| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 8, August 2023, pages 277-281
Primary Mediastinal B-Cell Lymphoma Presenting as Cardiac Tamponade
Alexander T. Phana, Johnny S. Randhawaa, Brandon Johnstona, Chayanne Khosravib, Aldin Malkocc, Sarkis Arabiana, b
aDepartment of Internal Medicine, Arrowhead Regional Medical Center, Colton, CA 92324, USA
bDepartment of Critical Care Medicine, Arrowhead Regional Medical Center, Colton, CA 92324, USA
cDepartment of General Surgery, Arrowhead Regional Medical Center, Colton, CA 92324, USA
dCorresponding Author: Alexander Phan, Department of Internal Medicine, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted May 24, 2023, accepted July 8, 2023, published online August 28, 2023
Short title: Tamponade Associated With B-Cell Lymphoma
doi: https://doi.org/10.14740/jmc4106
| Abstract | ▴Top |
Primary mediastinal B-cell lymphoma (PMBCL) is a rare subtype of non-Hodgkin lymphoma. Typical symptoms include cough, chest pain, and dyspnea; however, cardiac tamponade as the primary manifestation is exceedingly rare. We hereby present a case of a 34-year-old male with a past medical history of obesity, who presented to our emergency department with a chronic dry cough for 4 months. On admission, computed tomography demonstrated a large 11.1-cm diameter anterior mediastinal mass, and echocardiography demonstrated cardiac tamponade physiology. The patient underwent further workup including pericardiocentesis, subsequent pericardial window, and mediastinal biopsy, which demonstrated histopathology consistent with PMBCL. Our case highlights the importance of a complete and thorough workup for patients with chronic untraditional symptoms. This case is unique in that PMBCL is rarely associated with cardiac tamponade as the primary clinical presentation. Additionally, we recommend an extensive cardiac workup for patients presenting with a large mediastinal mass, as failure to do so may result in patient morbidity and mortality.
Keywords: B-cell lymphoma; Mediastinal mass; Cardiac tamponade; Oncology; Internal medicine
| Introduction | ▴Top |
Primary mediastinal B-cell lymphoma (PMBCL) is a rare subtype of non-Hodgkin lymphoma, only occurring in about 2-3% of patients diagnosed with non-Hodgkin lymphoma [1, 2]. The tumor arises from a dysregulation in the Janus kinase signal transducer and activator of transcription (JAK-STAT), dysregulation of nuclear factor-κB (NF-κB) pathways, and amplification of 9p24.1 region of chromosome 9 [3]. Though some patients may be asymptomatic, others present with rapidly progressing symptoms such as a cough, hoarseness, dyspnea, dysphagia, airway damage, vascular damage, or B symptoms (i.e., fever, night sweats, weight loss). Symptoms are typically due to the rapidly enlarging mass in the mediastinum, causing a mass effect on adjacent structures in the mediastinum including, but not limited to, the lungs and superior vena cava. The symptoms can also be due to pleural or pericardial effusions, which are rare complications of this malignancy [2]. Most cases occur in the anterior superior mediastinum in the regions of the thymus and are typically seen in females at approximately a median age of 35 years [2, 3]. As such, a diagnosis of PMBCL in males is uncommon. Here we report the case of a 34-year-old male patient with a history of obesity, who presented with a chronic dry cough and was found to have cardiac tamponade as the primary manifestation of PMBCL.
| Case Report | ▴Top |
Investigations
A 34-year-old male with a history of obesity and gastric bypass surgery presented to the emergency department with chief complaints of dyspnea, dry cough, and dysphagia over a 4-month period. At the onset of his symptoms, he described a sore throat, accompanied by a dry cough, and dyspnea in the supine position. These symptoms progressed towards early satiety and postprandial hidrosis. The patient denied fever, night sweats, vision change, chest pain, or unintentional weight loss. Family history was notable for thyroid and lung cancer on the paternal side of his family. Social history was significant for cigarette smoking and occasional alcohol consumption. The patient’s initial vital signs included a blood pressure 124/85 mm Hg, pulse rate 94, temperature 36.4 °C, respiratory rate 18, and oxygen saturation of 96% on ambient air. Physical exam revealed an obese male, audible S1 and S2 heart sounds, diminished breath sounds at the right lung base, and normal mentation. The physical exam did not demonstrate distended neck veins or pericardial friction rub.
