| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 4, April 2023, pages 137-140
Rare Case of Tongue Ischemia Following Cardiopulmonary Bypass
Alexandrea L. Garretta, d, Lauren V. Weberb, Amar M. Bhatta, c
aDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
bCollege of Pharmacy, The Ohio State University, Columbus, OH, USA
cDepartment of Anesthesiology & Pain Medicine, Divisions of Critical Care and Cardiothoracic Anesthesiology, The Ohio State University College of Medicine, Columbus, OH, USA
dCorresponding Author: Alexandrea Garrett, Department of Anesthesiology & Pain Medicine, The Ohio State University, Columbus, OH 43210, USA
Manuscript submitted April 12, 2023, accepted April 20, 2023, published online April 30, 2023
Short title: Tongue Ischemia and Cardiopulmonary Bypass
doi: https://doi.org/10.14740/jmc4100
| Abstract | ▴Top |
Tongue ischemia is a devastatingly rare disease complication that is typically attributed to cranial arteritis, vasculitis, or prolonged oral intubation that manifests in a patient as a phenotypically black or discolored tongue. There have been less than 10 cases reported in the literature, however, documenting tongue ischemia secondary to shock states requiring high-dose vasopressor support. In these cases, the ischemia or necrosis has typically been limited to the tip of the tongue or has been associated with unilateral disease as bilateral tongue involvement is unlikely given the collateral blood supply of the tongue. To date, the use of imaging modalities to confirm lingual artery disease as the etiology for the presentation of tongue ischemia has been limited. We present a unique case of bilateral tongue ischemia following the use of cardiopulmonary bypass which was confirmed with radiographic evidence demonstrating bilateral lingual artery disease. The nature of case is presented, previous reports of similar cases are reviewed, and potential etiologies of this rare manifestation are discussed.
Keywords: Tongue ischemia; Cardiopulmonary bypass; Shock; Critical care
| Introduction | ▴Top |
Tongue ischemia is a devastatingly rare complication of cranial arteritis, vasculitis, or prolonged oral intubation that manifests as a phenotypically black or discolored tongue. In less than 10 cases reported in the literature, tongue ischemia has instead been attributed to atherosclerotic disease and shock states in cases requiring high-dose vasopressor support. In these cases, ischemia or necrosis has typically been limited to the tip of the tongue or one side of the tongue due to the bilateral and collateral blood supply of the tongue. Due to patient instability, utilization of imaging to confirm lingual artery disease as the etiology for the presentation in these cases has been limited. One reported case of septic shock failed to visualize the lingual arteries on bedside duplex [1], while another case of spontaneous tongue ischemia showed evidence of severe carotid disease without lingual artery involvement on a computed tomography (CT) [2]. Further studies have instead confirmed lingual artery disease with histological examination post-mortem [3, 4]. To the best of our knowledge, this is the first reported case of a bilateral presentation of tongue ischemia secondary to mixed cardiogenic and vasoplegic shock following cardiopulmonary bypass in which imaging modalities have confirmed bilateral lingual artery involvement as the etiology for the patient presentation.
| Case Report | ▴Top |
Investigations
The patient is a 77-year-old female with a past medical history notable for breast cancer status post chemotherapy and radiation to the chest, severe aortic stenosis, and concomitant coronary artery disease with 90% occlusion of the left anterior descending artery. Consent has been obtained from the patient to publish details regarding her treatment information, diagnosis, prognosis, hospital admission, and photographs related to her care. The patient underwent tissue aortic valve replacement and saphenous vein graft bypass to the left anterior descending artery via midline sternotomy. Induction of anesthesia and intubation were uncomplicated. Intraoperatively, the left internal mammary artery was dissected out but found to be atretic and unusable for bypass, necessitating the use of the greater saphenous vein which was also noted to be very small. Upon discontinuation of cardiopulmonary bypass, there was noted to be a decline in cerebral head saturations greater than 25% from baseline for 30 min suggesting underlying reduced mean arterial perfusion and subsequent reduced cerebral artery perfusion. This was corrected with the use of vasopressors, and the patient was taken to the intensive care unit for subsequent care where she was extubated 2 h postoperatively.
