| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 3, March 2023, pages 100-104
Metastatic Squamous Cell Carcinoma From Primary Hypopharynx Source to Gastric Mucosa Presenting as Massive Gastrointestinal Bleeding
Monzer Abdallaa, Eltaib Saada, c, Mohammed S. Abdallaa, Mohammed Elamin Farisa, Ahmed A. Abdulrahmana, Khalid Mohameda, Ahmed M. Abdulrahmana, Abdurrahman Mustafaa, Dorota Fillipukb
aDepartment of Internal Medicine, Ascension Saint Francis Hospital, Evanston, IL, USA
bDepartment of Pathology, Ascension Saint Francis Hospital, Evanston, IL, USA
cCorresponding Author: Eltaib Saad, Department of Internal Medicine, Ascension Saint Francis Hospital, Evanston, IL, USA
Manuscript submitted February 14, 2023, accepted March 13, 2023, published online March 31, 2023
Short title: Metastatic SCC Presenting as GIB
doi: https://doi.org/10.14740/jmc4059
| Abstract | ▴Top |
Percutaneous endoscopic gastrostomy (PEG) is a relatively safe procedure that represents an important supportive adjunctive component for patients with primary head and neck squamous cell carcinoma (HNSCC). The HNSCC population is considered a high-risk group for developing critical nutritional deficiency due to a multitude of factors. Nevertheless, as the use of PEG in modern practice is gaining more popularity due to various indications, unusual complications have been increasingly reported. PEG site metastasis from primary HNSCC has emerged as a rare, yet serious oncological phenomenon that warrants careful consideration. The authors report an unusual case of squamous cell carcinoma (SCC) of the hypopharynx that metastasized to the gastric body mucosa through a PEG site. The metastatic SCC presented as massive gastrointestinal bleeding, and esophagogastroscopy revealed an ulcerated mass in the gastric body masquerading as a primary gastric adenocarcinoma. Histopathology and immunohistochemistry examination confirmed metastatic SCC which concurred with the patient’s primary hypopharyngeal SCC. The review of the updated literature revealed that a total of 121 cases of this rare oncological entity have been reported to date. Physicians need to be vigilant of the symptoms of PEG site metastasis to accurately diagnose and manage the care of this rare occurrence as it is associated with poor prognosis.
Keywords: Percutaneous endoscopic gastrostomy; PEG site metastasis; Primary head and neck squamous cell cancer; Upper gastrointestinal bleeding; Rare oncological phenomenon
| Introduction | ▴Top |
The technique of percutaneous endoscopic gastrostomy (PEG) was introduced by Gauderer and Ponsky in 1980 as an alternative way to provide long-term enteral access [1]. It has been widely used to provide nutrition and enteral access in patients with neurological and oropharyngeal disorders. Furthermore, patients with head and neck squamous cell carcinoma (HNSCC) represent a high-risk group requiring alternate means of enteral nutrition [1, 2]. PEG is considered a largely safe procedure with a 13% risk of occurrence of minor complications (such as superficial wound infections, stomal leak, and transient ileus), on other hand, the major complications (like major bleeding and visceral perforation) were reported in only 3% of the patients [3]. Nevertheless, as the use of PEGs in modern practice is gaining popularity due to various indications, more unusual complications have been increasingly reported [3]. PEG site metastasis of primary HNSCC has emerged as a rare, yet serious complication that deserves serious consideration, as the condition is usually associated with poor outcomes [3, 4].
Herein, the authors described an unusual case of metastatic squamous cell carcinoma (SCC) from a primary hypopharyngeal source to the gastric body mucosa, presumably from PEG site implantation, which presented as massive upper gastrointestinal bleeding. The patient was referred to oncology and was started on immunotherapy and palliative chemotherapy.
| Case Report | ▴Top |
Investigations
A 62-year-old male patient presented with a past medical history of stage IVA (T2N2M0) SCC of the hypopharynx (right pyriform sinus) that was initially diagnosed in August 2021 status post-primary radiotherapy (a total dose of 60 Gy) and chemotherapy (four cycles of carboplatin-based regimen) in October 2021 with interval downgrading of the hypopharyngeal tumor to stage II (T2N0M0). The treatment course was complicated by a cervicofacial actinomycosis infection that led to an acute hypercapnic respiratory failure from an acute upper airway obstruction that necessitated a tracheostomy placement and PEG placement (using Gauderer Ponsky technique) in March 2022. The patient has a history of a 50-pack-year smoking and alcohol use disorder. The patient presented to the emergency department in May 2022 with black-colored stools for 3 weeks. The patient denied nausea, vomiting, hematemesis, or abdominal pain and stated that he has been tolerating enteral feeding through the PEG without concerns.