Diagnosis
Laboratory evaluation was significant for mild normocytic anemia and an elevated D-dimer (Table 1). A basic metabolic panel and serum troponin-I were within normal limits. Chest X-ray showed a density bordering the aortic arch, descending thoracic aorta, and upper portion of the left heart (Fig. 1). Subsequent computed tomography (CT) scan of the chest with intravenous (IV) contrast revealed a large anterior mediastinal mass with mass effect on adjacent structures, bilateral pleural effusions, pericardial effusion, and enlarged retroperitoneal lymph nodes (Fig. 2a, b). A transthoracic echocardiogram (TTE) was performed, revealing a large circumferential pericardial effusion with evidence of echocardiographic tamponade physiology, evidenced by less than 50% collapse of inferior vena cava and significant respiratory variation in the mitral and tricuspid inflow. An electrocardiogram demonstrated sinus tachycardia (heart rate of 104) without evidence of electrical alternans or ischemia.
 Click to view | Table 1. Initial Laboratory Findings, Demonstrating Normocytic Anemia and Elevated D-Dimer |
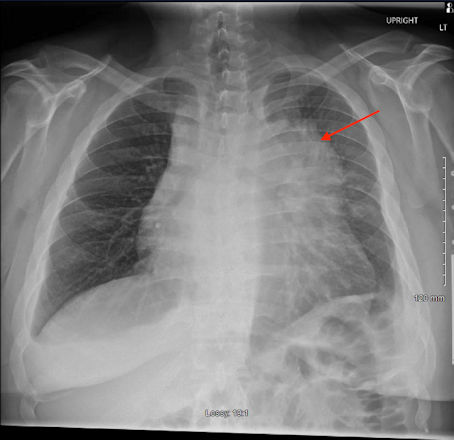 Click for large image | Figure 1. Posterior-anterior chest radiograph demonstrating a density bordering the aortic arch, descending thoracic aorta, and upper portion of the left heart (red arrow). |
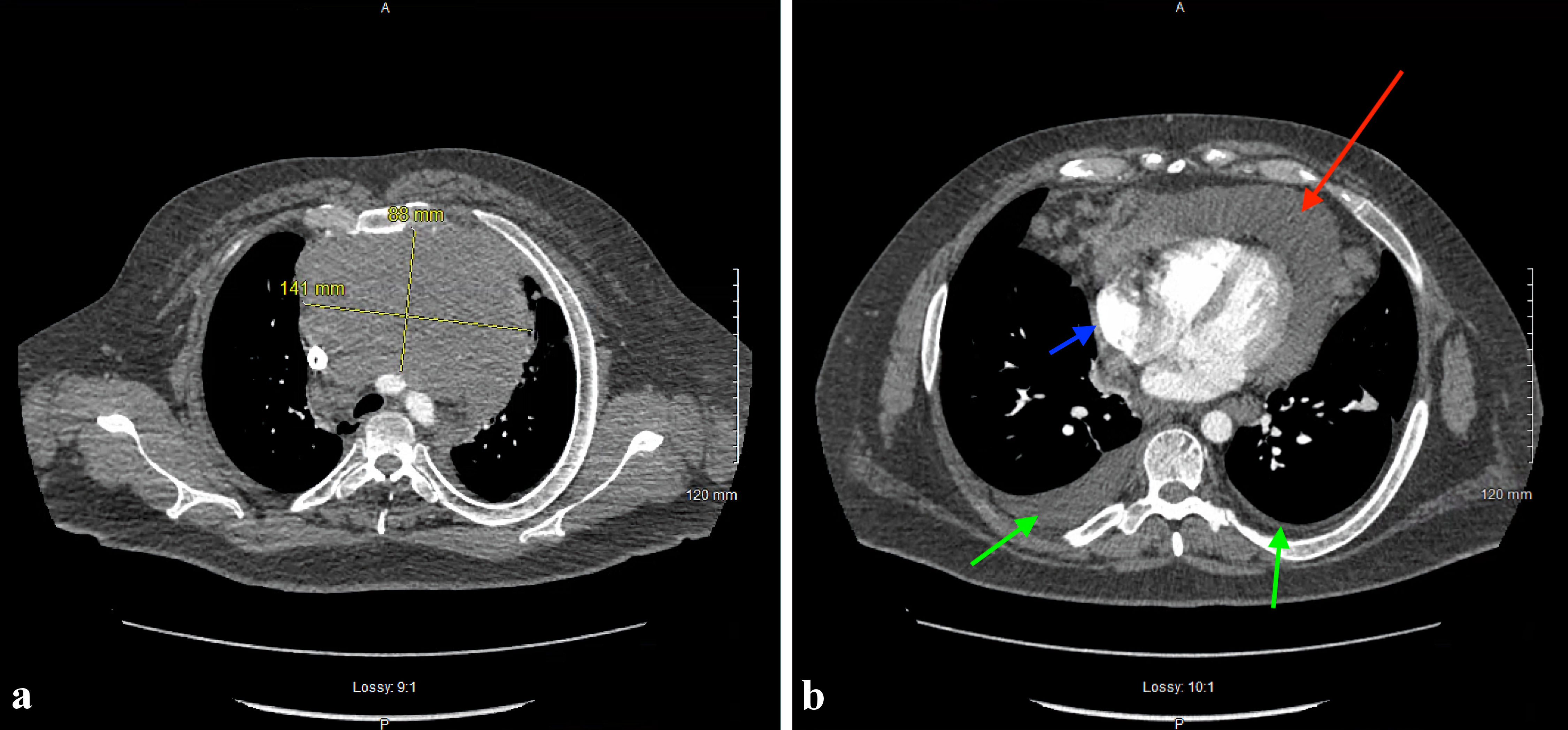 Click for large image | Figure 2. (a) Axial section of a computed tomography (CT) angiogram of the chest showing anterior mediastinal mass measuring 14.1 × 8.8 cm. (b) Axial section of a CT angiogram of the chest demonstrating an anterior mediastinal mass (red arrow) compressing cardiac structures, small pericardial effusion (blue arrow), and bilateral pleural effusions (green arrows). |
