| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 10, October 2022, pages 504-508
The Management of Traumatic Abdominal Wall Flank Hernia Along the Spigelian Aponeurosis Using Component Separation, Synthetic, and Biological Mesh
Aldin Malkoca, d , Kerry E. Finea, Ramisa Anjuma, b, Joseph Vivian Davisa, b, c
aDepartment of Surgery, Arrowhead Regional Medical Center, Colton, CA, USA
bDepartment of Medicine, St. George’s University School of Medicine, True Blue, Grenada
cDepartment of Surgery, California University of Science and Medicine, Colton, CA, USA
dCorresponding Author: Aldin Malkoc, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted September 7, 2022, accepted October 17, 2022, published online October 31, 2022
Short title: Traumatic Abdominal Wall Flank Hernia Repair
doi: https://doi.org/10.14740/jmc4006
| Abstract | ▴Top |
Blunt abdominal trauma is associated with a variety of medical complications. Traumatic abdominal wall hernias (TAWHs) are a rare sequela of blunt trauma. Of the various forms of TAWH, a rare subtype described as a “spontaneous lateral ventral hernia” or flank hernia occurs in less than 1% of all blunt abdominal traumas. We present a case of a 39-year-old male with a past medical history of epilepsy who was involved in a rollover motor vehicle collision. It was reported that the patient had a seizure while driving. On physical exam, the patient had a large left lower flank contusion. Computed tomography revealed a complex TAWH with complete avulsion of the abdominal wall musculature from the iliac crest and near to total disruption of the internal oblique. To address this, we used a biological mesh inlay, reinforced with a synthetic Ventralight™ mesh secured to the iliac crest. In this article, we describe the patient’s experience and management of a complex TAWH.
Keywords: Flank hernia; Traumatic abdominal wall hernia; Blunt abdominal trauma
| Introduction | ▴Top |
Rarely hernias are considered a primary concern in the setting of blunt abdominal trauma. Traumatic abdominal wall hernias (TAWHs) are some of the most infrequent occurring hernias overall [1]. TAWH can occur along any segment of the abdomen. A rare subtype is the traumatic abdominal wall flank hernia (TAWFH) along the spigelian fascia, which occurs in less than 1% of all blunt abdominal traumas [1, 2]. The spigelian fascia is located in the anterior abdominal wall adjacent to the semilunar line and lateral to the rectus abdominis muscle and is formed by the fusion of the internal oblique aponeurosis and transversus abdominis aponeurosis [3]. Flank hernia injuries in this location are often associated with motor vehicle collision (MVC) with deceleration forces, increased intra-abdominal pressure, and the naturally weaker spigelian fascia [2].
There are various treatment options for TAWFH; however, no clear standardized surgical approach has been identified. Difficulties in treating these conditions are providing enough exposure to identify the full extent of the damaged structures and ultimately closure of a large abdominal injury [4]. Currently, the main recommendation is urgent repair using either an open laparotomy, direct incision over the defect, or laparoscopic approach with either mesh or primary closure [4]. In this study, we present a challenging case involving a TAWFH which occurred in a patient after an MVC. The patient developed a hernia at the location of the spigelian fascia with also completely torn abdominal oblique and transversus abdominis from the iliac crest attachment, thus requiring a unique definitive closure utilizing component separation, biological mesh, and synthetic Ventralight™ mesh.
| Case Report | ▴Top |
Investigations
A 39-year-old male with a past medical history of epilepsy was brought in by ambulance after being involved in a rollover MVC. The patient reportedly experienced a seizure while driving, which led to the MVC. On arrival to the trauma bay, the patient complained of abdominal pain and left lower extremity pain. The patient was neurologically intact with a Glasgow coma scale (GCS) of 15 and his initial vital signs were significant for hypotension with a systolic blood pressure below 80 mm Hg. Extended focused assessment with sonography for trauma (e-FAST) was negative for any intraabdominal or intrathoracic bleeding. During the primary trauma survey, a malrotated left ankle along with an absent left dorsalis pedis pulse and a large left lower flank contusion was discovered (Fig. 1). The patient’s left ankle was reduced by orthopedic surgery with return of palpable pulses. The patient’s blood pressure was stabilized with 2 units of packed red blood cells (pRBCs) and a 2 L crystalloid bolus.
