| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 3, March 2023, pages 95-99
Fracture Neck of the Femur: A Case of Two Pathologies
Mohamed H. Ahmeda, b, f, Shravani Joshic, Amirmohammad Heidaric, Oliver Pearced, Maria Panourgiab, Henry Owlesb, Moez Dungarwallae
aDepartment of Medicine and HIV Metabolic Clinic, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
bDepartment of Geriatric Medicine, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
cThe Medical School, University of Buckingham, Buckingham, Buckinghamshire, UK
dDepartment of Trauma and Orthopaedics, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
eDepartment of Haematology, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
fCorresponding Author: Mohamed H. Ahmed, Department of Medicine and HIV Metabolic Clinic, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
Manuscript submitted January 30, 2023, accepted March 14, 2023, published online March 31, 2023
Short title: Fracture Neck of the Femur
doi: https://doi.org/10.14740/jmc4055
| Abstract | ▴Top |
We report a case of a 65-year-old woman who sustained a left neck of femur (NOF) fracture following low-energy trauma. Computed tomography (CT) scan for the neck, chest, abdomen and pelvis was normal apart from enlargement of the right lobe of the thyroid. Interestingly, thyroid function was normal. While waiting for the result of thyroid cytology and bone histology, the patient recovered well from the operation and started to engage well with physiotherapy. The result of the investigation showed presence of diffuse large B-cell lymphoma in the left NOF and right lobe of the thyroid. As the presence of lymphoma only in these two organs is extremely rare, it is not yet clear what is underlying mechanism for such association. Therefore, such observations may raise many future research questions as detailed in the discussion of this case report. This case also illustrates the importance of a multidisciplinary approach in identifying, evaluating, and treating unique and complex presentations of NOF fracture, with a focus on the patient’s history, clinical examination and applying diagnostic tools.
Keywords: Neck of femur fracture; Neck of femur malignancies; Malignancy; Clinical examination; Multidisciplinary team
| Introduction | ▴Top |
There is an increasing incidence of neck of femur (NOF) fractures with increasing age [1]. It was estimated that approximately 100,000 patients will need surgical treatment for a fractured NOF by 2033 in England [2]. NOF fractures confer a high morbidity and mortality, with a decreased functional status post-surgically [3]. Atraumatic NOF fractures can be frequently encountered in clinical practice and can be defined as low-energy mechanism of injury producing a fracture. Causes of atraumatic NOF fractures may include stress, insufficiency, fatigue, atypical and pathological fractures. These causes may cause weakening of the bone or impair bone healing, hence leading to reduced integrity and bone strength [1]. It is difficult to evaluate the exact prevalence of pathological fractures due to studies not including histological screening for all NOF fractures; however, one study found nine out of 311 patients to have a pathological fracture as a result of malignancy. Pathological fractures most commonly result from lymphoma, myeloma or metastatic disease of breast and lung being the commonest, followed by renal and prostate [3]. In this case report, the presence of lymphoma was only confined to the left neck of the femur and right lobe of thyroid. Interestingly, the thyroid function for this patient remained within the normal range.
