| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 8, August 2024, pages 180-185
Primary Hyperparathyroidism and Pulmonary Embolism in Patients With a Fractured Neck of Femur
Yashar Mashayekhia, Sara Baba-Aissaa, Amina Al-Qaysib, Mohammed Eishc, Abdulmalik Timamyc, Maria Panourgiad, e, Mohamed H. Ahmedd, e, f, g
aFaculty of Medicine and Health Sciences, The University of Buckingham, Buckingham, UK
bDepartment of Diabetes and Endocrinology, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
cDepartment of Orthopaedic and Trauma, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
dDepartment of Geriatric Medicine, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
eHonorary Senior Lecturer of the Faculty of Medicine and Health Sciences, University of Buckingham, Buckingham, UK
fDepartment of Medicine and HIV Metabolic Clinic, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
gCorresponding Authors: Mohamed H. Ahmed, Department of Medicine and HIV Metabolic Clinic, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes, Buckinghamshire, UK
Manuscript submitted April 27, 2024, accepted July 1, 2024, published online July 18, 2024
Short title: Primary Hyperparathyroidism and PE in Patients With NOF
doi: https://doi.org/10.14740/jmc4235
| Abstract | ▴Top |
Two patients aged 82 and 77, with a fractured neck of the femur, were found to have primary hyperparathyroidism, characterized by hypercalcemia and hypercalciuria. Post-surgery, both developed pulmonary embolism (PE), highlighting a possible link between hypercalcemia and increased hypercoagulation risk. There have been few case reports suggesting the association between hypercalcemia due to hyperparathyroidism and the increase in tendency of hypercoagulation and subsequent risk of venous thromboembolism (VTE). This case series offers insights into how ionized calcium influences thrombin formation, platelet activation and aggregation, and activation of clotting factors such as factor VII and factor X, raising questions about the role of chronic hypercalcemia in VTE. Further research is needed to 1) establish whether chronic hypercalcemia in the absence of fracture can modulate the risk of hypercoagulation; 2) determine whether chronic hypercalcemia in individuals with bone fracture may represent a significantly higher hypercoagulability risk during the postoperative periods.
Keywords: Primary hyperparathyroidism; Pulmonary embolism; Hypercalcemia; Fracture neck of the femur
| Introduction | ▴Top |
Primary hyperparathyroidism (PHPT) is a common endocrine disorder whereby the parathyroid gland secretes excessive parathyroid hormone (PTH). It affects approximately four in 1,000 individuals in the UK [1] and is twice as common in women than in men.
The condition arises from various etiologies, including solitary adenomas (85% of cases), multiglandular disease (10-15%), and parathyroid carcinoma (< 1%) [2]. PTH acts on the bones, kidneys, and intestines to increase serum calcium levels. In bones, PTH stimulates osteoclast activity, causing bone resorption and releasing calcium into the bloodstream, which further enhances intestinal calcium absorption [3]. Thus, patients with PHPT suffer from chronic hypercalcemia. Ionized calcium, as the coagulation factor IV, participates in the coagulation process and is necessary for thrombin formation. Calcium is also crucial for the activation of various clotting factors, such as factor VII and factor X, as well as for platelet activation and aggregation [4]. Studies have shown that patients with parathyroid adenoma have increased protein S activity and fibrinogen levels [5].
This puts patients with PHPT in a hypercoagulable state, therefore possibly multiplying the risk of thrombotic events, including pulmonary embolism (PE). While the incidence of PE in the UK is estimated to be around eight per 10,000 individuals annually [6], the association between PHPT-induced hypercalcemia and PE remains an area of interest and ongoing investigation. Understanding the potential link between hypercalcemia and PE in patients with PHPT is crucial for early recognition, diagnosis, and appropriate management of this rare but serious complication. In this case series, we present two challenging cases of PHPT-induced hypercalcemia and explore its potential association with PE.
| Case Reports | ▴Top |
Case 1
The first case is an 82-year-old male who presented to the emergency department (ED) with left knee pain and difficulty to mobilize due to a fall. His past medical history included stroke, deep vein thrombosis (DVT) and very high risk of falls and fractures. Prior to this incident, the patient was independent, mobilizing with a stick and living with his wife. Atorvastatin and apixaban were the two regular medications he was taking.
On examination he was unable to weight bear with his left leg, had reduced leg extension and a swollen left knee. He was pyrexial and had raised inflammatory markers. Initial investigations showed hypercalcemia with calcium levels of 2.9 (normal reference range: 2.1 - 2.6 mmol/L) and raised PTH with levels of 15.7 (reference range: 1.6 - 6.9 pmol/L) (Table 1). Following a computed tomography of chest/abdomen/pelvis (CT CAP), multiple incidental findings came to light: parathyroid nodule suspicious of adenoma (Fig. 1), intracapsular left neck of femur fracture (Fig. 2) and acute small volume PE (Fig. 3). In view of the findings, the patient had a left hip hemiarthroplasty, was started on therapeutic dose low-molecular-weight heparin (LMWH) (dalteparin) for PE, then switched to apixaban. The diagnosis of hyperparathyroidism was made in light of the presence of parathyroid adenoma, raised urinary calcium/creatinine ratio, as well as high level of calcium and PTH. Patient was referred to the ear, nose and throat (ENT) department to be assessed and found not suitable for surgery and advised to manage medically, in consideration of multiple comorbidities and frailty. He was discharged with an endocrinology follow-up.