 Click for large image | Figure 1. Ecchymosis noted on the patient’s left flank and hip. |
Diagnosis
The complete blood cell count (CBC) showed a leukocytosis of 17.6 × 109/L, hemoglobin of 11.5 g/dL, and platelets of 229 × 109/L. Basic metabolic panel was within normal limits except a chloride of 114 mEq/L and a carbon dioxide of 19 mEq/L. Coagulation tests showed a prothrombin time of 15.3, international normalized ratio of 1.2, and partial thromboplastin time of 29.4. A urine drug screen (Roche Diagnostics Indianapolis, IN) was positive for amphetamine. Computed tomography (CT) of the abdomen, pelvis, and bilateral lower extremity with intravenous contrast (IV) was notable for a left lateral abdominal wall hematoma, left lateral abdominal hernia (Fig. 2), comminuted left distal femur fracture, left fibula fracture, a left fifth metatarsal fracture, and three vessel runoffs of bilateral lower extremities without any noted vascular injuries. The patient was admitted to the surgical intensive care unit (SICU) for hemodynamic monitoring.
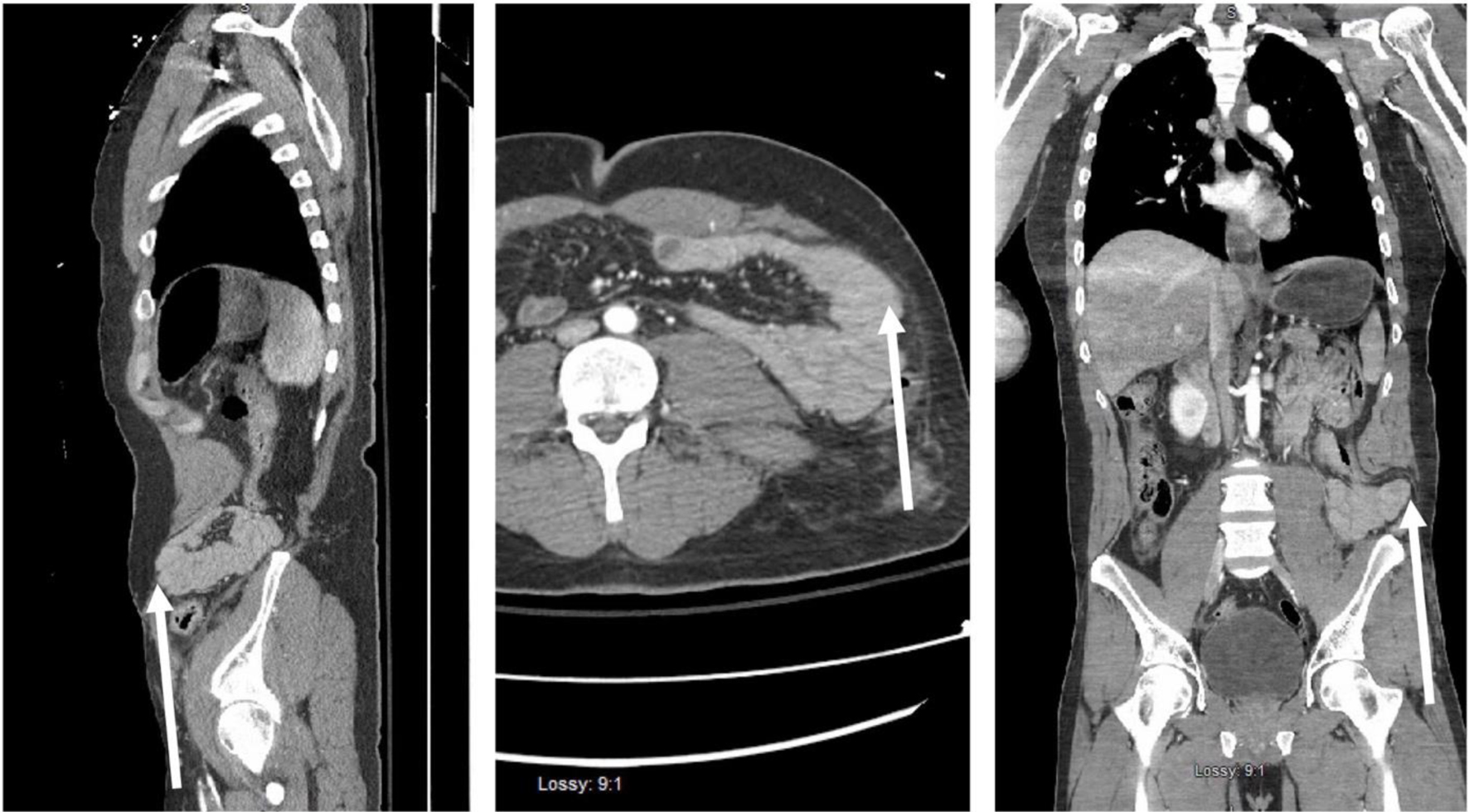 Click for large image | Figure 2. Sagittal, transverse, and coronal computed tomography of abdomen showing disruption of left abdominal wall musculature from iliac crest and retraction of the muscle noted by a white arrow in the three figure segments. |
Treatment
On hospital day 2, the patient underwent an open reduction and internal fixation (ORIF) of the left distal femur. He returned postoperatively to the SICU for continued close hemodynamic monitoring. The patient was taken back to the operating room on hospital day 3 for a left abdominal wall component separation and complex TAWFH repair. An incision was made over the defect and the external oblique was divided lateral to the linea semilunaris, then vertically and separated from the internal oblique. While providing adequate exposure, the team noted that there was complete tearing of the abdominal obliques from the iliac crest with near to total disruption of the internal oblique. The underlying bowel contents were examined and noted to be intact without any injury. The complete obliteration of the left lateral wall provided additional difficulty with the repair. A biological mesh inlay was used to bridge the transversus abdominis to iliac crest to recreate the