| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 8, August 2024, pages 167-170
Wake-Up Thrombolysis With Negative Diffusion-Weighted Magnetic Resonance Imaging
Huma Manjraa, c, Vishal Sambojub, Navdeep Sanghab
aKaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, CA, USA
bDepartment of Neurology, Los Angeles Medical Center, Kaiser Permanente, Los Angeles, CA, USA
cCorresponding Author: Huma Manjra, Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, CA, USA
Manuscript submitted May 4, 2024, accepted June 24, 2024, published online July 18, 2024
Short title: Wake-Up Thrombolysis With Negative DWI MRI
doi: https://doi.org/10.14740/jmc4241
| Abstract | ▴Top |
This case underscores the importance of treating neurological deficits of an acute stroke presentation despite initial negative diffusion-weighted imaging (DWI), especially in the acute phase when there is high clinical suspicion of stroke. Additionally, it highlights the appropriate use of a WAKE-UP protocol for patients that present with stroke symptoms without a well-defined inception time. A 71-year-old female presented to the emergency department with symptoms of dizziness and double vision upon wake-up. While clinical exam findings revealed left intranuclear ophthalmoplegia (INO) and inability to ambulate due to gait ataxia, magnetic resonance imaging (MRI) was negative for acute stroke. Despite negative DWI MRI, this patient’s clinical exam findings of a left INO and gait ataxia were indicative of an ischemic stroke localizing to the medial longitudinal fasciculus (MLF), and the patient received thrombolytics. Repeat MRI about 48 h later revealed an acute infarct in the left midbrain with a DWI lesion in the MLF.
Keywords: Wake-up thrombolysis; Ischemic stroke; Diffusion-weighted MRI; Medial longitudinal fasciculus
| Introduction | ▴Top |
Brain stem strokes in the acute phase can present with a negative diffusion-weighted imaging (DWI) magnetic resonance imaging (MRI) [1]. However, physical exam findings of left intranuclear ophthalmoplegia (INO) and gait ataxia can be indicative of an ischemic stroke warranting treatment of neurological deficits. The WAKE-UP study deemed patients eligible for thrombolytics if there was not a well-defined inception time of stroke, the patient presented within 4.5 h of symptom discovery, and if there was a mismatch between the presence of a DWI and absence of fluid-attenuated inversion recovery (FLAIR) changes on MRI. This protocol relies on the assumption that less than 4.5 h have passed since the patient’s symptoms began, if there are no corroborating findings of FLAIR changes on the MRI [2]. Given that patients can have negative DWI in the acute setting, it should not preclude them from receiving thrombolytics if their neurological examination is consistent with a focal neurological phenomenon due to an acute stroke, and if they present within 4.5 h of symptom discovery.
| Case Report | ▴Top |
Investigations
A 71-year-old female with a past medical history of hyperlipidemia and hypertension presented to the emergency department with symptoms of dizziness and double vision that occurred at 6:00 am upon waking up. Her last known well time was 4:00 am of the same morning when she arose to use the restroom. The patient presented to the emergency department and was seen by the stroke team. A code stroke was initiated, but by the time the patient’s non-contrast computed tomography of the head (CTH) and computed tomography angiography (CTA) of the head and neck were completed, and the case was discussed with the attending stroke neurologist, the patient was beyond 4.5 h from the last known well time. On exam, the patient demonstrated medial gaze palsy of the left eye and inability to ambulate due to gait ataxia. Vital signs were notable for a blood pressure of 201/108 mm Hg and labs were grossly unremarkable. On the exam the patient scored a National Institutes of Health Stroke Score (NIHSS) of 1 for partial gaze palsy, however, the patient had dense gait ataxia and was unable to ambulate.
Diagnosis
The CTH did not show evidence of an intracranial hemorrhage or other hypodensity suggesting completed infarction, indicating no absolute radiographic contraindications for lytic administration, and the CTA did not demonstrate any large vessel occlusion or major steno-occlusive disease. Given the symptom discovery was 4.5 h from the last seen normal but within 4.5 h of symptoms discovery, MRI was obtained to evaluate for candidacy for thrombolytics. The MRI was performed under a WAKE-UP stroke protocol which deems candidates amenable to receiving thrombolytics if there is a mismatch between the presence of a DWI lesion and absence of FLAIR changes on MRI. The MRI was negative for both diffusion restriction and FLAIR changes (Fig. 1).