| Case Report | ▴Top |
Investigations
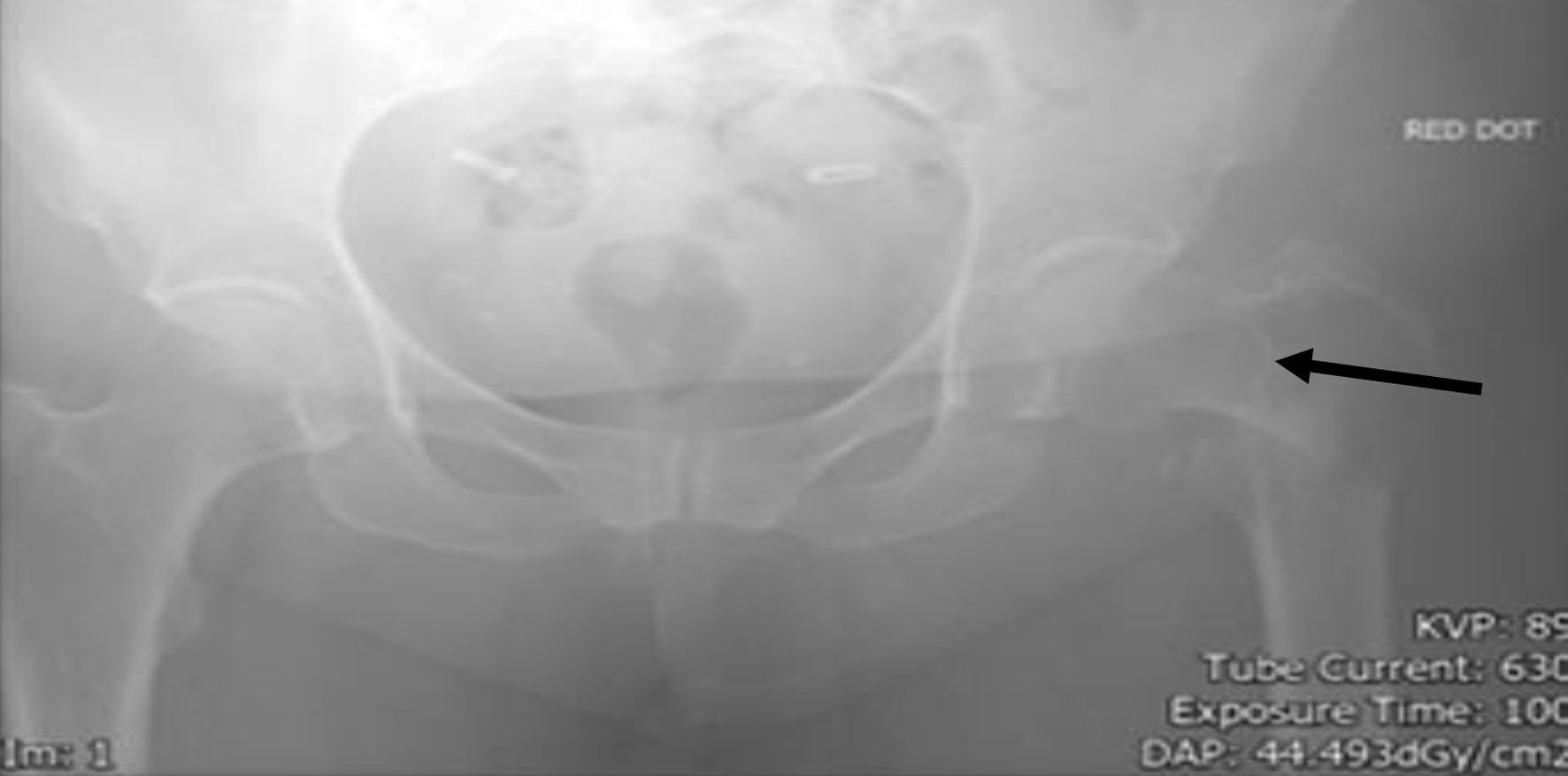
A 65-year-old woman presented to her general practitioner complaining of a 4-week history of left knee pain after which she sustained a fall at the practice and presented to the local accident and emergency (A&E). At the time, she denied any systemic symptoms. The plain radiographs taken in A&E showed no abnormalities, and the patient was discharged home (Fig. 1).
 Click for large image | Figure 1. The pelvic X-ray on admission (no clear evidence of fracture of the left neck of the femur). |
Four days later, she re-presented to A&E, having sustained another fall, with left hip pain. On this occasion, the radiograph showed a basic cervical/intertrochanteric fracture of the left hip. The report stated a lucency in the region of the greater trochanter, which was not visible on the initial radiograph; however, this was attributed to be a potential artefact (Fig. 2).