 Click to view | Table 1. PTH, Adjusted Calcium, Calcium-Creatinine Ratio and Vitamin D Levels for Both Cases |
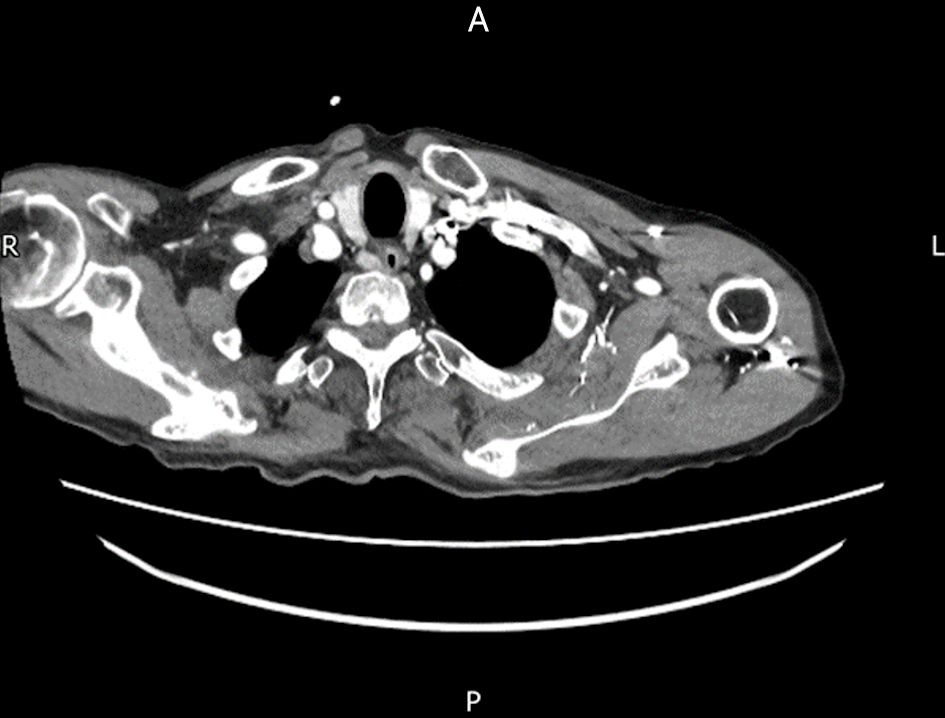 Click for large image | Figure 1. Axial view of computed tomography (CT) scan showing parathyroid nodule suspicious of adenoma. |
 Click for large image | Figure 2. Sagittal view of computed tomography (CT) scan showing left intracapsular neck of femur fracture (yellow arrow). |
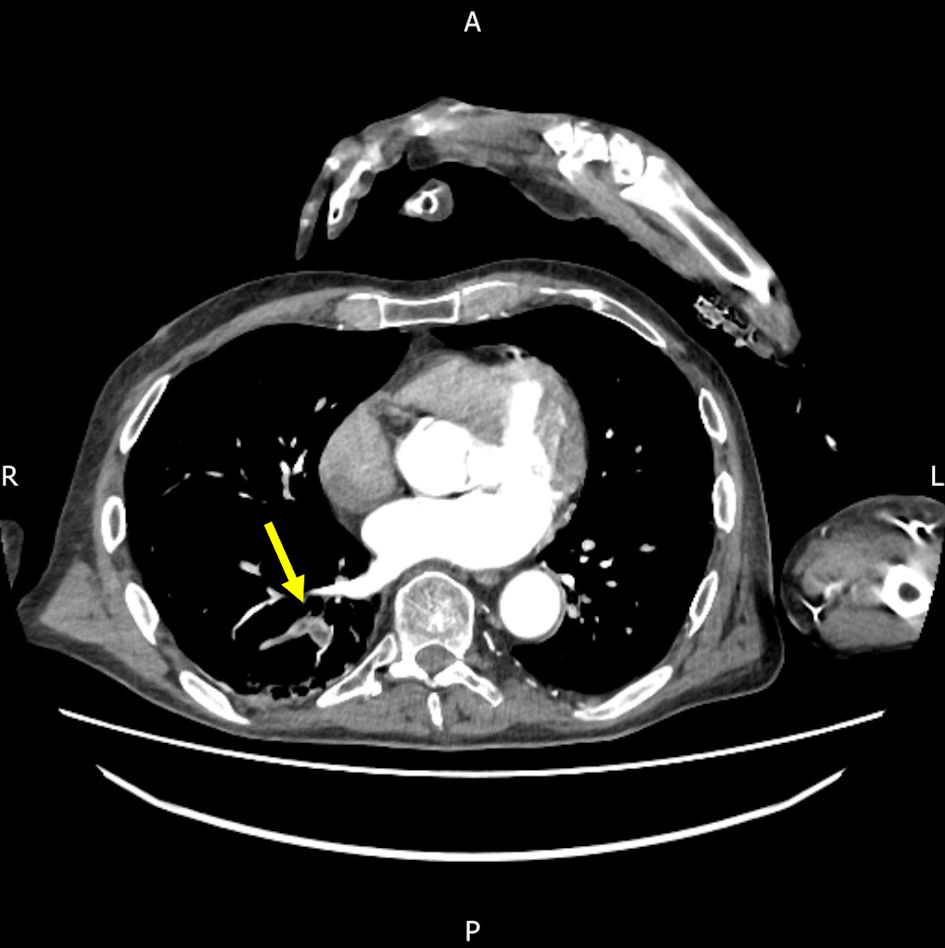 Click for large image | Figure 3. Axial view of computed tomography (CT) scan showing