An initial evaluation in the emergency department revealed a middle-aged male who was hemodynamically unstable with a blood pressure of 88/44 mm Hg and a pulse rate of 132 beats/min. The patient was pale but not jaundiced. The abdominal examination was remarkable for a dry and clean PEG site and moderate epigastric tenderness without guarding or rigidity. The digital rectal examination revealed a black tarry stool consistent with melena. The rest of the systemic examination was unremarkable.
Diagnosis
Initial laboratory results demonstrated an acute blood loss anemia with an extremely low hemoglobin of 3.3 g/dL (patient’s baseline 9.5 - 10.0 g/dL, reference range 13.0 - 17.0 g/dL), platelets of 576 × 103/mm3 (reference range 150 - 450 × 103/mm3), and an international normalized ratio (INR) of 1.0 (reference range 0.9 - 1.1). The comprehensive metabolic panel (CMP) was only remarkable for an elevated blood urea nitrogen (BUN) of 75 mg/dL (reference range 8.5 - 25 mg/dL).
Treatment
The patient received aggressive fluid resuscitation and intravenous pantoprazole therapy and he was transfused with four units of packed red blood cells. The patient was admitted to the intensive care unit (ICU) for close hemodynamic monitoring. An urgent esophagogastroduodenoscopy (EGD) revealed a large, ulcerated, non-circumferential