Diagnosis
The patient’s postoperative course was complicated by persistent lactic acidosis and high-dose vasopressor support in order to achieve a mean arterial perfusion pressure goal of > 65 mm Hg. Her shock was presumed to be mixed cardiogenic and vasoplegic shock following cardiopulmonary bypass. Approximately 15 h into her postoperative course, she became lethargic and exhibited a leftward gaze with right upper extremity weakness. These symptoms resolved over the course of 15 min. Interestingly, progressive bilateral tongue ecchymoses was also appreciated during her neurological exam (Fig. 1). At that time, she endorsed symptoms of tongue numbness and dysgeusia. A CT scan of her head was negative for acute hemorrhage, and a CT angiogram of her brain and neck showed no large vessel occlusion. Thus, her constellation of symptoms likely suggested an underlying transient ischemic attack. Upon further evaluation of the CT angiogram of her brain and neck, there was only mild calcification noted at the bifurcation of the right common carotid artery and only 50% focal stenosis of the distal left common carotid artery. However, the right lingual artery was found to be completely occluded with mild distal collateral flow while the left lingual artery was found to have multifocal irregularities (Fig. 2).
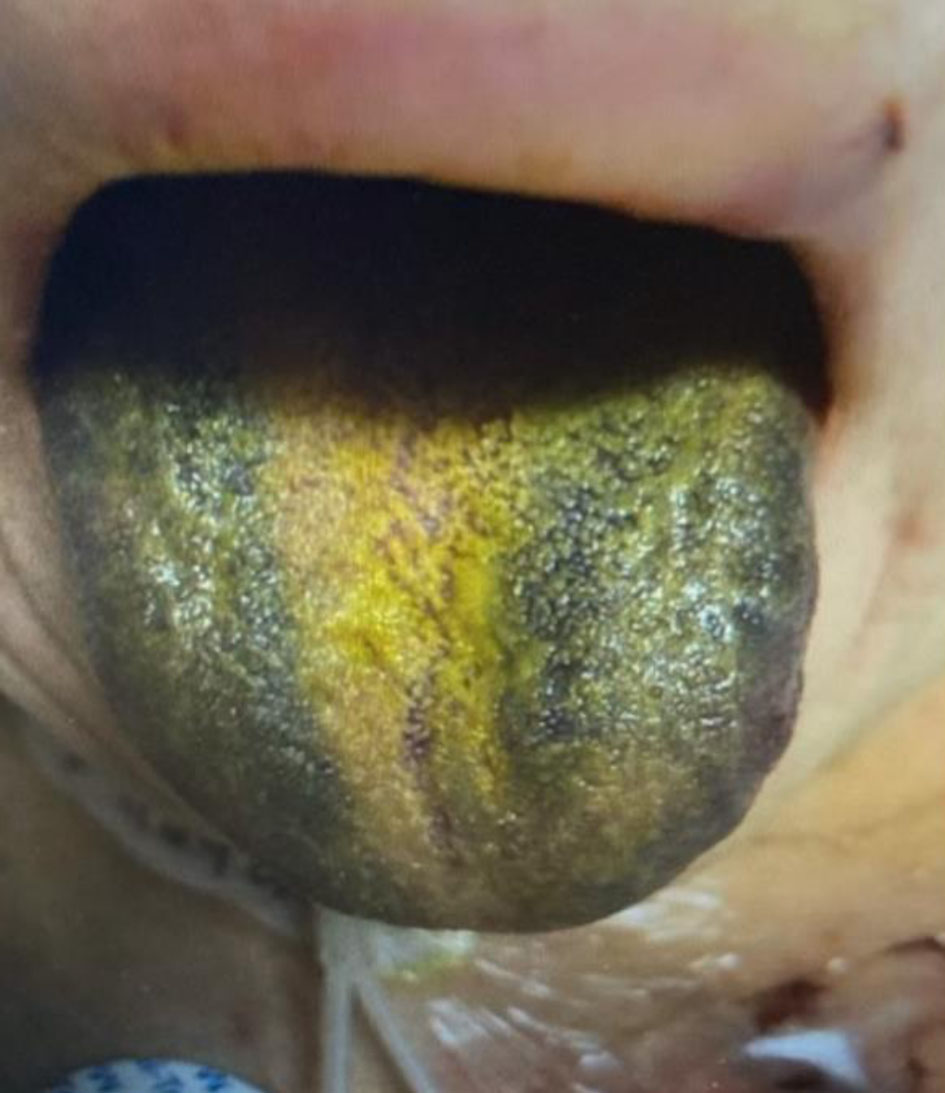 Click for large image | Figure 1. Bilateral ecchymosis of the patient’s tongue noted on exam. |
