| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 8, August 2022, pages 365-368
Severe Tricuspid Stenosis Secondary to Permanent Pacemaker Lead
Asif Khana, Ahmad Mustafaa, c, Joanne Linga, James Laffertyb
aDepartment of Medicine, Staten Island University Hospital, Staten Island, NY 10305, USA
bDepartment of Cardiology, Staten Island University Hospital, Staten Island, NY 10305, USA
cCorresponding Author: Ahmad Mustafa, Department of Medicine, Staten Island University Hospital, Staten Island, NY 10305, USA
Manuscript submitted January 12, 2022, accepted July 7, 2022, published online August 19, 2022
Short title: TS Due to Permanent Pacemaker Lead
doi: https://doi.org/10.14740/jmc3900
| Abstract | ▴Top |
Tricuspid stenosis (TS) is a rare valvular abnormality and generally associated with mitral stenosis in cases of rheumatic heart disease. TS is now frequently being described in the setting of permanent pacemaker leads, either with or without the presence of infective endocarditis. We describe a case of a female with TS secondary to permanent pacemaker leads in the absence of infective endocarditis being managed during the pre-conception period. She initially had a balloon valvuloplasty done for moderate to severe TS and subsequently conceived and delivered without complications. However, upon being evaluated before her second pregnancy, she was again found to have severe TS. We hypothesize that the presence of permanent pacemaker lead contributed to the development of early restenosis after the first procedure. A repeat balloon valvuloplasty was unsuccessful and she ultimately underwent successful tricuspid valve replacement with no echocardiographic or clinical signs of restenosis years later. The options for management of TS secondary to permanent pacemaker lead include medical management, balloon valvuloplasty (with or without removal of pacemaker lead), or tricuspid valve replacement. Overall, there is a scarcity of data on long-term outcomes of either option making the management challenging.
Keywords: Tricuspid valve stenosis; Pregnancy complications; Cardiovascular; Heart valve diseases; Balloon valvuloplasty
| Introduction | ▴Top |
Tricuspid stenosis (TS) is a rare valvular abnormality and is primarily seen in younger women [1]. It is rarely found as an isolated valvular defect, but rather is a common sequela of rheumatic heart disease and is generally associated with mitral stenosis [2, 3]. Other less frequent causes of TS include carcinoid syndrome, vegetations due to infective endocarditis, systemic conditions like systemic lupus erythematosus and antiphospholipid antibody syndrome, metastatic tumors, radiation therapy and congenital abnormalities such as atresia or stenosis [1-3]. TS leads to an elevated right atrial pressure due to a pressure gradient between the right atrium and ventricle. Due to elevated right sided pressures, patients with TS frequently present with signs of right heart failure, including fatigue and exertional syncope. Hepatic congestion and ascites causing abdominal discomfort, and lower extremity edema can also be seen in severe cases of TS [1].
The passage of permanent pacemaker lead through the tricuspid valve has been known to be associated with tricuspid regurgitation and stenosis [4]. Initially, it was observed in the setting of endocarditis associated with permanent pacemaker lead [5]. The presence of vegetation due to endocarditis would lead to tricuspid regurgitation, and rarely to TS [5]. This was known as “functional tricuspid stenosis” [6]. However, since the 1980s, authors have described pacemaker lead-induced TS in the absence of endocarditis [7-9]. The likely underlying mechanism is adherence between the lead and the sub-valvular tissue causing mechanical irritation or fibrosis secondary to leaflet perforation and/or laceration [7, 8]. Occasionally the permanent pacemaker lead forms a loop in the right ventricle which predisposes to adhesions and reactive fibrosis [8, 10-14]. However, cases have been reported of TS with no discernible lead looping or leaflet perforation [15].
During pregnancy, an increase in cardiac output occurs secondary to an increased preload due to a rise in blood volume, reduced afterload due to decline in systemic vascular resistance, and an increased maternal heart rate [16]. This increase in cardiac output during pregnancy can result in cardiac decompensation if concomitant valvular heart disease is present. Presence of TS may lead to overt heart failure and other grave complications including recurrent miscarriages [17]. A patient with multivalvular heart disease having recurrent miscarriages that were solely attributed to presence of TS has been reported [17]. The proposed mechanism was that TS causes low cardiac output which leads to decreased uterine blood flow and impaired venous drainage which ultimately leads to decreased viability of pregnancy [17]. However, the specific impact of isolated TS on pregnancy is still undetermined.