visceral sac as shown in Figure 3a. This was performed by drilling two holes in the iliac crest in order to affix the muscle and mesh. Then, a Ventralight™ mesh was secured to the internal oblique and iliac crest. A counter incision was required for access to the retracted abdominal wall musculature, as shown in Figure 3b, c. Lastly, the internal oblique muscle was re-approximated over the mesh repair as shown in Figure 3d. The patient left the operating room in stable condition with an abdominal binder in place. Postoperatively, antibiotics were discontinued and his WBC was 11,800 µL.
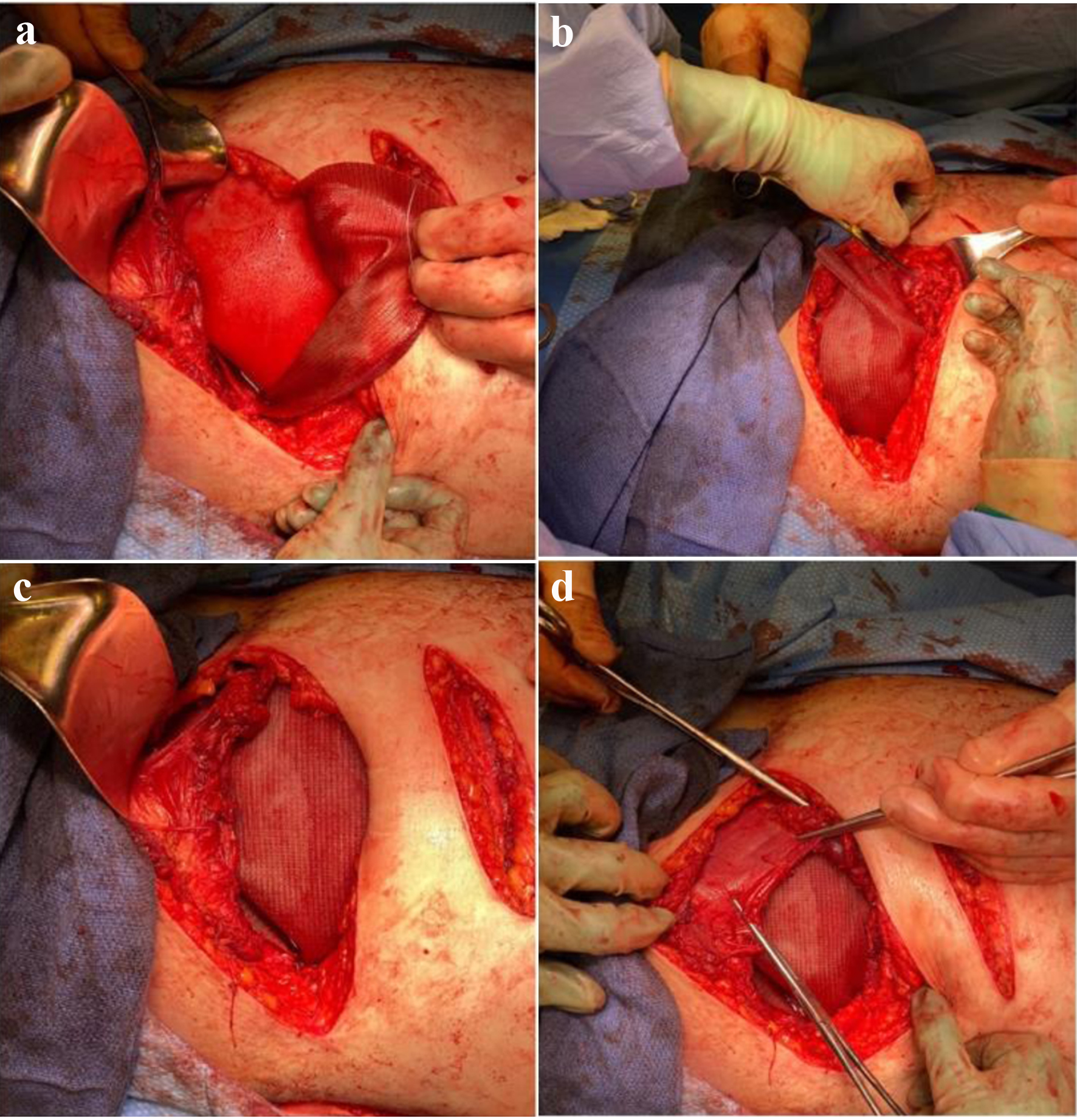 Click for large image | Figure 3. (a) Biological mesh inlay bridging transversus abdominis to iliac crest to recreate visceral sac. (b) Ventralight™ mesh underlay secured to internal oblique and iliac crest. (c) Counter incision visualized for access to retracted abdominal wall musculature. (d) Re-approximation of internal oblique muscle over mesh repair. |
The patient was advanced to a regular diet by hospital day 6. On hospital day 7, the patient was noted to have an ileus along with an increased WBC of 21,900 µL, cough, and fever. A CT of chest without IV contract was suggestive of lobular pneumonia and sputum cultures showed growth of methicillin-resistant Staphylococcus aureus (MRSA). The patient was started on IV vancomycin.
Follow-up and outcomes
On hospital day 8 during daily dressing changes, serous fluid was noted to be draining from his hernia repair incision which also had increased tenderness. These findings were consistent with a seroma, and due to the absence of incision site warmth, erythema, edema, or purulence and a normalizing WBC, no additional antibiotics were initiated. By hospital day 12, drainage from the seroma site had ceased and by hospital day 19, the patient was discharged. The patient was working with physical and occupational therapy with significant improvement; however, he decided to leave against medical advice. At departure, there were no documented complaints related to his left abdominal surgical site and his ileus had resolved with normal bowel function.
| Discussion | ▴Top |