mass in the greater curvature of the stomach with stigmata of recent bleeding, and multiple biopsies were obtained (Fig. 1a, b). Histopathology with immunohistochemistry confirmed a diagnosis of metastatic SCC that concurred with the patient’s primary hypopharyngeal SCC (Fig. 2a-c).
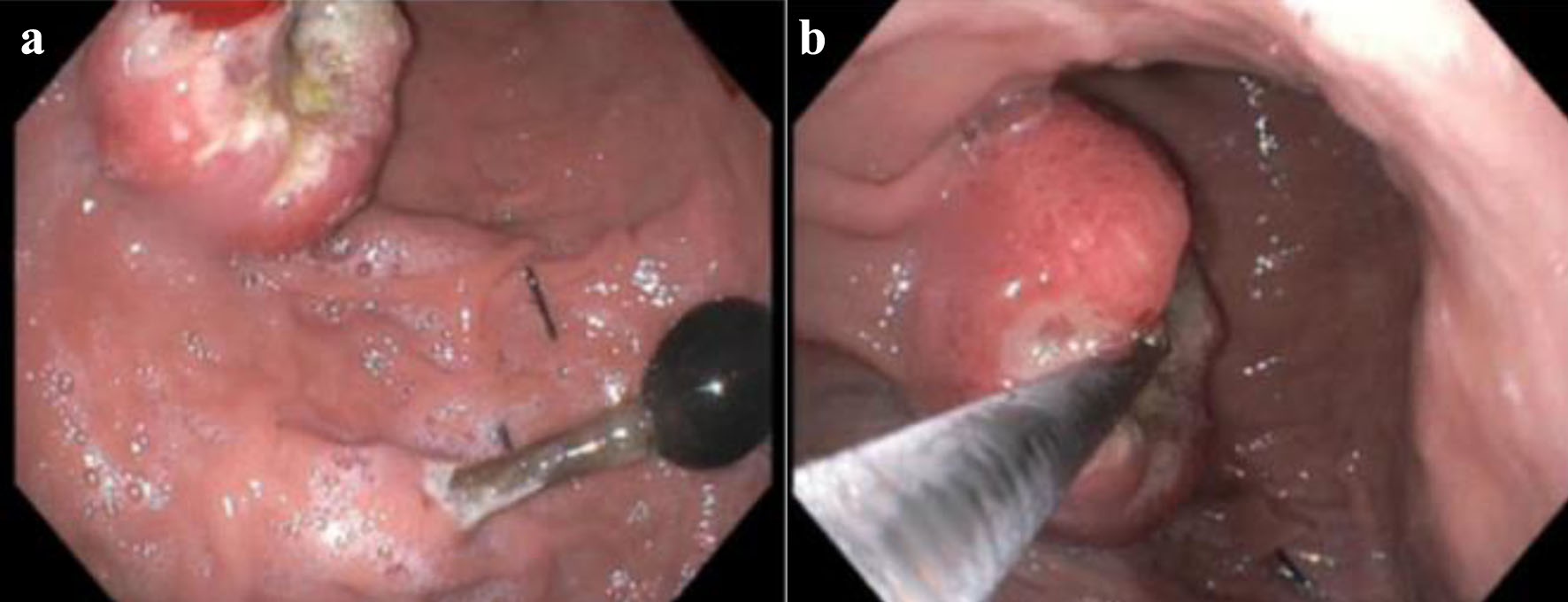 Click for large image | Figure 1. (a) The proximal end of PEG. (b) EGD showing an ulcerating circumferential gastric mass at the gastric body. PEG: percutaneous endoscopic gastrostomy; EGD: esophagogastroduodenoscopy. |
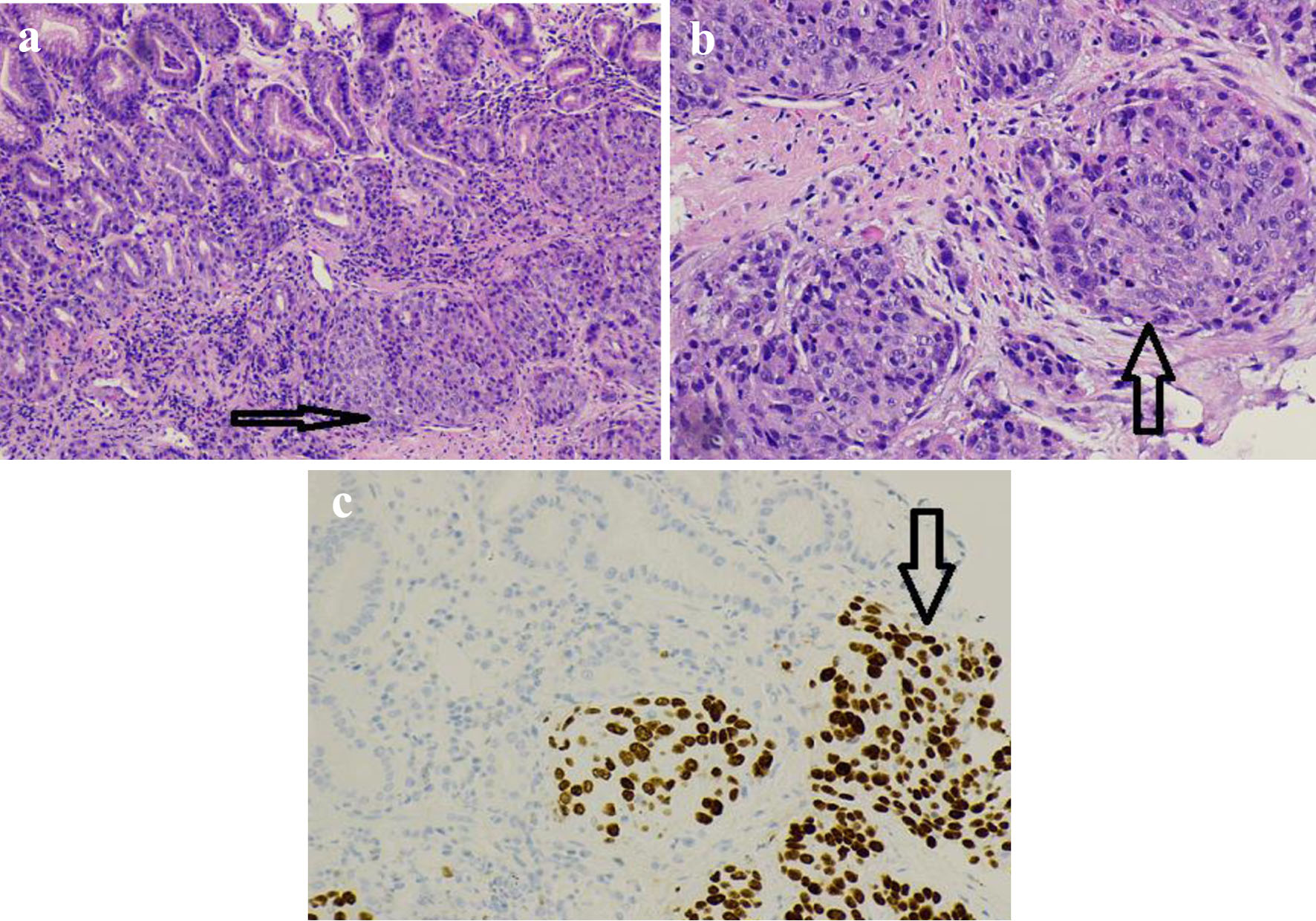 Click for large image | Figure 2. (a) H&E staining (× 100) of the biopsied gastric mass showing an invasive SCC (horizontal arrow) that concurred with the patient’s known hypopharyngeal SCC. (b) H&E (× 200) of the gastric biopsy with metastatic SCC (vertical arrow). (c) Immunohistochemistry staining (× 200) with strongly positive p63 uptake by the neoplastic cells (vertical arrow) confirming their SCC origin. H&E: hematoxylin and eosin; SCC: squamous cell carcinoma. |
Follow-up
A staging computed tomography (CT) scan of the abdomen and pelvis demonstrated a gastric mass in the greater curvature (Fig. 3) and multiple suspicious metastatic hepatic lesions, and CT of the neck soft tissue depicted markedly decreased