 Click for large image | Figure 2. The repeat of pelvic X-ray, 4 days after the X-ray in Figure 1. Arrow points to the site of the fracture of the left neck of the femur. |
Her past medical history included hypertension, depression, foot neuropathy of unknown origin, gastric band surgery and severe diverticulosis. She had no significant family history. On investigation, her vitamin D was found to be low 28 nmol/L and adjusted calcium of 2.51 mmol/L, normal thyroid function. The thyroglobulin was high (47.55 µg/L), while dual-energy X-ray absorptiometry (DEXA) scan was normal.
Diagnosis
Her fracture was fixated with an intermedullary nail. Due to a history of multiple presentations with hip pain without any radiological evidence of pathology such as osteoarthritis, the surgeon sent the bone remains for histopathological examination (Fig. 2). The bone sample was found to show para-trabecular infiltrate containing sheets of atypical lymphoid cells with frequent fibrosis and apoptosis. The atypical cells were found to be positive for CD45, CD20, and CD79a, with the Ki67 index being raised. Consequently, a diagnosis of diffuse large B-cell lymphoma was made.
A subsequent computed tomography (CT) of chest, abdomen, and pelvis (CT CAP) identified a “4-cm solid nodule in the lower pole of the right lobe of the thyroid with retrosternal extension causing tracheal displacement” (Fig. 3). However, her thyroid function was found to be unaffected. An ultrasound scan showed a hypoechoic mass