Development of TAWFH is an important consideration in blunt abdominal trauma. Blunt abdominal trauma transiently increases intra-abdominal pressures and allows for herniation through the spigelian fascia along with disruption of abdominal wall musculature [2]. Diagnosis of such an injury can be difficult as some patients are asymptomatic while others complain of dull abdominal pain with a mild bulge [5]. Often, it is difficult to find physical evidence of TAWFH on primary or secondary trauma survey. This highlights the importance of radiological imaging. Abdomen and pelvis CT scan allows for visualization of abdominal wall defects and provides information on size, location, and the presence of any neighboring structural damage [6]. Our radiographic images demonstrate the complete avulsion of the abdominal wall musculature from the iliac crest which confirmed the presence of TAWFH versus other differential diagnoses related to the presence of ecchymosis on exam.
In the setting of TAWFH, open hernia repair is recommended, although laparoscopic repairs have been reported in literature [2]. Open repair is recommended due to the possibility of coexisting structural damage that requires prompt visualization and expeditious repair [7]. In our case, an open approach with incisions directly overlying the defect was necessary due to the mechanism of injury, large disruption of left lateral abdominal musculature, and strong suspicion for concurrent intra-abdominal injuries. Upon opening the abdomen, we noted the extent of damage to the abdominal wall musculature. Primary repair with a combination of biological and synthetic mesh was necessary. While mesh repair is recommended regardless of open or laparoscopic technique, the large abdominal disruption in our patient warranted combination of biological and synthetic mesh [8]. Biological meshes provide the benefit of bridging abdominal wall defects and are less prone to infection, enterocutaneous fistula formation, and adhesion formation; however, they confer less mechanical support than synthetic counterparts [9, 10]. In this case, we used a combination of both biological mesh and synthetic Ventralight ST mesh. The biological mesh provided a bridge between the avulsed transversus abdominis and iliac crest attachment as well as a bolster for the overlying repaired internal oblique and synthetic mesh. The Ventralight ST mesh provided tensile strength to the repair to reduce the risk of future recurrence.