size in the mass of the right piriform sinus compared to the previous imaging 10 months ago. The patient’s hemodynamic status stabilized, and hemoglobin remained stable without further episodes of gastrointestinal bleeding. He was safely discharged home with an oncology follow-up. The patient was commenced on immunotherapy (pembrolizumab), given the tumor’s strong positivity for programmed death-ligand-1 (PD-L1), and palliative chemotherapy with a carboplatin-based regimen.
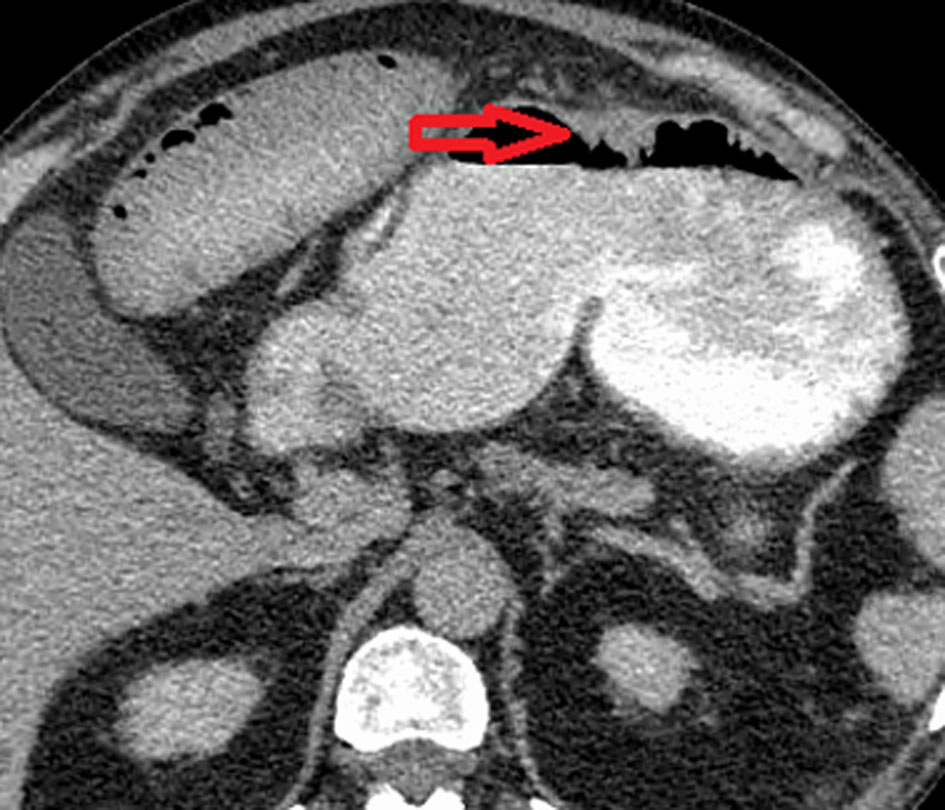 Click for large image | Figure 3. Contrast-based CT scan of the abdomen with a gastric mass in the greater curvature (horizontal arrow). CT: computed tomography. |
| Discussion | ▴Top |
Patients with HNSCCs are at increased risk of malnutrition up to 20-57%, because of a multitude of factors that encounter, for instance, increased catabolism, anorexia, dysphagia, odynophagia, and aspiration [3-7]. Poor nutrition has been linked with adverse outcomes in the HNSCC patients’ population, hence alternative nutritional support means have understandably been employed to improve life expectancy and overall outcome [3]. Moreover, the global benefits of enteral nutritional support have become well-established as an adjunctive component in the interdisciplinary management of primary HNSCC [8, 9].