with increased vascularity and a fine-needle aspiration of the thyroid mass was suspicious for non-Hodgkin’s lymphoma (NHL). The patient underwent a CT of her left upper leg to evaluate the size of the femoral lesion better. The CT did not find any discrete lesion or mass in the femur. A positron emission tomography (PET) scan was then conducted to identify any insidious areas of malignancy. This showed an intensely avid solitary right thyroid nodule, measuring at 4 × 3.6 cm, displacing the trachea and a surgically fixed pathological left femoral fracture due to intensely avid proven diffuse large B-cell lymphoma (DLBCL) (Fig. 4). The remaining FDG biodistribution and CT appearances were unremarkable.
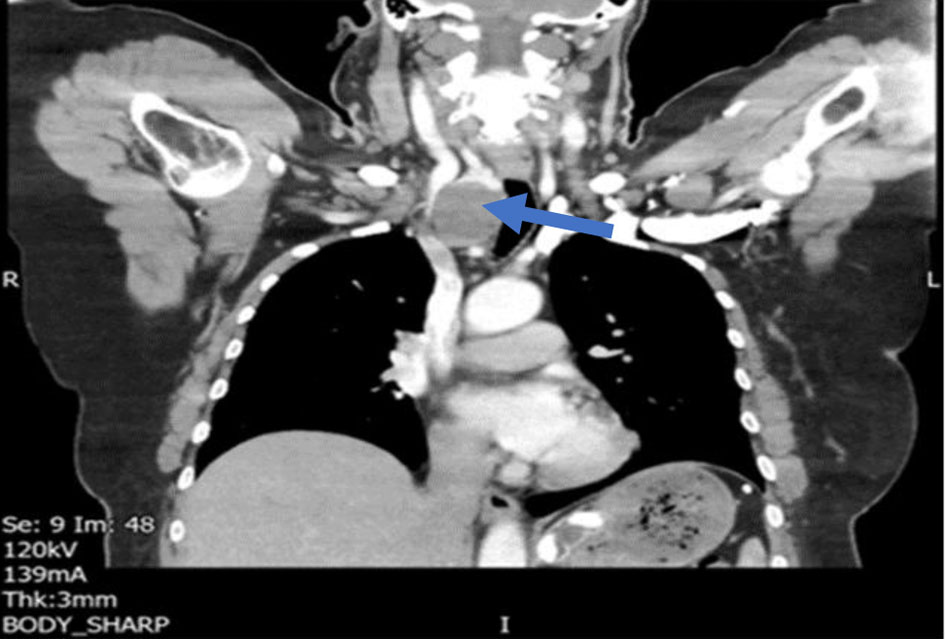 Click for large image | Figure 3. Computed tomography (CT) scan showing the enlargement of the thyroid gland (blue arrow points to the enlarged thyroid). The rest of the CT scan of the neck, abomen and plevis showed no other abnormalities. |
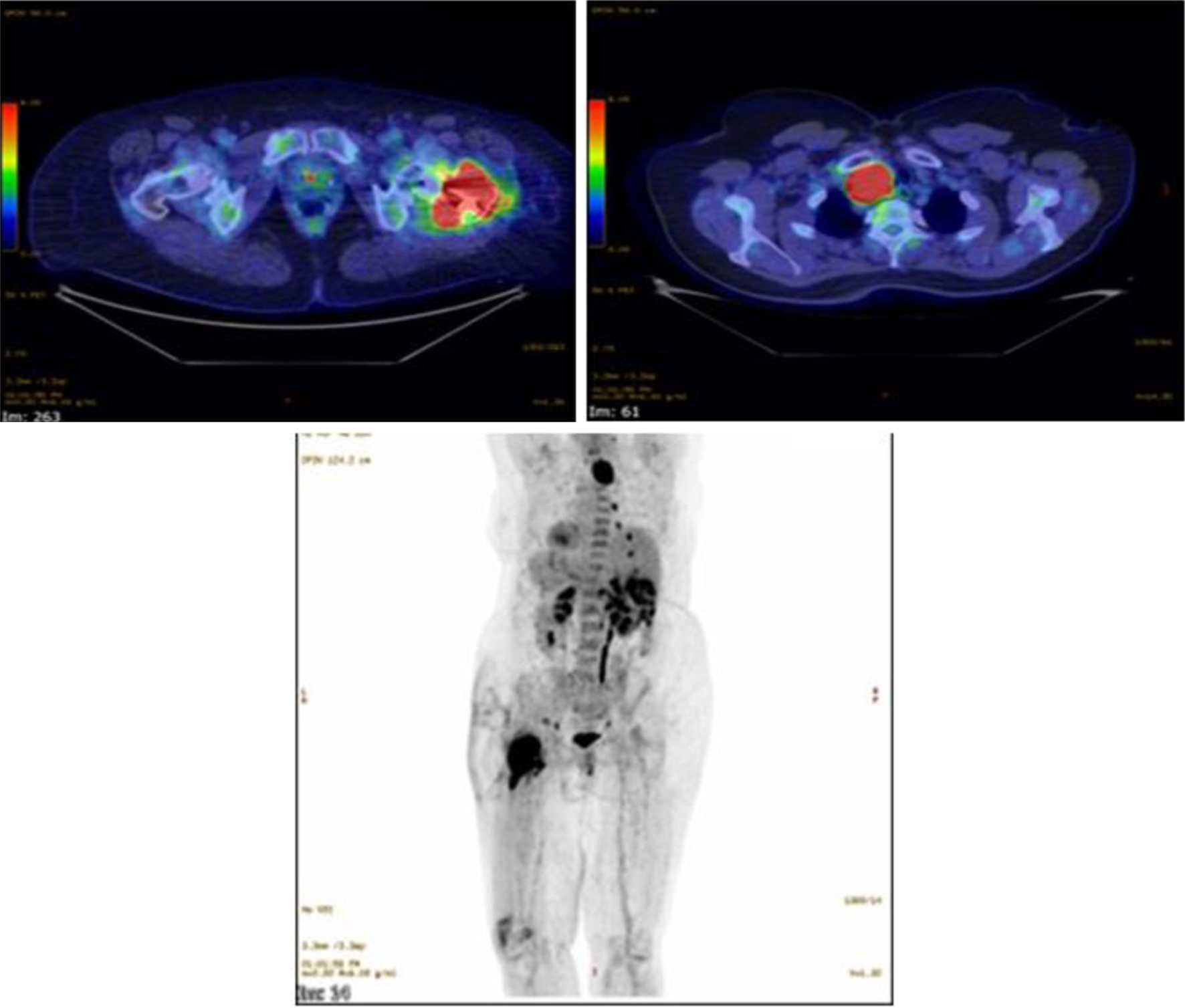 Click for large image | Figure 4. PET scan and high uptake can be seen in the right lobe of thyroid gland. The conclusion of all the investigations: this diffuse B-cell lymphoma is confined to thyroid gland and left neck of the femur. |
Treatment
A diagnosis of stage IV DLBCL was made, and the patient was therefore commenced on systemic chemotherapy regime in a clinical trial of R-CHOP with acalabrutinib, and subsequently was found to be in complete remission.