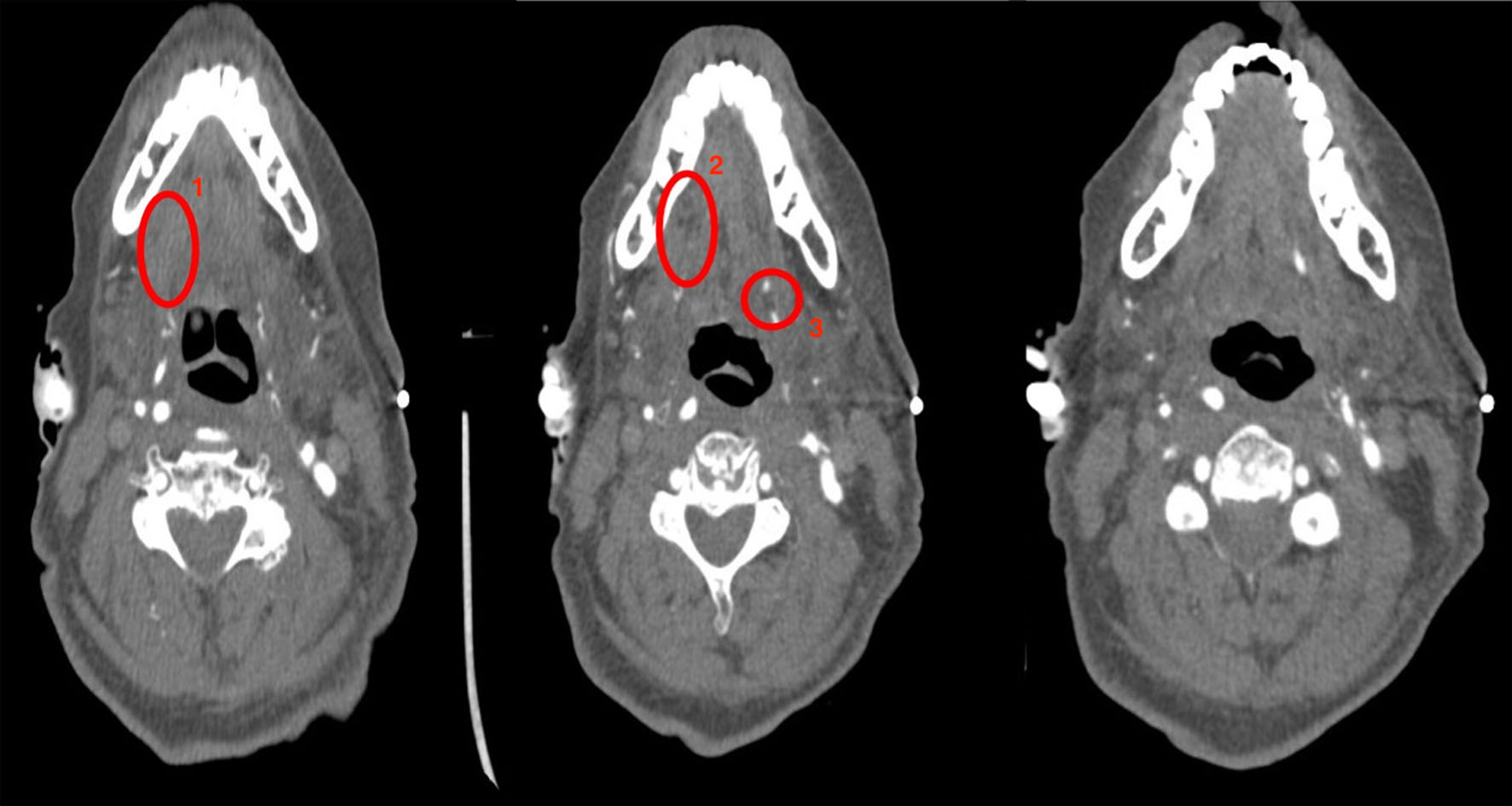 Click for large image | Figure 2. CT angiogram findings of a completely occluded right lingual artery with mild distal collateral flow (circles 1 and 2) and left lingual artery with multifocal irregularities (circle 3). CT: computed tomography. |
Treatment
Her postoperative platelet count, prothrombin time (PT), international normalized ratio (INR), and fibrinogen were in normal limits. She had no prior history of known vasculitic disease. An ADAMTS13 inhibitor screen returned normal to rule out acquired thrombotic thrombocytopenic purpura (TTP) as an etiology for possible lingual emboli given her imaging findings. With the nature of her shock state, the patient was treated with volume resuscitation with both crystalloid and colloid. She initially required low-dose epinephrine to support her cardiac function, but she had a persistent high-dose requirement of both norepinephrine and vasopressin to support her systemic vascular resistance in the setting of vasoplegic shock. Her systemic vascular resistance gradually improved with time over the course of 2 days. The otolaryngology service was consulted to perform serial examinations of the patient’s tongue. The patient underwent evaluation with multiple flexible bronchoscopes to monitor for progression of her disease.