incidental finding of acute small volume PE in the right lobe (yellow arrow). PE: pulmonary embolism. |
Case 2
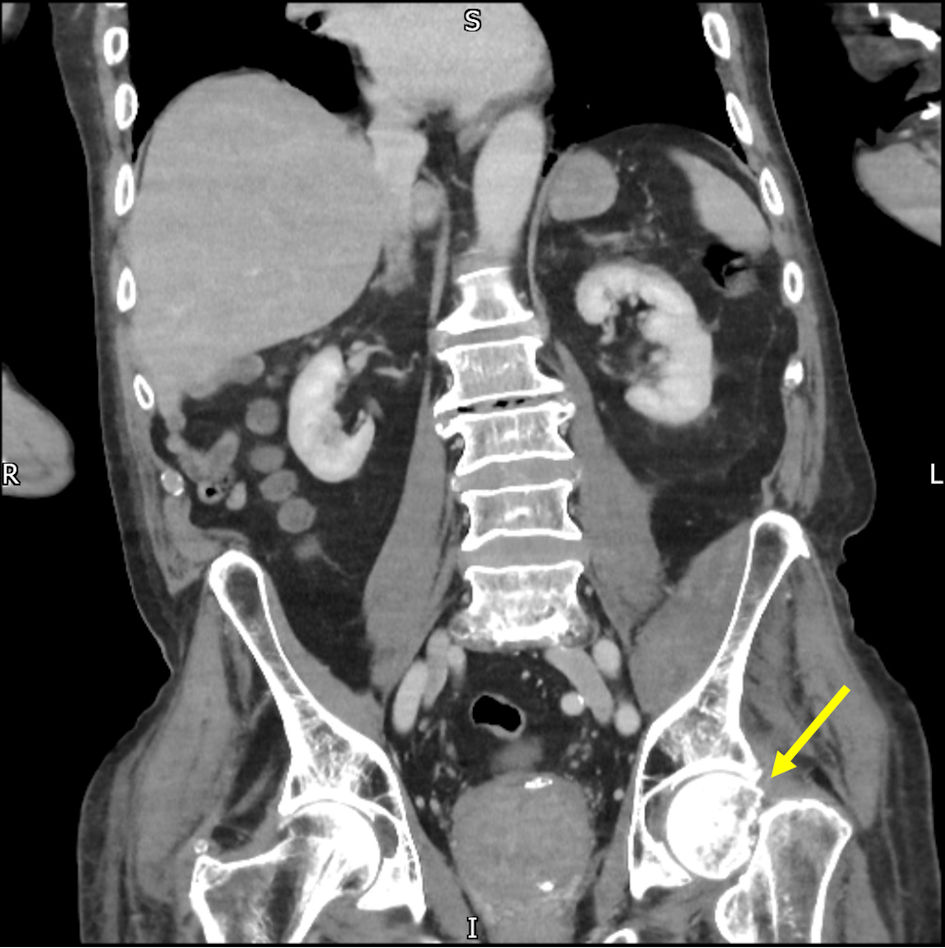
The second patient, a 77-year-old female, presented to the ED with right hip pain following a fall on ice. Examination revealed external rotation of the right leg. A plain radiograph and subsequent CT scan confirmed an impacted right subcapital proximal femoral fracture (Fig. 4). Further preoperative evaluation through magnetic resonance imaging (MRI) confirmed the fracture diagnosis with no lytic lesions (Fig. 5).