Follow-up and outcomes
Patient was seen in hematology and orthopedic clinic 3 - 6 months after discharge, and remained well and no further concern was raised. Unfortunately, after 12 months recurrence of lymphoma in the left hip was noted and patient was referred to specialist center for further treatment.
| Discussion | ▴Top |
The B-cell lymphomas result from the malignant proliferation of B cells [4] and are classified into Hodgkin’s lymphoma (HL) and NHL. NHL constitutes about 80% of all lymphomas. NHL is highly heterogeneous, with one of the commonest subtypes being DLBCL [5, 6], accounting for approximately a quarter of all NHLs worldwide [7, 8].
Tumor tissue can affect any organ and system, usually in lymph nodes, and 30-40% of primary DLBCL is mainly in non-lymph nodes organs. Therefore, extra-nodal involvement is prevalent in DLBCL compared to other NHL subtypes [9, 10]. Examples of such extra-nodal involvement can be seen in the gastrointestinal tract, skin and soft tissue, bone, and genitourinary system [11]. Femoral involvement often presents with non-specific symptoms and inconclusive radiographic features which make diagnosis of DLBCL difficult to establish. Patients usually present at a late stage of the disease, with features including bone pain, fractures, swellings, and fevers [12,-14].
It is important to note that in the majority of cases, bony involvement was associated with widespread disseminated disease. Fifty percent of patients with presumed solitary lesions were found to have disease elsewhere upon further investigation [13]. Reported radiographic features usually included lytic lesions [15]. Thyroid lymphoma is classified into primary lymphomas (PTLs) and secondary thyroid lymphomas (STLs). STL affects lymph nodes and other organs first followed by spread to the thyroid later. The incidence of thyroid involvement in patients with lymphoma is approximately 20%; however, these are very rarely clinically overt [16-18]. PTLs are uncommon malignancies, accounting for around 5% of all thyroid cancers [19, 20]. DLBCL is the most common type, with more than half of these cases.
Differentiating PTL from STL can be challenging. A review of the literature reveals that PTL tends to occur in older age group, around 60 years old, and almost exclusively originates in setting of pre-existing thyroiditis. On the contrary, STL more commonly affects middle-aged patients, and presents with disseminated disease and with no evidence of thyroiditis [21]. To our knowledge, there has only been one reported case of DLBCL involving both the femur and thyroid which presented with distal femoral fracture, with imaging revealing lytic lesions in the femur and fibula [22]. Siddiqui et al reported that lymphomas presenting primarily at the proximal femur and proximal humerus are unusual [23]. The pathological association between thyroid, femur bone, cancer and lymphoma is very interesting. For instance, DLBCL of the mandibular bone was incidentally found to be associated with papillary thyroid carcinoma in a case report [24]. Suwardjo et al reported the presence of papillary thyroid cancer with NOF fracture [25]. Evans et al reported a case of primary thyroid lymphoma with bone marrow infiltration at presentation [26].