Follow-up and outcomes
The patient experienced persistent tongue numbness and dysgeusia throughout her hospital stay, and supportive therapy was offered. Her examination and symptoms gradually improved with treatment of her underlying shock state without the need for surgical intervention. Approximately 2 months postoperatively, tongue sensation and taste had returned to baseline.
| Discussion | ▴Top |
Tongue ischemia and subsequent tongue necrosis are very rare manifestations of systemic disease, most commonly associated with giant cell arteritis [5]. Other cases of tongue ischemia have been reported due to Wegener’s granulomatosis [6], rheumatoid vasculitis [7], disseminated intravascular coagulation [3], prolonged oral intubation [8, 9], and end-organ emboli [2, 4, 10]. There have been three cases reported following treatment for septic shock [1, 11], and six cases reported following treatment for cardiogenic shock [1, 12]. Unfortunately, the patients in seven of these nine cases expired shortly after diagnosis due to multisystem organ failure. Due to patient instability, imaging studies were not performed in most of these cases. In one case of septic shock [1], a bedside duplex was performed which did not detect lesions of the external carotid arteries but was also unable to directly visualize the lingual arteries.
The blood supply is provided to the tongue via bilateral lingual arteries which are branches of the external carotid arteries. There may also be collateral blood supply from the facial artery and pharyngeal artery. The collateral blood supply to the tongue likely contributes to why unilateral disease presentation is more common, especially in vasculitis disease cases where treatment of the underlying disease may resolve the ischemia before it progresses to necrosis of the tongue. However, it does not help to explain why states of hypoperfusion may lead to tongue ischemia especially without signs or symptoms of hypoperfusion to other organs such as the gastrointestinal tract. Roman et al hypothesized that blood flow is preferentially diverted to the internal carotid system, rather than the external carotid system, during shock states to perfuse the brain at the expense of other muscular organs, including the tongue [5]. The researchers also hypothesized that treatment with an intra-aortic balloon pump (IABP) in cases of cardiogenic shock may not be protective against tongue ischemia as shown in three of their five reported cases [5]. This is likely because an IABP does not augment carotid flow as it operates distal to the carotid artery take-off points.
Of the cases related to states of shock expressed in the current literature, including the case [11] involving the prolonged use of terlipressin (an anti-diuretic hormone analogue), there has not been definitive evidence to suggest a specific dose of vasopressor that may be more probable to contribute to tongue ischemia. Given that the patient in our case as well as a patient in a previously reported case of circulatory shock [5] did not show signs of hypoperfusion to other organs such as the gastrointestinal tract, there must be a multitude of contributing factors to lingual artery disease process. Thus, tongue ischemia may be caused by any severity of shock at any time during the disease process and may indicate a poor prognosis for the patient given the high mortality rate in the available published cases [1, 5, 11, 12].
In our case, the patient was known to have very atretic vessels systemically as evidenced by the intraoperative findings of her small internal mammary arteries and saphenous veins. This suggests that her lingual arteries were also likely to be relatively small. More so, given she was undergoing coronary artery bypass grafting, she has known coronary artery disease with likely peripheral vascular disease. Intraoperatively, she was known to have reduced cerebral perfusion, as evidenced by her reduction in cerebral head saturations, as well as reduced systemic mean arterial pressures as evidenced by her persistent postoperative vasopressor requirement. Despite minimal evidence of carotid artery disease noted on the CT angiogram of her brain and neck, this patient still experienced significant lingual artery disease manifestation as noted on the same scan. Given her concomitant history of a transient ischemic attack postoperatively, this may suggest atherosclerotic emboli as the cause for her disease state although it would be unusual to be bilateral. It is also possible that she had shower emboli during aortic cross cramp intraoperatively, but her tongue had not been examined until her neurologic exam during her transient ischemic attack. It is unlikely that prolonged oral intubation may have contributed to her symptomology given her short duration of endotracheal intubation compared to the cases in which this was a hypothesized etiology [8, 9]. Nevertheless, these factors suggest that her disease manifestation may very well have been multifactorial as no single etiology could be identified.