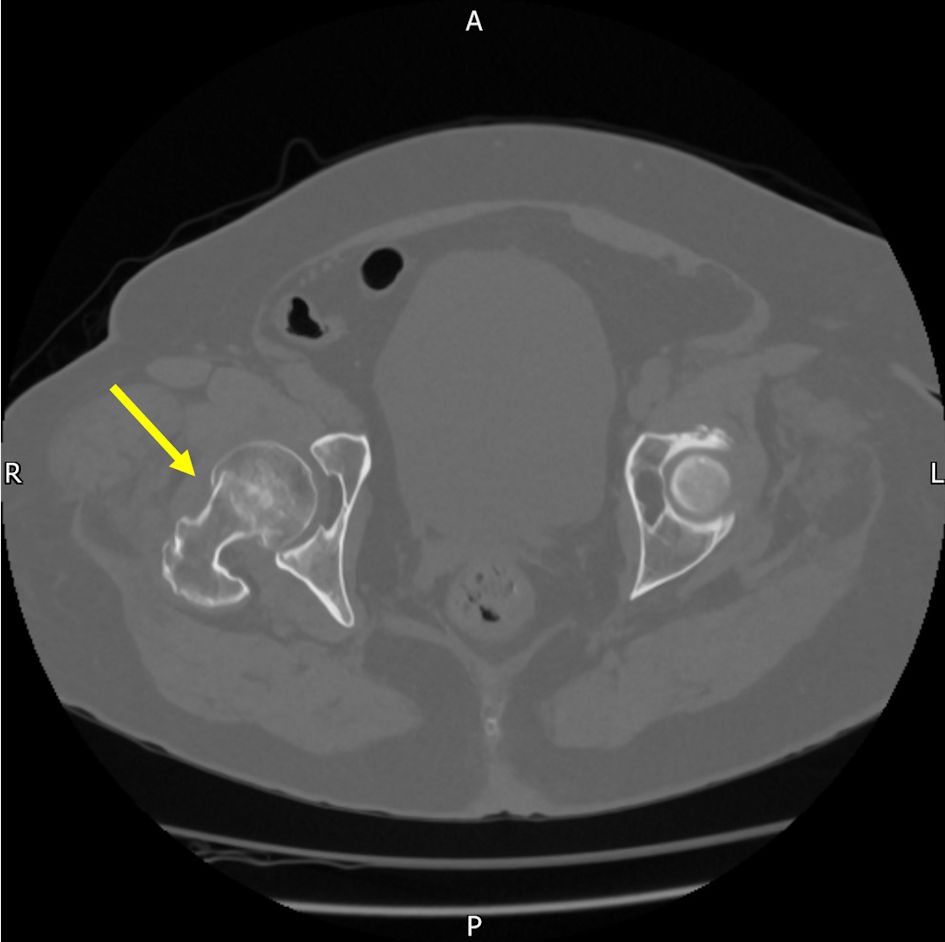 Click for large image | Figure 4. Subcapital proximal femoral fracture of the neck of the femur (yellow arrow) in computed tomography (CT) scan. |
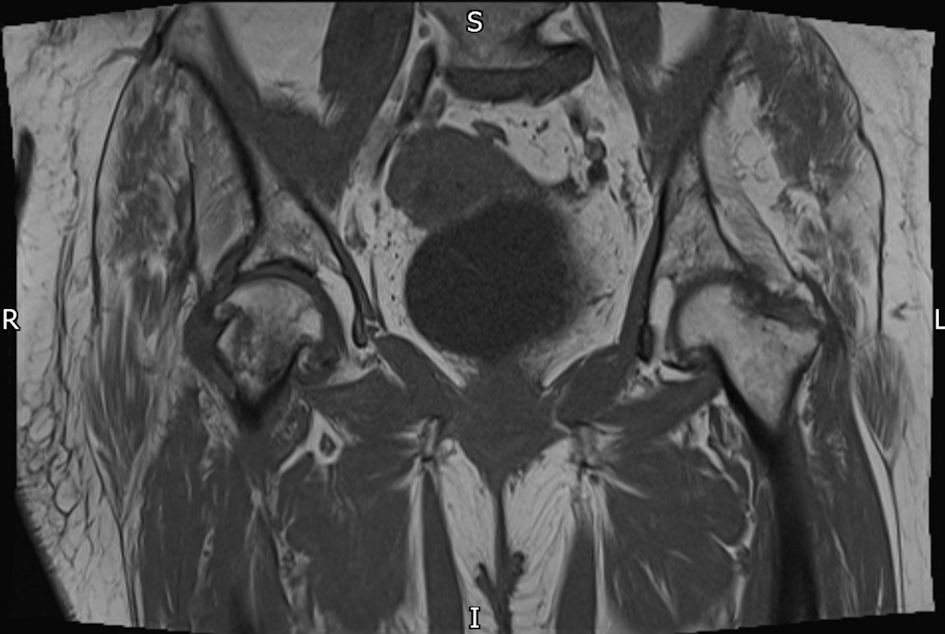 Click for large image | Figure 5. MRI confirming fracture diagnosis of right neck of femur with no lytic lesions. MRI: magnetic resonance imaging. |
The patient’s medical history included hypertension, multiple episodes of DVT treated with edoxaban, hypothyroidism, and breast cancer managed with letrozole and adjuvant radiotherapy in 2019. A hemi-arthroplasty was planned for the patient. During the perioperative workup, hypercalcemia was detected, raising concerns about an underlying malignancy as the possible cause. A CT CAP scan was performed, revealing bilateral lower lobe PE without evidence of malignancy (Fig. 6). Intraoperative histology samples of the head of the right femur did not indicate any malignancy.