A pericardiocentesis was performed by interventional cardiology, yielding 350 mL of sanguineous fluid, and a pericardial drain was left in place. The next day, an additional 260 mL of serosanguinous fluid was removed. Cytology and flow cytometry studies of the pericardial fluid were negative for malignancy. Due to a suspicion for malignancy, our medical oncologist was consulted, who recommended a biopsy of the mediastinal mass and bone marrow biopsy. A needle biopsy of the mediastinal mass was thus obtained by our interventional radiology specialist, and the sample was sent for review by our pathologist. Over the next 7 days, the patient continued to drain over 100 mL of fluid into the pericardial drain, so a repeat echocardiogram was obtained, showing re-accumulation of moderate amounts of pericardial fluid with continued signs of hemodynamic compromise. Consequently, the cardiothoracic surgeon was consulted and performed a successful pericardial window. Five days after the pericardial window, another echocardiogram was obtained, demonstrating resolution of cardiac tamponade.
At this point in time, the mediastinal mass biopsy results returned, demonstrating primary mediastinal large B-cell lymphoma, as the tissue was positive for CD20, CD79a, B-cell lymphoma (Bcl)6, Bcl2, multiple myeloma 1 (MUM1), cellulary myc (c-myc), programmed cell death ligand 1 (PD-L1), CD30, and nuclear protein Ki-67 (Ki-67). The bone marrow biopsy results also demonstrated rare isolated atypical lymphoid cells. Additional laboratory studies were obtained, showing a lactate dehydrogenase level of 2,158 U/L (normal range: 120 - 230), normal serum alpha fetoprotein level, and normal serum human chorionic gonadotropin level.
Treatment
Based on results of the diagnostic workup, our oncologist suggested starting R-EPOCH therapy (rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin). The patient was also started on allopurinol 300 mg oral daily and monitored for signs of tumor lysis syndrome, which he never developed. The day before hospital discharge, 20 days into admission, the pericardial drains were removed. The patient was also given filgrastim for a 7-day period with close follow-up in the outpatient oncology, cardiology, and primary care clinics.