Such observations may raise many future research questions. 1) How the thyroid gland communicate with neck of the femur during normal physiological conditions; 2) How such communication will change between the two organs in presence of cancer or lymphoma; 3) If these two hypotheses were true, the role of thyroid in bone metabolism may be beyond our current understanding; 4) Interestingly, in our case report, the NOF fracture was in the left while the lymphoma was in the right lobe of the thyroid (it is tempting to describe, is this similar to the control exerted by the right side of the brain in the left side of the body, obviously further research is needed). The lymphoma may have different clinical presentations. For instance, De Vitis et al reported unique case report of a primary B-cell lymphoma causing a pure sensory peripheral neuropathy of the upper limb, that responded to radiotherapy treatment [27].
Conclusions
Our case is unique, as the patient presented with hip pain twice to the hospital, lymphoma in both the femur and thyroid and no clinical features of lymphoma. The case also illustrates the importance of the collaboration between ortho geriatrician, orthopedic surgeons and hematologists in making the diagnosis, treatment and follow-up.
Learning points
NOF fracture following low-energy trauma warrants the need to exclude pathological fracture. Lymphoma of the bone can be confined to the bone or affect other organs as well. The presence of lymphoma of the NOF and one lobe of the thyroid is extremely rare.
Acknowledgments
Shravani Joshi and Amirmohammad Heidari are grateful for their parents for their unlimited support during their study at the Medical School in the University of Buckingham.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
Conception and design: MHA. Administrative support: all authors. Provision of study materials or patients: all authors. Collection and assembly of data: MHA, SJ, and AH. Data analysis and interpretations: all authors. Manuscript writing: all authors. Final approval of manuscript: all authors.
Data Availability
The authors declare that data supporting of this study are available within this study.
| References | ▴Top |
- Hedge G, Thaker S, Botchu R, Fawcett R, Gupta H. Atraumatic fractures of the femur. Br J Radiol. 2021;94(1121):20201457.
doi pubmed pmc - White SM, Griffiths R. Projected incidence of proximal femoral fracture in England: a report from the NHS Hip Fracture Anaesthesia Network (HIPFAN). Injury. 2011;42(11):1230-1233.
doi - Khan S, Wadee N, Burger M, Ferreira N, Jordaan J. Prevalence of pathological neck of femur fractures in patients undergoing arthroplasty at a tertiary referral hospital. SA Orthopaedic Journal. 2021;20(1):16-20.
- Liu Y, Barta SK. Diffuse large B-cell lymphoma: 2019 update on diagnosis, risk stratification, and treatment. Am J Hematol. 2019;94(5):604-616.
doi - Li S, Young KH, Medeiros LJ. Diffuse large B-cell lymphoma. Pathology. 2018;50(1):74-87.
doi - Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107(1):265-276.
doi pubmed pmc - van Leeuwen MT, Turner JJ, Joske DJ, Falster MO, Srasuebkul P, Meagher NS, Grulich AE, et al. Lymphoid neoplasm incidence by WHO subtype in Australia 1982-2006. Int J Cancer. 2014;135(9):2146-2156.
doi - Nowakowski GS, Czuczman MS. ABC, GCB, and double-hit diffuse large B-cell lymphoma: does subtype make a difference in therapy selection? Am Soc Clin Oncol Educ Book. 2015:e449-e457.
doi - Padala SA, Kallam A. Cancer, diffuse large B cell lymphoma [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557796/.
- Shabbir A, Kojadinovic A, Gidfar S, Mundi PS. Extranodal diffuse large B-cell lymphoma of bone and soft tissue presenting with marked lymphedema and hypercalcemia. Cureus. 2022;14(2):e22025.
doi pubmed pmc - Jiang X, Sun M, Liu C. Secondary EBV-positive diffuse large B-cell lymphoma of skeletal muscle from EBV-positive primary diffuse large B-cell lymphoma of thyroid gland: case report and literature review. Austin Journal of Medical Oncology [Internet]. 2021. Available from: https://austinpublishinggroup.com/medical-oncology/fulltext/ajmo-v8-id1057.pdf.