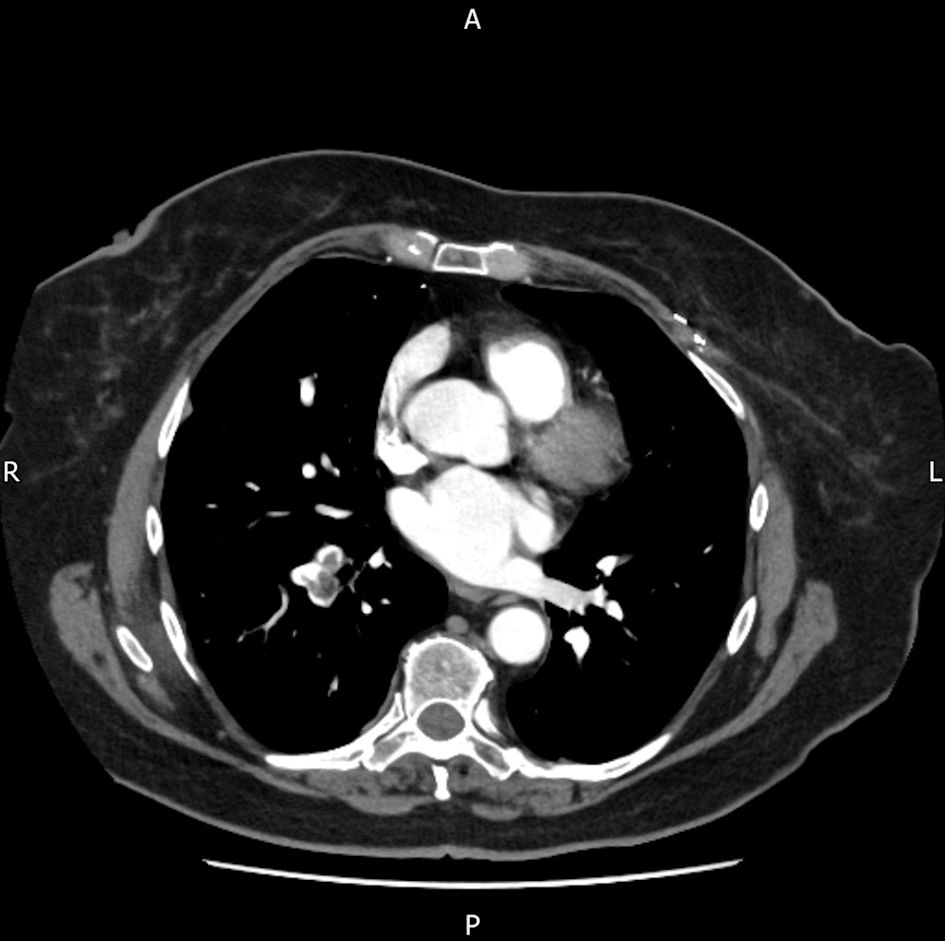 Click for large image | Figure 6. A CT chest/abdomen/pelvis scan was performed, revealing bilateral lower lobe pulmonary emboli without evidence of malignancy. CT: computed tomography. |
Treatment for the PE included LMWH, with discontinuation of edoxaban. To address hypercalcemia, the patient was advised to discontinue calcium supplements and increase oral fluid intake. Referral to the endocrinology department was made due to suspicion of PHPT based on the blood test results (Table 1). Following fracture treatment, the patient recovered well. Calcium levels are being monitored by the primary care physician, and calcium supplementation was discontinued. The hematology clinic conducted a thrombophilia screen, which showed negative anticardiolipin and beta-2 glycoprotein 1 antibodies, normal protein C and protein S levels, and no evidence of factor V Leiden or prothrombin gene mutations. At yearly follow-up, the patient demonstrated good mobility without signs of PE recurrence or hypercalcemia.
| Discussion | ▴Top |
This case series explores the potential association between PHPT and PE in patients with a fracture of the neck of the femur, a subject that, despite being understudied, may have important effects on patient care. By examining two elderly patients who presented with a fracture of the neck of the femur and were subsequently found to have high calcium, high PTH, and high urinary calcium levels indicative of PHPT, we have uncovered clinical presentations that support the pre-existing body of research that suggests a potential link between these two illnesses. Both patients developed PE postoperatively, diagnosed via CT imaging.
The potential for improved patient outcomes through early detection and care, should a solid link be unquestionably proven, highlights the significance of this work. We will explore the potential relevance of our findings, interpret them, and examine how they fit with existing medical knowledge in this debate.
From the late 20th century, evidence has suggested possible connections between hypercalcemia and an increased risk of thromboembolic events. A study published in 1979 demonstrated that hypercalcemia could lead to a hypercoagulable state and therefore, increase the risk of thromboembolic diseases [7]. Further to this, Gorelick et al reported six patients with hypercalcemia among 502 stroke patients in the mid-1980s, all of whom had elevated PTH levels, having said that, parathyroid adenoma and hyperplasia were detected in only two cases [8]. These findings suggested that hypercalcemia, often a result of PHPT, could have significant vascular implications.