Follow-up and outcomes
To date, he is alive and well, and completing the remainder of his chemotherapy regimen. He has not had recurrence of cardiac tamponade and is tolerating chemotherapy well. He is also being followed closely in the medical oncology clinic.
| Discussion | ▴Top |
PMBCL derives from medullary thymic B cells and typically affects females in the third and fourth decades of life [4]. Previously, it was thought to be a subset of diffuse large B-cell lymphoma; however, it is now recognized as its own entity based on molecular features and represents approximately 2-4% of all non-Hodgkin lymphomas [5]. Symptoms at the time of diagnosis are attributed to the location of the mass in the anterior mediastinum, including cough, chest pain, and dyspnea [4, 6, 7]. Although PMBCL typically is confined to the mediastinum, it may also involve surrounding structures [4]. Involvement of structures, such as the heart, bronchial tree, and superior vena cava may pose life-threatening risks to patients, representing an oncologic emergency [4]. PMBCL may present with pleural and pericardial effusions in up to approximately 50% of cases; however, cardiac tamponade as the primary manifestation of PMBCL is exceedingly rare. Only several case reports have noted cardiac tamponade as the primary diagnosis at the time of hospital admission [8-12].
The standard diagnostic workup for PMBCL includes complete hematologic examination, total body CT, mediastinal mass biopsy, and bone marrow aspirate and biopsy [7]. Consistent with the current literature, our patient’s mediastinal mass biopsy results demonstrated positivity for CD20, CD79a, Bcl6, Bcl2, MUM1, c-myc, PD-L1, CD30, and Ki-67 [8-12]. Additionally, PMBCL classically does not involve the bone marrow, as is the case for our patient. Clinically, the patient did not present with hypotension or electrical alternans; however, echocardiography demonstrated significant respirophasic changes of the inferior vena cava and disruption of mitral and tricuspid inflow, representing clinical cardiac tamponade. The patient underwent pericardiocentesis, but due to large pericardial output, he ultimately underwent a pericardial window for definitive pericardial drainage. Repeat echocardiography demonstrated resolution of tamponade and the patient was initiated on chemotherapy with rituximab, etoposide, vincristine, and doxorubicin (R-EPOCH). R-EPOCH therapy has become more popular since 2013 and has been shown to have high rates of complete response (84%) as opposed to an alternative regimen of rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone (R-CHOP), which showed 70% complete response. Additionally, R-EPOCH patients had less exposure to radiation when compared to patients undergoing R-CHOP [13]. As such, our oncologist decided to utilize R-EPOCH. He was safely discharged home with close outpatient primary care and oncology follow-up appointments, and he has not had any further re-admissions for cardiac tamponade.
This case is unique for several reasons. First, PMBCL is more common in females, and this patient is of male sex. Second, cardiac tamponade as the primary manifestation is rare, as previously mentioned. Third, the patient’s clinical exam did not demonstrate typical signs of cardiac tamponade, as in distended neck veins, pericardial friction rub, and hypotension; further, his electrocardiogram did not show evidence of electrical alternans. The diagnosis of cardiac tamponade was made through a transthoracic echocardiogram, which was obtained due to CT imaging demonstrating compression of the heart. Careful clinical consideration was made in the evaluation of this patient, and we believe that this is one of the major strengths of our case study. Another strength is that he underwent prompt therapeutic interventions and has had excellent outpatient follow-up with a primary care physician, cardiologist, and oncologist. The major limitation to our case report lies in the fact that there is a dearth of information in the current literature citing cardiac tamponade as a manifestation of PMBCL; despite this limitation, we believe that our case contributes well as an addition to the limited body of literature.
Conclusions
PMBCL is a rare subtype of non-Hodgkin lymphoma, and is currently defined as its own entity, separate from diffuse large B-cell lymphoma. This case highlights the rare instance in which PMBCL manifests primarily as cardiac tamponade. Additionally, PMBCL is uncommon in males, and we would like to contribute to the body of evidence citing a male patient afflicted by PMBCL. When presented with a patient that has a mediastinal mass, clinicians should remain vigilant for any signs or symptoms of cardiac tamponade, as this condition may progress towards a medical emergency if left untreated. Further investigation will need to be pursued into elucidating risk factors predisposing patients with PMBCL to cardiac tamponade and if there are any specific chemotherapeutic agents best suited for patients with tamponade.
Learning points
Our case report aims to contribute to the limited current body of literature citing cardiac tamponade as the primary manifestation of PMBCL. Clinicians should maintain a high degree of suspicion for PMBCL when a patient presents with cardiac tamponade and a large anterior mediastinal mass. Moving forward, future studies should collect larger patient sample sizes of PMBCL to identify risk factors associated with cardiac tamponade and if there are any specific chemotherapeutic agents best suited for patients who present with cardiac tamponade.