The management of TS is primarily based on observational data and expert opinion due to limited literature. No specific recommendations are available regarding the management of TS in the presence of permanent pacemaker leads. The available options for management of TS secondary to permanent pacemaker lead include medical management, balloon valvuloplasty (with or without removal of pacemaker lead), or tricuspid valve replacement. The common practice includes pre-pregnancy counseling and close monitoring by expert physicians during pregnancy [18]. Here we describe the management and outcomes of a 33-year-old female with pacemaker lead-induced TS, prior to and post pregnancy.
| Case Report | ▴Top |
Investigations
A 33-year-old female presented to the office for prepregnancy counseling. She was complaining of intermittent palpitations associated with dyspnea on exertion. Her past medical history was remarkable for symptomatic congenital complete heart block for which a dual-chamber permanent pacemaker was implanted at the age of 15 years, as well as essential hypertension and asthma. On presentation, she was 100% atrial-sensed ventricular-paced, dual-chamber pacing (DDD) mode. Her vital signs were within normal limits. Her physical exam was significant for grade 3/6 diastolic murmur along the left sternal border. Physical examination was negative for rales/crackles on lung auscultation, peripheral edema, or ascites.
Diagnosis
On transthoracic echocardiogram, the patient had a normal left ventricular function, moderate to severe TS with mild regurgitation, and a tricuspid valve area of 0.88 cm2. The mean gradient across the tricuspid valve was 19.4 mm Hg (Figs. 1, 2). The anterior leaflet of the tricuspid valve seemed to be tethered down by pacing lead. Due to physiological increase in cardiac output during pregnancy, there was concern about severe TS leading to overt failure. Hence, an intervention was deemed necessary prior to conception.
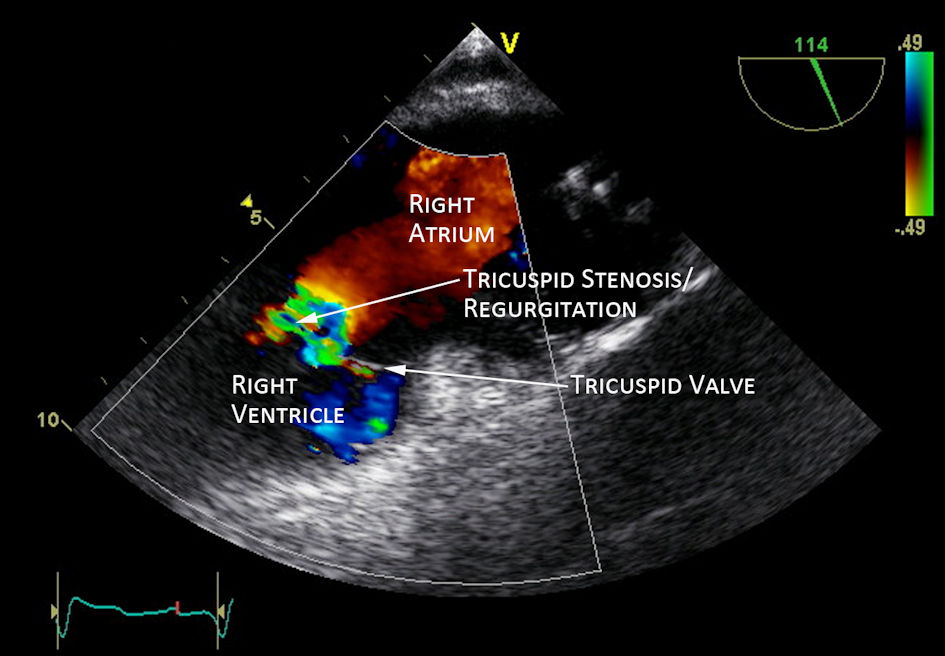 Click for large image | Figure 1. Transthoracic echocardiogram showed tricuspid stenosis and regurgitation (white arrow). |