A study conducted in 2008 provides further evidence supporting the presence of a hypercoagulable state in patients with PHPT. It was observed that there were increased platelet count, factor VII and factor X activities, as well as elevated D-dimer levels in patients with PHPT, compared to healthy controls [9]. These findings suggest that the hypercoagulable state associated with PHPT may heighten the risk of atherosclerotic and atherothrombotic complications, potentially contributing to the elevated mortality rate attributed to cardiovascular disease in patients with PHPT. Moreover, a separate study from 2021 provides similar support for this conclusion. It indicates that hyperparathyroidism can induce a hypercoagulable state, which can be successfully assessed using modified rotation thermoelectrometry [10]. Considering these findings, it is plausible to infer that the hypercoagulable state linked with PHPT could have contributed to the development of PE in our patients, especially in the presence of a fractured neck of the femur. In more recent investigations into the coagulation profile of PHPT patients, abnormal coagulation tests have been reported, and coagulopathy has been frequently linked with hyperparathyroidism secondary to vitamin D deficiency [11]. These reports further support the hypothesis of a potential hypercoagulable state in patients with hyperparathyroidism in line with the findings presented in this case series. Factors such as reduced mobility, multimorbidity, and the presence of cancer can significantly impact the risk of thrombosis in patients [12]. Additional considerations include weight, gender, the development of frailty, and calciphylaxis [13]. Moreover, PTH levels tend to increase with age [14], which may further enhance the hypercoagulability risk in elderly patients with PHPT.
An additional proposed mechanism contributing to the hypercoagulability observed in PHPT is the direct activation of platelets induced by elevated calcium levels. Studies have suggested that increased calcium can directly trigger platelet activation, leading to platelet aggregation and clot formation. This calcium-induced platelet activation further exacerbates the prothrombotic state associated with PHPT [15, 16]. Nevertheless, it is essential to acknowledge that some studies have reported conflicting findings regarding the impact of PHPT or secondary hyperparathyroidism (SHPT) and serum calcium levels on platelet functions, specifically when evaluated through aggregation tests [17]. These inconsistent results indicate a potential variation in the relationship between PTH, hypercalcemia, and platelet function. This may suggest the need for more research to explore whether bone fracture in association with hypercalcemia may lead to an increase in activation of platelets and hence risk of coagulation. Moreover, calcium is crucial for vascular smooth muscle cell activity and can help prevent altered blood flow patterns. These altered patterns are often associated with hypercoagulability due to flow disruption and the release of prothrombotic substances by the endothelium [18].
Importantly, the “Tromso Study” which included 27,712 subjects, showed that high levels of both calcium and PTH were associated with an increased risk of VTE compared to subjects with normal levels [19]. It is significant to note that both our patients had a history of DVT and experienced PE. Interestingly, in case series of three patients, it was shown that surgical treatment of hyperparathyroidism was associated with significant decrease in recurrence of thrombotic events (stroke, PE, DVT) [20]. The unique part in our case series is the fact that the presence of a fractured neck of femur in association with hypercalcemia led to the association of the development of PE. Several studies showed an increased tendency of risk of coagulation in elderly patients with a fractured neck of femur [21-23].
Conclusions
Further research is needed to 1) establish whether chronic hypercalcemia in absence of fracture can modulate the risk of hypercoagulation; and 2) whether chronic hypercalcemia in individuals with bone fracture may represent significant hypercoagulability risk during the postoperative periods. The potential interplay between bone fracture, hypercalcemia, comorbidities, and high PTH is shown in Figure 7.