Acknowledgments
The authors would like to thank and express their gratitude to Arrowhead Regional Medical Center’s exceptional nursing staff and unit managers for their expert clinical support.
Financial Disclosure
The authors have no financial or funding disclosures.
Conflict of Interest
The authors declare there is no conflict of interest.
Informed Consent
Informed consent was obtained from the family of the patient. The patient was also appropriately de-identified for this manuscript.
Author Contributions
ATP, JSR, BJ, CK and AM contributed to the initial manuscript write-up, literature review, and editing of the manuscript. SA attended on the case and contributed to decision-making, management of the patient, literature review, and editing of the manuscript.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
PMBCL: primary mediastinal B-cell lymphoma; JAK-STAT: Janus kinase signal transducer and activator of transcription; NF-κB: nuclear factor-κB; TTE: transthoracic echocardiogram; CT: computed tomography; IV: intravenous; Bcl: B-cell lymphoma; MUM1: multiple myeloma 1; c-myc: cellulary myc; Ki-67: nuclear protein Ki-67; PD-L1: programmed cell death ligand 1; R-EPOCH: rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin
| References | ▴Top |
- Khalid S, Khalid A, Daw H, Maroo P. Management of primary mediastinal B-cell lymphoma in pregnancy. Cureus. 2018;10(2):e2215.
doi pubmed pmc - Yu Y, Dong X, Tu M, Wang H. Primary mediastinal large B cell lymphoma. Thorac Cancer. 2021;12(21):2831-2837.
doi pubmed pmc - Ahmed Z, Afridi SS, Shahid Z, Zamani Z, Rehman S, Aiman W, Khan M, et al. Primary mediastinal B-cell lymphoma: a 2021 update on genetics, diagnosis, and novel therapeutics. Clin Lymphoma Myeloma Leuk. 2021;21(11):e865-e875.
doi pubmed - Dunleavy K, Wilson WH. Primary mediastinal B-cell lymphoma and mediastinal gray zone lymphoma: do they require a unique therapeutic approach? Blood. 2015;125(1):33-39.
doi pubmed pmc - Steidl C, Gascoyne RD. The molecular pathogenesis of primary mediastinal large B-cell lymphoma. Blood. 2011;118(10):2659-2669.
doi pubmed - Lees C, Keane C, Gandhi MK, Gunawardana J. Biology and therapy of primary mediastinal B-cell lymphoma: current status and future directions. Br J Haematol. 2019;185(1):25-41.
doi pubmed pmc - Martelli M, Ferreri A, Di Rocco A, Ansuinelli M, Johnson PWM. Primary mediastinal large B-cell lymphoma. Crit Rev Oncol Hematol. 2017;113:318-327.
doi pubmed - Yendamuri R, Gonzalez D, Barve N, Bashir HI. A case of diffuse B cell lymphoma inducing cardiac tamponade in a young female. Am J Respir Crit Care Med. 2022;205:A2838.
doi - Castro E. Primary mediastinal B cell non-Hodgkin lymphoma presenting as superior vena cava syndrome and pericardial effusion in tamponade in a 28-year-old female: a case report. CHEST Journal. 2020;158(4S):1448A.
doi - Eldib OS, Shakwer E, Habeeb K. Cardiac tamponade; a rare presentation of mediastinal lymphoma. Journal of Case Reports in Practice. 2014;2(4):113-115.
- Percuku L, Berisha G, Haliti E, Bajraktari G. Mediastinal Lymphoma Presenting With Cardiac Tamponade. JACC. 2017;119(suppl 8):e69-e70.
doi - Kumagai T, Abe K, Enomoto K, Maebou A, Hara H, Yoshimoto T, Hirao F. [A case of mediastinal malignant lymphoma with cardiac tamponade treated effectively with chemotherapy]. Nihon Kyobu Shikkan Gakkai Zasshi. 1992;30(7):1308-1314.
pubmed - Shah NN, Szabo A, Huntington SF, Epperla N, Reddy N, Ganguly S, Vose J, et al. R-CHOP versus dose-adjusted R-EPOCH in frontline management of primary mediastinal B-cell lymphoma: a multi-centre analysis. Br J Haematol. 2018;180(4):534-544.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