- Ozpolat T, Saka B, Yonal-Hindilerden I, Tascioglu C, Dogan O, Nalcaci M. A misleading presentation of T cell/histiocyte rich B-cell lymphoma mimicking osteomyelitis. Blood Res. 2018;53(3):250-251.
doi pubmed pmc - Choi JY, Hahn JS, Suh CO, Yang WI. Primary lymphoma of bone - survival and prognosis. Korean J Intern Med. 2002;17(3):191-197.
doi pubmed pmc - Olszewski AJ, Kurt H, Evens AM. Defining and treating high-grade B-cell lymphoma, NOS. Blood. 2022;140(9):943-954.
doi - Suzuki Y, Cho Y, Ma T. A case of precursor B-cell acute lymphoblastic leukemia occurred with rapid hip bone destruction and femoral neck fracture. J Clin Case Rep. 2018;8:4.
- Shimaoka K, Sokal JE, Pickren JW. Metastatic neoplasms in the thyroid gland. Pathological and clinical findings. Cancer. 1962;15:557-565.
doi - Li J, Zhou C, Liu W, Sun X, Meng X. Synchronous diffuse large B-cell lymphoma of the stomach and small cell lung carcinoma: A case report. Medicine (Baltimore). 2017;96(50):e8873.
doi pubmed pmc - Silverberg SG, Vidone RA. Adenoma and carcinoma of the thyroid. Cancer. 1966;19(8):1053-1062.
doi - Derringer GA, Thompson LD, Frommelt RA, Bijwaard KE, Heffess CS, Abbondanzo SL. Malignant lymphoma of the thyroid gland: a clinicopathologic study of 108 cases. Am J Surg Pathol. 2000;24(5):623-639.
doi - Thieblemont C, Mayer A, Dumontet C, Barbier Y, Callet-Bauchu E, Felman P, Berger F, et al. Primary thyroid lymphoma is a heterogeneous disease. J Clin Endocrinol Metab. 2002;87(1):105-111.
doi - Foppiani L, Secondo V, Arlandini A, Quilici P, Cabria M, Del Monte P. Thyroid lymphoma: a rare tumor requiring combined management. Hormones (Athens). 2009;8(3):214-218.
doi - McNierney DA, Vazquez B, Shahlapour M, Rahman S, Horani MH. SUN-915 diffuse large B cell lymphoma presents with femur fracture and involvement of thyroid gland. Journal of the Endocrine Society [Internet]. 2020;4(Supplement_1):SUN-915.
- Siddiqui YS, Khan AQ, Sherwani M. Pathological fractures in primary non-Hodgkin's lymphoma of the bone: a case series with review of the literature. J Clin Diagn Res. 2013;7(3):513-517.
doi pubmed pmc - Bosch-Barrera J, Arbea L, Garcia-Velloso MJ, Gil-Bazo I, Garcia-Foncillas J, Panizo C. Primary bone lymphoma of the mandible and thyroid incidentaloma identified by FDG PET/CT: a case report. Cases J. 2009;2:6384.
doi pubmed pmc - Suwardjo S, Avanti WS, Dwianingsih EK, Harahap WA, Anwar SL. Complete diaphysis resorption of the femur: A case report in a metastatic papillary thyroid cancer. Ann Med Surg (Lond). 2020;60:614-618.
doi pubmed pmc - Evans TR, Mansi JL, Bevan DH, Dalgleish AG, Harmer CL. Primary non-Hodgkin's lymphoma of the thyroid with bone marrow infiltration at presentation. Clin Oncol (R Coll Radiol). 1995;7(1):54-55.
doi - De Vitis R, D'Orio M, Fiorentino V, Passiatore M. Primary lymphoma of the medial cutaneous nerve of the forearm: the first case in a pure sensory nerve of the upper limb. BMJ Case Rep. 2022;15(3):e248597.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