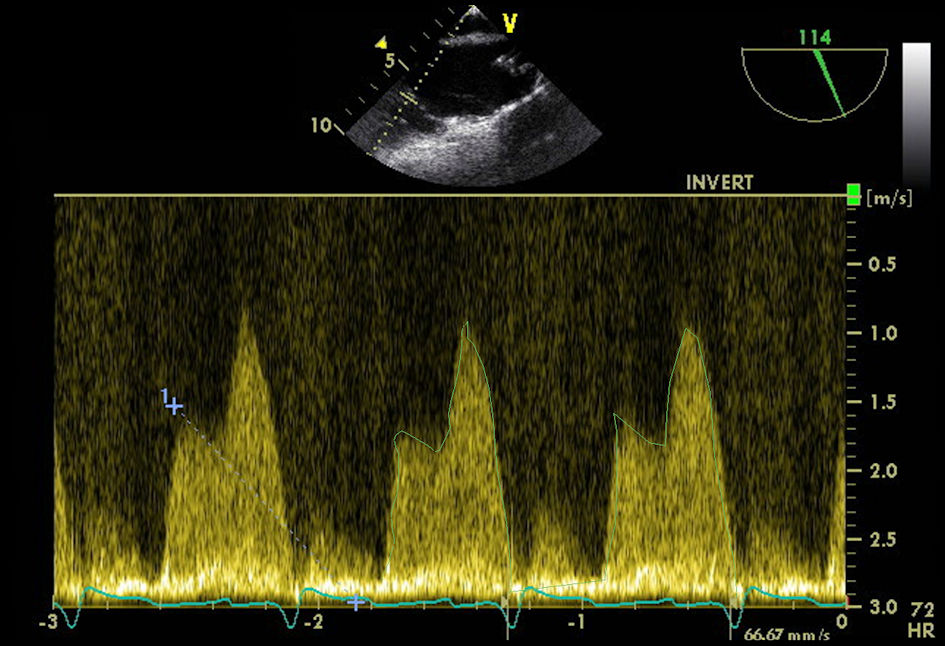 Click for large image | Figure 2. Continuous-wave Doppler showed the mean gradient pressure was 19.4 mm Hg with tricuspid valve pressure half-time 214.29 ms and tricuspid valve area 0.88 cm2. |
Treatment
The patient underwent a successful tricuspid balloon valvuloplasty, and the mean gradient across the tricuspid valve decreased from 19.4 to 5 - 7 mm Hg. There was no change in lead impedances or pacing thresholds after the procedure. Subsequently, patient achieved an uneventful pregnancy with close surveillance. Follow-up echocardiographic findings were stable throughout pregnancy, and she had a normal vaginal delivery at term with no complications.
Follow-up and outcomes
She presented for a routine follow-up 2 years after her valvuloplasty and was found to have elevated impedance and threshold but adequate sensitivity in the right atrial lead. The device was switched from DDD mode to ventricular pacing (VDD) mode which resulted in 100% atrial sensing and 100% ventricular pacing. She presented again 2 more years later with worsening dyspnea on exertion and intermittent palpitations. Repeat echocardiogram showed restenosis of the tricuspid valve with a mean gradient of 14 mm Hg along with a valve area of 0.72 cm2 (Fig. 3). She wanted to conceive again so a repeat balloon valvuloplasty was planned. She underwent balloon valvuloplasty with an 1.8 × 6 cm balloon dilation catheter followed by a 25 mm balloon. However, there was still no change in degree of TS and the mean gradient remained high after the procedure. The case was discussed with cardiothoracic surgery and a tricuspid valve replacement was planned. She underwent successful tricuspid valve replacement with 33 mm Epic valve. During the procedure the right atrial lead was repositioned due to elevated impedance. The right ventricular lead was disconnected, retained, and sewn over and an epicardial ventricular lead was placed. She was able to conceive again and delivered at term with no complications. Repeat echocardiogram 2 years later showed a mean gradient of 5.5 mm Hg across the bioprosthetic tricuspid valve and the patient denied any symptoms of dyspnea or palpitations.