Enteral feeding by open gastrostomy was first introduced in 1875, but this method has up to 50% risk of major complications associated with the procedure [3]. PEG tube feeding was introduced by Gauderer and Ponsky in 1980 [1] and has been a useful method of providing an alternative mean of adjunctive nutrition, especially for patients with primary HNSCC [3].
PEG site metastasis from primary HNSCCs is a rare but serious clinical entity [3, 8, 9]. According to a recent systematic review conducted by Siu et al in 2019 [8], a total of 121 cases of PEG site metastasis from various primary upper aerodigestive cancers were documented [8]. Most cases were of SCC pathology (95%). There were 86 cases available to be analyzed for clinical staging using the AJCC seventh edition [8]. Most cases had SCC as primary cancer (95%). More than two-thirds had stage IV (67.4%) with advanced nodal metastasis (N2/N3) (52%) at the time of PEG metastasis diagnosis [8], in keeping with our reported patient’s characteristics [8].
The average time from PEG placement to the diagnosis of metastasis was 7.78 ± 4.96 months, the average tumor size on detection was 4.65 (standard deviation (SD) 2.02) cm, and the average length of survival after detection was 7.26 (SD 6.23) months. About one-third of patients (33.1%) had evidence of other distant metastases at the time of PEG site metastatic diagnosis, in a similar pattern to this reported patient who was also found to have a metastatic liver disease identified at the time of PEG metastasis diagnosis [8].
The reviewed literature postulated several hypotheses for the metastasis at the PEG site [3, 8]. The direct seeding hypothesis postulates procedural inoculation of tumor cells, during the instrument passage through the primary aerodigestive neoplasm, that eventually implant at the PEG site [6, 8]. Nevertheless, cases of metastasis in patients in which a PEG was placed without instrument passage through the oral cavity or pharynx may favor alternate methods of tumor implantation [9]. Hematogenic or lymphatic dissemination to the PEG site, which may be more susceptible because of prior surgical trauma and local vascularization conditions, and lastly shedding of tumor cells into the digestive tube that selectively spread into the traumatized tissues of the PEG [6-8].
Interestingly, PEG site metastasis may take a relatively long time to develop (an average of 12 months) after the PEG placement; this observation may support the hematogenic dissemination theory, in contrast to the rapid development onset (around 7.9 months) that suggests the direct implantation model of PEG site metastasis [6].
They are diverse clinical presentations for PEG site metastasis from primary HNSCCs including unexplained abdominal pain, PEG site bleeding, ulceration around the PEG site, stomal drainage, and less commonly massive gastrointestinal bleeding as demonstrated in our case [3, 8]. Additionally, the condition may be asymptomatic and getting incidentally detected during the diagnostic workup for other complaints [3].
It is important to note that in several cases the diagnosis was delayed as the tumor was missed or underrecognized and treated as an infection or benign granulation tissue [8].
PEG site metastasis is generally associated with poor prognosis with a survival rate of 12.9% [3], although it may be better than other sites of distant metastatic disease in HNSCC in the term of prognosis (1-6.5%) [3, 7].
In contrast to the most commonly used “pull technique” of Gauderer and Ponsky, alternative techniques (push, direct, or radiologically inserted) were not shown to have a significantly reduced incidence of PEG site metastasis [8, 9]. The available literature revealed a lack of any statistical data to support a relationship between the “pull” method and PEG metastasis suggesting that this complication cannot be avoided simply by use of alternate PEG placement methods [9]. It was theorized that regardless of the method used, the surgical placement of PEG tubes creates an environment potentially favorable for tumor implantation as the tumor cells have an increased likelihood of implanting in the incision site due to increased circulation to the inflamed site [8]. Therefore, physicians need to be vigilant of the symptoms of PEG site metastasis to accurately diagnose and manage the care of this rare occurrence [9].