This case highlights a rare potential sequalae of cardiopulmonary bypass that may present in critically ill patients. This case also highlights that imaging modalities may be of utility in diagnosis for an unusual clinical finding of a discolored tongue. It is clear that many complex factors may contribute to the clinical picture, and clinicians should be aware of these risk factors to aid in prompt diagnosis. In our case, the end result was ideal as the patient’s symptoms improved without surgical management. However, given the high rate of mortality associated with tongue ischemia and necrosis as documented in the literature, consideration for surgery in more severe cases may be a viable option to debride necrotic tissue in order to reduce mortality. In conservative management approaches, the tissue may become necrotic, self-amputate, or even self-resolve. However, patients may go on to develop deformities of the tongue and/or develop speech, language, and swallowing difficulties in these cases as well [8, 9]. Thus, it is crucial that awareness of this complication is known in order to promote prompt diagnosis and management strategies.
Learning points
Tongue ischemia is an extremely rare disease manifestation that is typically a complication of cranial arteritis, vasculitis, or prolonged oral intubation. There have been less than 10 cases reported in the literature of tongue ischemia secondary to atherosclerotic disease or shock states. The disease typically presents as a unilateral black-appearing tongue or discoloration limited to the tip of the tongue. This is an important disease to recognize as tongue ischemia can progress to tongue necrosis which has an extremely high mortality rate. In cases in which patients survive, they may develop tongue deformities, speech and language alterations, or even swallowing difficulties. Our clinical experience suggests that imaging modalities can be of utility in identifying the etiology of the disease, and our case gives evidence to suggest that bilateral lingual artery disease is entirely possible despite the abundant collateral blood supply of the tongue. Prompt recognition, diagnosis, and treatment as in our case can lead to resolution of the ischemia to prevent disease progression and reduced mortality.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors deny any conflict of interest.
Informed Consent
Informed consent was obtained directly from the patient for anesthetic care and the use of patient data for publication purposes. The patient information was de-identified for publication.
Author Contributions
AG provided clinical care for the patient, performed the initial manuscript preparation, literature review, and editing of all revisions. LW participated in manuscript preparation, aided in the literature review, and assisted with editing of revisions. AB provided clinical care for the patient and participated in manuscript preparation (initial draft, revisions, and final version).
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Cho J, Sung K, Lee D. Ischemic necrosis of the tongue in surgical patients with septic shock: a case report. BMC Surg. 2016;16(1):48.
doi pubmed pmc - Bjordahl PM, Ammar AD. Tongue necrosis as an unusual presentation of carotid artery stenosis. J Vasc Surg. 2011;54(3):837-839.
doi pubmed - Kamatani T, Yamashita K, Okabayashi T, Maeda H, Toi M, Yamamoto T. Bilateral ischemic necrosis of the tongue due to disseminated intravascular coagulation. Int J Oral Maxillofac Surg. 2008;37(8):777-779.
doi pubmed - Kitamura N, Sasabe E, Kitaoka H, Yamamoto T. Unilateral necrosis of the tongue caused by embolisation of cholesterol crystals. Br J Oral Maxillofac Surg. 2018;56(4):340-342.
doi pubmed - Roman BR, Immerman SB, Morris LG. Ischemic necrosis of the tongue in patients with cardiogenic shock. Laryngoscope. 2010;120(7):1345-1349.
doi pubmed pmc - Carter LM, Brizman E. Lingual infarction in Wegener's Granulomatosis: a case report and review of the literature. Head Face Med. 2008;4:19.
doi pubmed pmc - Piechnik B, Swietlicki M, Klatka J. Tungue necrosis as a result of the overlap syndrome - case report. Polish Otorhinolaryngology Review. 2015;4(1):36-39.
- Adegbite NA, Avery C, Rajaram K, Mohamed Ahmed M. Tongue necrosis: a rare complication of prolonged oral intubation. J Surg Case Rep. 2019;2019(11):rjz284.
doi pubmed pmc - Haider S. A rare case of lingual necrosis secondary to prolonged endotracheal intubation. J Med Cases. 2016;7(10):429-431.
- McGoldrick DM, Khan I, Cotter CJ. Ischaemic necrosis of the tongue. BMJ Case Rep. 2015;2015:bcr2014208330.
doi pubmed pmc - Megarbane H, Barete S, Khosrotehrani K, Izzedine H, Moguelet P, Chosidow O, Frances C, et al. Two observations raising questions about risk factors of cutaneous necrosis induced by terlipressin (Glypressin). Dermatology. 2009;218(4):334-337.
doi pubmed - Hulstaert E, Roggeman E, Beeckman AS, Moerman M, Vanderstraeten E, Rasquin K, Monsaert E, et al. Ischaemic necrosis of the tongue as a rare complication of cardiogenic shock. Acta Clin Belg. 2015;70(6):436-439.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