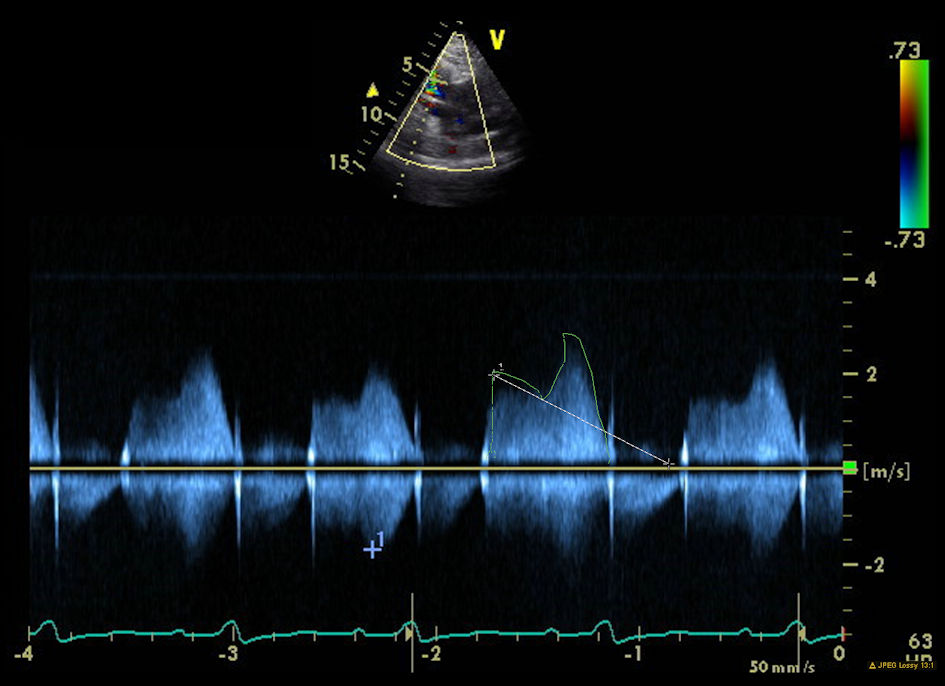 Click for large image | Figure 3. Repeat echocardiogram after 2 more years follow-up showed the mean gradient pressure was 14 mm Hg with tricuspid valve pressure half-time 264 ms and tricuspid valve area 0.72 cm2. |
| Discussion | ▴Top |
Our patient had moderate to severe TS secondary to adhesion of the pacemaker lead to the septal leaflet of the tricuspid valve, and wanted to conceive. She underwent balloon valvotomy prior to pregnancy to reduce the risk of complications during pregnancy. The patient attained pregnancy with no complications. However, in the planning of her second pregnancy, the patient underwent balloon valvuloplasty again for tricuspid restenosis that was unsuccessful. It was later followed by tricuspid valve replacement with repositioning of the right atrial and right ventricular leads. We suspect that the presence of permanent pacemaker lead contributed to the development of early restenosis after the first procedure.
Severe TS is classified as a mean pressure gradient of 5 mm Hg or more, inflow time-velocity integral of greater than 60 cm, a pressure half-time (T1/2) of 190 ms or more, and a valve area by continuity equation of 1 cm2 or less [19]. As per European Society of Cardiology Guidelines for the management of valvular heart disease, intervention on the tricuspid valve is usually carried out at the time of intervention on other valves in patients who are symptomatic despite being on medical therapy [2]. Percutaneous balloon tricuspid dilatation has been performed in a few cases but frequently induces significant regurgitation. The choice between valve repair or valve replacement depends on valve anatomy and surgical expertise [2]. For individuals with symptomatic TS and with low to moderate surgical risk, tricuspid valve surgery is recommended over balloon valvotomy alone [18]. Overall, there is a scarcity of data on long-term outcomes of either procedure.
The management of TS secondary to permanent pacemaker lead is primarily based on observational data and expert opinion. Medically, patients with symptomatic TS, including those with lower extremity edema and hepatic congestion can be treated with loop diuretics but efficacy is limited in the long term [2]. Cases have been described where TS was successfully treated with percutaneous tricuspid valvuloplasty without the removal of the permanent pacemaker lead [10]. Other options for management include permanent pacemaker lead removal with tricuspid valve replacement or permanent pacemaker lead removal with valvuloplasty [10]. Data regarding tricuspid balloon valvotomy outcomes and studies comparing balloon valvotomy with valve surgery in the presence of permanent pacemaker lead is limited. A recent meta-analysis describes the management of mitral stenosis in pregnancy guided by the Wilkins score and the severity of sub-valvular disease [20]. However, no similar score or studies are available to help in the management of TS. Overall, there is a lack of data on long-term results on any form of medical or surgical interventions for management isolated TS, especially when permanent pacemaker is present.
To our knowledge, we presented the only case highlighting the management of pacemaker lead-induced TS prior to pregnancy. The limitation to our case is that the management may not be generalizable. More studies are needed to help further guide TS management especially in this patient population. In our opinion, patients with moderate to severe TS secondary to pacemaker leads would likely benefit from tricuspid valve replacement compared to balloon valvuloplasty as the possibility of later restenosis of the valve is very high. Leaving the permanent pacemaker lead in place further increases the possibility of restenosis in case of balloon valvuloplasty. We conclude that more data is needed in this regard especially considering the increased use of permanent pacemakers.
Learning points
Clinicians may consider that patients with moderate to severe TS secondary to pacemaker leads may likely benefit more, prior to conceiving, from a tricuspid valve replacement compared to balloon valvuloplasty. Balloon valvuloplasty alone while leaving the PPM lead in place may lead to high possibility of restenosis.
Acknowledgments
The authors have no acknowledgments to declare.