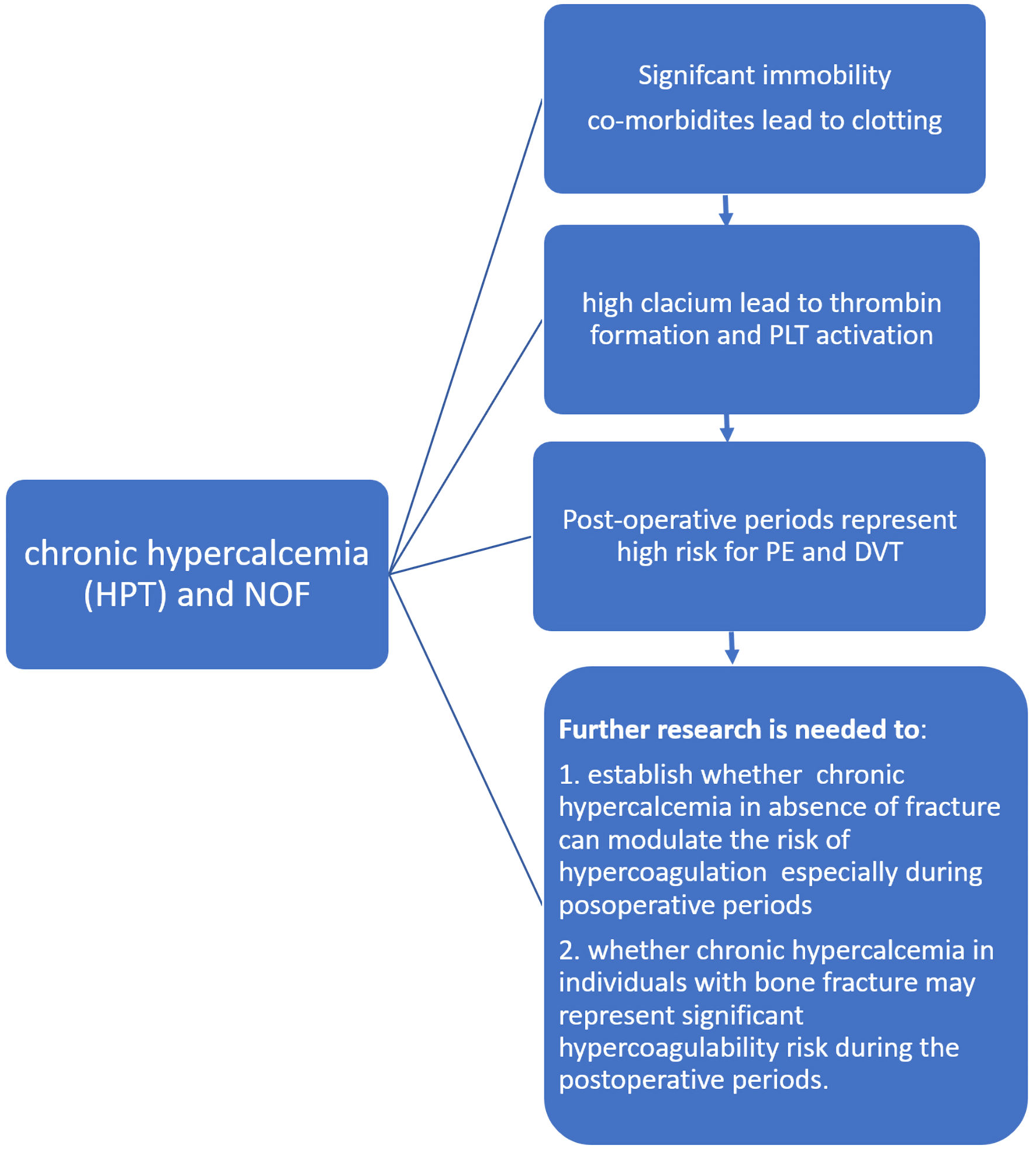 Click for large image | Figure 7. The potential interplay between bone fracture, hypercalcemia, comorbidities, and high PTH. DVT: deep vein thrombosis; PE: pulmonary embolism; HPT: hyperparathyroidism: PLT: platelets; NOF: fracture neck of femur; PTH: parathyroid hormone. |
Learning points
Despite the fact that hypercalcemia is not frequently acknowledged as a characteristic precipitant of venous thrombotic events, our case series emphasizes the significance of taking it into account in patients with bone fracture who come with thrombotic symptoms, such as PE. As a result, we recommend including checks for thromboembolic events in the evaluation of patients who are diagnosed with PHPT and other chronic causes of hypercalcemia admitted to orthopedic wards. Additionally, calcium levels, particularly ionized calcium, should be measured in all elderly patients with hip fractures.
This proactive strategy makes it easier to identify potential thrombotic risks quickly and to start taking precautions through simple measures such intravenous or oral rehydration.
Acknowledgments
Yashar Mashayekhi and Sara Baba-Aissa are grateful for their parents for their unlimited support during their study at the Medical School in the University of Buckingham, UK. The first case was presented in the Endobridge conference in Istanbul, Turkey (2023), and only abstract was published (Yashar Mashayekhi, Sara Baba-Aissa, Amina Adil Al-Qaysi, Henry Owles, Maria Panourgia, Mohamed H. Ahmed, P-11 Case report of Primary Hyperparathyroidism and PE, JCEM Case Reports, Volume 2, Issue Supplement_1, January 2024, luad146.016).
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent has been obtained from the patients.
Author Contributions
Conception and design: MHA. Administrative support: all authors. Provision of study materials or patients: all authors. Collection and assembly of data: MHA, YM, and SBA. Data analysis and interpretations, manuscript writing, and final approval of manuscript: all authors.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Guideline scope Hyperparathyroidism (primary): diagnosis, assessment and initial management [Internet]. Available from: https://www.nice.org.uk/guidance/ng132/documents/final-scope.
- Taniegra ED. Hyperparathyroidism. Am Fam Physician. 2004;69(2):333-339.
pubmed - Lofrese JJ, Basit H, Lappin SL. Physiology, parathyroid. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Mikaelsson ME. The role of calcium in coagulation and anticoagulation. Coagulation and Blood Transfusion. 1991;29-37.
