Iwai T, Kida M, Yamauchi H, Okuwaki K, Kaneko T, Hasegawa R, Watanabe M, et al. EUS-guided transanastomotic drainage for severe biliopancreatic anastomotic stricture using a forward-viewing echoendoscope in patients with surgically altered anatomy. Endosc Ultrasound. 2021;10(1):33-38.
- Wang F, Xu B, Li Q, Zhang X, Jiang G, Ge X, Nie J, et al. Endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: One single center's experience. Medicine (Baltimore). 2016;95(52):e5743.
- Itoi T, Kikuyama M, Ishii K, Matsumura K, Sofuni A, Itokawa F. EUS-guided rendezvous with single-balloon enteroscopy for treatment of stenotic pancreaticojejunal anastomosis in post-Whipple patients (with video). Gastrointest Endosc. 2011;73(2):398-401.
- Kinney TP, Li R, Gupta K, Mallery S, Hunter D, Jensen E, Vickers S, et al. Therapeutic pancreatic endoscopy after Whipple resection requires rendezvous access. Endoscopy. 2009;41(10):898-901.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