Financial Disclosure
The authors have no financial disclosures to declare.
Conflict of Interest
No conflict of interest was reported among authors.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
Ahmad Mustafa and Asif Khan drafted the case report and conducted the necessary supportive literature review. JL and JL reviewed and revised the manuscript. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
TS: tricuspid stenosis
| References | ▴Top |
- Golamari R, Bhattacharya PT. Tricuspid stenosis. In: StatPearls. Treasure Island (FL), 2022.
- Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739-2791.
doi pubmed - Asmarats L, Taramasso M, Rodes-Cabau J. Tricuspid valve disease: diagnosis, prognosis and management of a rapidly evolving field. Nat Rev Cardiol. 2019;16(9):538-554.
doi pubmed - Hagers Y, Koole M, Schoors D, Van Camp G. Tricuspid stenosis: a rare complication of pacemaker-related endocarditis. J Am Soc Echocardiogr. 2000;13(1):66-68.
doi - Unger P, Clevenbergh P, Crasset V, Selway P, Le Clerc JL. Pacemaker-related endocarditis inducing tricuspid stenosis. Am Heart J. 1997;133(5):605-607.
doi - Aboukhoudir F, Boulet V, Rekik S, Pansieri M. [Lead-related infective endocarditis with massive vegetation causing severe functionnal tricuspid stenosis]. Ann Cardiol Angeiol (Paris). 2017;66(5):326-329.
doi pubmed - Uijlings R, Kluin J, Salomonsz R, Burgmans M, Cramer MJ. Pacemaker lead-induced severe tricuspid valve stenosis. Circ Heart Fail. 2010;3(3):465-467.
doi pubmed - Taira K, Suzuki A, Fujino A, Watanabe T, Ogyu A, Ashikawa K. Tricuspid valve stenosis related to subvalvular adhesion of pacemaker lead: a case report. J Cardiol. 2006;47(6):301-306.
- Cassagneau R, Jacon P, Defaye P. Pacemaker lead-induced severe tricuspid valve stenosis: complete percutaneous extraction under extracorporeal life support. Europace. 2013;15(9):1248.
doi pubmed - Hussain T, Knight WB, McLeod KA. Lead-induced tricuspid stenosis - successful management by balloon angioplasty. Pacing Clin Electrophysiol. 2009;32(1):140-142.
doi pubmed - Old WD, Paulsen W, Lewis SA, Nixon JV. Pacemaker lead-induced tricuspid stenosis: diagnosis by Doppler echocardiography. Am Heart J. 1989;117(5):1165-1167.
doi - Heaven DJ, Henein MY, Sutton R. Pacemaker lead related tricuspid stenosis: a report of two cases. Heart. 2000;83(3):351-352.
doi pubmed - Rama-Merchan JC, Arribas-Jimenez A, Martin-Moreiras J, Garcia-Fernandez E, Cruz-Gonzalez I. Pacemaker lead-related tricuspid stenosis successfully treated with percutaneous balloon valvuloplasty guided by 3D echocardiography. Rev Port Cardiol. 2014;33(11):739.e731-733.
doi pubmed - Skoric B, Baricevic Z, Brida M, Samardzic J, Jurin H, Milicic D. Dynamic tricuspid valve stenosis induced with a pacemaker lead: a case report. J Heart Valve Dis. 2014;23(1):142-144.
- Rosenberg Y, Myatt JP, Feldman M, Carpenter AJ, Bauch T, Restrepo CS, Panday M. Down to the wire: tricuspid stenosis in the setting of multiple pacing leads. Pacing Clin Electrophysiol. 2010;33(5):e49-52.
doi pubmed - Robson SC, Hunter S, Boys RJ, Dunlop W. Serial study of factors influencing changes in cardiac output during human pregnancy. Am J Physiol. 1989;256(4 Pt 2):H1060-1065.
doi pubmed - Gamra H, Betbout F, Ayari M, Addad F, Jarrar M, Maatouk F, Ben Farhat M. Recurrent miscarriages as an indication for percutaneous tricuspid valvuloplasty during pregnancy. Cathet Cardiovasc Diagn. 1997;40(3):283-286.
doi - Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, 3rd, Guyton RA, O'Gara PT, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):2440-2492.
doi pubmed - Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009;22(1):1-23; quiz 101-102.
doi pubmed - Sreerama D, Surana M, Moolchandani K, Chaturvedula L, Keepanasseril A, Keepanasseril A, Pillai AA, et al. Percutaneous balloon mitral valvotomy during pregnancy: A systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2021;100(4):666-675.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