While our patient did not experience re-herniation during his acute hospital stay, he did develop a seroma over the incision site, without any clinical signs of infection. In future repairs, we would consider placement of a drain to prevent seroma formation. The patient was initially on IV vancomycin for MRSA pneumonia and no additional antibiotics were initiated for the seroma. The seroma spontaneously drained through the stapled closure by hospital day 12. Aside from the seroma, our patient’s postoperative course had no further complications related to the hernia repair.
A diagnosis of TAWSH is difficult and often requires three-dimensional imaging to accurately visualize the underlying hernia. More importantly, repair of the hernia is warranted to prevent future bowel strangulation. From our isolated case, we recommend utilizing a biological mesh in large muscular avulsions overlayed with a synthetic mesh for increased support as compared to the more common single mesh approach.
Learning points
While TAWSHs are rare, they can be a significant cause of morbidity related to the possibility of visceral strangulation. There is no standardized method of repair and few studies have reported using a combination of biological and synthetic mesh. In our presented case, the use of a biological mesh inlay, reinforced with a synthetic Ventralight™ mesh, offers an alternative approach to the management of a complex TAWSH.
Acknowledgments
The authors would like to thank and express their gratitude to the wonderful Arrowhead Regional Medical Center operating room staff, emergency department trauma staff, and the Surgical Intensive Care Unit exceptional nursing staff for their expert clinical support.
Financial Disclosure
The research presented in this manuscript had no specific funding from any agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Informed consent was obtained from the patient for publication of this case report and accompanying images. This was approved by the Arrowhead Regional Medical Center IRB committee (CS #22-11).
Author Contributions
Aldin Malkoc, MD’s contributions include manuscript writing, editing, and conducting the literature review. Kerry Fine, DO’s contributions include managing the patient and reviewing and revising the manuscript. Ramisa Anjum, BS’ contributions include manuscript writing, editing, and literature review. Vivian Davis, DO, JD’s contributions include attending the patient and reviewing and editing the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
TAWH: traumatic abdominal wall hernias; MVA: motor vehicle accident; GCS: Glasgow coma scale; e-FAST: extended focused assessment with sonography for trauma; CT: computed tomography; IV: intravenous contrast; SICU: surgical intensive care unit; ORIF: open reduction and internal fixation; MRSA: methicillin-resistant Staphylococcus aureus
| References | ▴Top |
- Dennis RW, Marshall A, Deshmukh H, Bender JS, Kulvatunyou N, Lees JS, Albrecht RM. Abdominal wall injuries occurring after blunt trauma: incidence and grading system. Am J Surg. 2009;197(3):413-417.
doi pubmed - Wilson KL, Davis MK, Rosser JC, Jr. A traumatic abdominal wall hernia repair: a laparoscopic approach. JSLS. 2012;16(2):287-291.
doi pubmed - Mittal T, Kumar V, Khullar R, et al. Diagnosis and management of Spigelian hernia: A review of literature and our experience. J Minim Access Surg. 2008;4(4):95-98.
doi pubmed - Webber V, Low C, Skipworth RJE, Kumar S, de Beaux AC, Tulloh B. Contemporary thoughts on the management of Spigelian hernia. Hernia. 2017;21(3):355-361.
doi pubmed - Moreno-Egea A, Campillo-Soto A, Morales-Cuenca G. Which should be the gold standard laparoscopic technique for handling Spigelian hernias? Surg Endosc. 2015;29(4):856-862.
doi pubmed - Cabry RJ, Jr., Thorell E, Heck K, Hong E, Berkson D. Understanding noninguinal abdominal hernias in the athlete. Curr Sports Med Rep. 2014;13(2):86-93.
doi pubmed - Drago SP, Nuzzo M, Grassi GB. Traumatic ventral hernia: report of a case, with special reference to surgical treatment. Surg Today. 1999;29(10):1111-1114.
doi pubmed - Zhou DJ, Carlson MA. Incidence, etiology, management, and outcomes of flank hernia: review of published data. Hernia. 2018;22(2):353-361.
doi pubmed - Elghali MA, Nasri S, Seghaier A, Dhouioui K, Hamila F, Youssef S, Letaief R. Unusual complication of seroma after ventral hernia mesh repair: Digestive perforation by tacks. A case report. Int J Surg Case Rep. 2018;53:151-153.
doi pubmed - Sailes FC, Walls J, Guelig D, Mirzabeigi M, Long WD, Crawford A, Moore JH, Jr., et al. Synthetic and biological mesh in component separation: a 10-year single institution review. Ann Plast Surg. 2010;64(5):696-698.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