- Alay M, Ercek BM, Sonmez GM, Sakin A, Ucler R, Yildiz S. Evaluation of coagulation parameters in patients with parathyroid adenoma. Sci Rep. 2020;10(1):19208.
doi pubmed pmc - Appendix B National Institute for Health and Clinical Excellence Final scope for the appraisal of Rivaroxaban for the treatment of PE and the prevention of recurrent venous thromboembolism [Internet]. 2012. Available from: https://www.nice.org.uk/guidance/ta287/documents/pulmonary-embolism-acute-treatment-vte-prevention-rivaroxaban-appendix-b-final-scope2#:∼:text=The%20annual%20incidence%20of%20venous.
- Bostrom H, Alveryd A. Stroke in hyperparathyroidism. Acta Med Scand. 1972;192(4):299-308.
doi pubmed - Gorelick PB, Sloan MA. Calcium, hypercalcemia, magnesium, and brain ischemia [Internet]. 2nd ed. Bogousslavsky J, Caplan LR, editors. Cambridge: Cambridge University Press; 2008. p. 357-364. [cited Jun 11, 2023] Available from: https://www.cambridge.org/core/books/abs/uncommon-causes-of-stroke/calcium-hypercalcemia-magnesium-and-brain-ischemia/CEB1A615C5FD8D80AEC71FB338E17E8C.
- Erem C, Kocak M, Hacihasanoglu A, Yilmaz M, Saglam F, Ersoz HO. Blood coagulation, fibrinolysis and lipid profile in patients with primary hyperparathyroidism: increased plasma factor VII and X activities and D-Dimer levels. Exp Clin Endocrinol Diabetes. 2008;116(10):619-624.
doi pubmed - Yorulmaz G, Kalkan AT, Akalin A, Alaguney ES, Gunduz E, Badak B, Buyruk BA, et al. Effect of hyperparathyroidism on coagulation: a global assessment by modified rotation thromboelastogram (ROTEM). Turk J Med Sci. 2021;51(6):2897-2902.
doi pubmed pmc - Elbers LPB, Wijnberge M, Meijers JCM, Poland DCW, Brandjes DPM, Fliers E, Gerdes VEA. Coagulation and fibrinolysis in hyperparathyroidism secondary to vitamin D deficiency. Endocr Connect. 2018;7(2):325-333.
doi pubmed pmc - Engbers MJ, Blom JW, Cushman M, Rosendaal FR, van Hylckama Vlieg A. The contribution of immobility risk factors to the incidence of venous thrombosis in an older population. J Thromb Haemost. 2014;12(3):290-296.
doi pubmed - Nigwekar SU, Thadhani R, Brandenburg VM. Calciphylaxis. N Engl J Med. 2018;378(18):1704-1714.
doi pubmed - Hadlow NC, Brown S, Wardrop R, Henley D. The effects of age, adiposity, and physical activity on the risk of seven site-specific fractures in postmenopausal women. J Bone Miner Res. 2017;32(1):157-166.
- Cabrera D, Walker K, Moise S, Telling ND, Harper AGS. Controlling human platelet activation with calcium-binding nanoparticles. Nano Res. 2020;13(10):2697-2705.
doi pubmed pmc - Howard MR, Ashwell S, Bond LR, Holbrook I. Artefactual serum hyperkalaemia and hypercalcaemia in essential thrombocythaemia. J Clin Pathol. 2000;53(2):105-109.
doi pubmed pmc - Yorulmaz G, Akalin A, Akay OM, Sahin G, Bal C. The effect of hyperparathyroid state on platelet functions and bone loss. Turk J Haematol. 2016;33(4):293-298.
doi pubmed pmc - Amberg GC, Navedo MF. Calcium dynamics in vascular smooth muscle. Microcirculation. 2013;20(4):281-289.
doi pubmed pmc - Lerstad G, Brodin EE, Svartberg J, Jorde R, Brox J, Braekkan SK, Hansen JB. Associations between serum levels of calcium, parathyroid hormone and future risk of venous thromboembolism: the Tromso study. Eur J Endocrinol. 2017;176(5):625-634.
doi pubmed - Koufakis T, Antonopoulou V, Grammatiki M, Karras SN, Ajjan R, Zebekakis P, Kotsa K. The Relationship between primary hyperparathyroidism and thrombotic events: report of three cases and a review of potential mechanisms. Int J Hematol Oncol Stem Cell Res. 2018;12(3):175-180.
pubmed pmc - Xia ZN, Xiao K, Zhu W, Feng B, Zhang BZ, Lin J, Qian WW, et al. Risk assessment and management of preoperative venous thromboembolism following femoral neck fracture. J Orthop Surg Res. 2018;13(1):291.
doi pubmed pmc - Wu L, Cheng B. Analysis of perioperative risk factors for deep vein thrombosis in patients with femoral and pelvic fractures. J Orthop Surg Res. 2020;15(1):597.
doi pubmed pmc - Song K, Yao Y, Rong Z, Shen Y, Zheng M, Jiang Q. The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Arch Orthop Trauma Surg. 2016;136(10):1459-1464.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