Conclusion
The authors described an unusual case of a primary hypopharyngeal SCC that metastasized to the gastric body mucosa through a PEG site implantation. The metastatic SCC presented as massive gastrointestinal bleeding with a large, ulcerated mass in the gastric body on the EGD masquerading as a primary gastric adenocarcinoma. Physicians need to be vigilant of the symptoms of PEG site metastasis to accurately diagnose and manage the care of this rare occurrence as it is associated with poor prognosis.
Learning points
PEG is a relatively safe procedure that represents an important supportive adjunctive component for patients with primary HNSCC.
PEG site metastasis from primary HNSCC has emerged as a rare, yet serious oncological phenomenon that warrants careful consideration.
Physicians need to be vigilant of the symptoms of PEG site metastasis to accurately diagnose and manage the care of this rare occurrence as it is associated with poor prognosis.
Further research is warranted to explore whether changes in the PEG placement techniques or in the timing of adjunctive therapies of HNSCC would minimize the incidence of this oncological phenomenon.
Acknowledgments
The authors would like to acknowledge the Department of Pathology at Saint Francis Presence Hospital for providing valuable input to this case presentation.
Financial Disclosure
The authors confirm that there is no funding to declare regarding the publication of this case report.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Informed Consent
Informed written consent was obtained from the patient to write and publish his case as a case report with all accompanying clinical and radiological images. No personal identifying information has been used in this article.
Author Contributions
MA, ES, and MSA contributed to conceptualizing and writing the first manuscript. MEF, AA, KM, and AM have contributed to the editing of the manuscript. DF provided and reviewed the histopathology and immunohistochemistry images. ES performed the critical review and editing of the final draft. All authors agreed to the final draft submission.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Gauderer MW, Ponsky JL, Izant RJ, Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
doi - Glicksman JT, Bottoni D, Shepherd J, Parry N, Franklin JH. Carcinoma of the larynx, metastatic to illeum, presents as ruptured appendicitis: case report and literature review. J Otolaryngol Head Neck Surg. 2014;43(1):18.
doi pubmed pmc - Huang AT, Georgolios A, Espino S, Kaplan B, Neifeld J, Reiter ER. Percutaneous endoscopic gastrostomy site metastasis from head and neck squamous cell carcinoma: case series and literature review. J Otolaryngol Head Neck Surg. 2013;42(1):20.
doi pubmed pmc - Schneider AM, Loggie BW. Metastatic head and neck cancer to the percutaneous endoscopic gastrostomy exit site: a case report and review of the literature. Am Surg. 1997;63(6):481-486
- Bekdache O, Al Nuaimi L, El Salhat H, Sharma V, Nowrasteh G, Al Rawi SJ. Uncommon metastasis of laryngeal cancer to small bowel causing intestinal obstruction treated by laparoscopic approach. Case Rep Surg. 2014;2014:260631.
doi pubmed pmc - Querichelli AFA, Faria FL, Martinez LF, Campos Junior E. Squamous cell carcinoma implantation in gastrostomy orifice. Case report. Einstein (Sao Paulo). 2020;18:eRC5409.
doi pubmed pmc - Vincenzi F, De Caro G, Gaiani F, Fornaroli F, Minelli R, Leandro G, Di Mario F, et al. Risk of tumor implantation in percutaneous endoscopic gastrostomy in the upper aerodigestive tumors. Acta Biomed. 2018;89(8-S):117-121.
doi pubmed pmc - Siu J, Fuller K, Nadler A, Pugash R, Cohen L, Deutsch K, Enepekides D, et al. Metastasis to gastrostomy sites from upper aerodigestive tract malignancies: a systematic review and meta-analysis. Gastrointest Endosc. 2020;91(5):1005-1014.e1017.
doi - Montes de Oca MK, Nye A, Porter C, Collins J, Satterfield C, Schammel CMG, Trocha SD. Head and neck cancer PEG site metastases: Association with PEG placement method. Head Neck. 2019;41(5):1508-1516.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