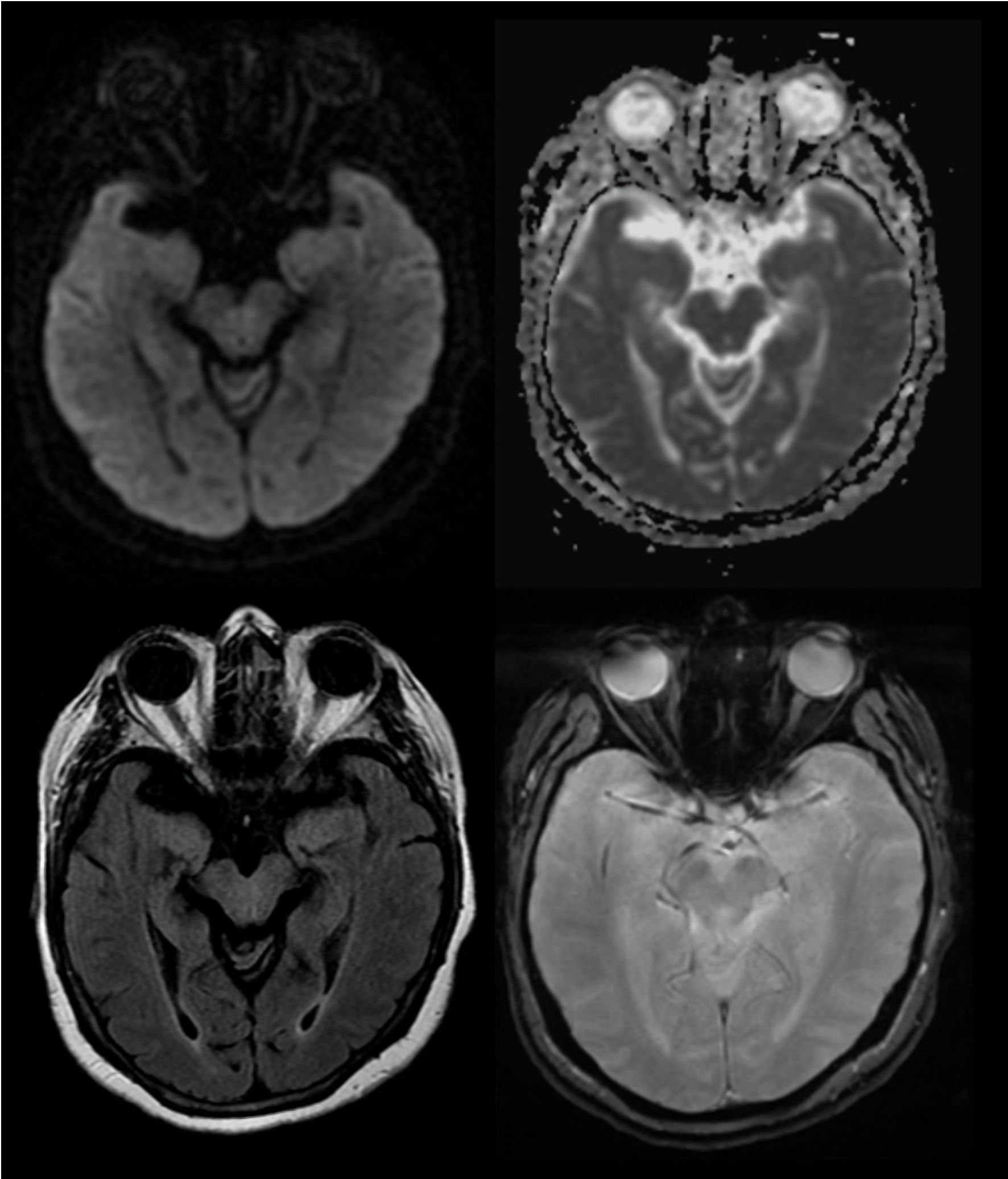 Click for large image | Figure 1. MRI upon presentation. The MRI shows no evidence of acute ischemic stroke on DWI (top left) or FLAIR lesion (bottom left). Pictured in the top right is the ADC and the bottom right is the GRE. MRI: magnetic resonance imaging; DWI: diffusion-weighted imaging; FLAIR: fluid-attenuated inversion recovery; ADC: apparent diffusion coefficient; GRE: gradient echo sequence. |
Treatment
Despite both CT and MRI being negative for acute stroke, the patient’s clinical exam findings of acute INO and gait ataxia clinically suggested an ischemic stroke localizing well to the medial longitudinal fasciculus (MLF). The risk and benefits of thrombolysis based on the WAKE-UP study were discussed with the patient who agreed to proceed with thrombolysis [2].
Follow-up and outcomes
The patient was admitted to the intensive care unit (ICU) for further monitoring. A repeat CTH was obtained which was negative for new hemorrhage. Additionally, about 48 h later a repeat MRI of the brain and brainstem revealed an acute infarct in the left midbrain with a DWI lesion in the left MLF (Fig. 2). Residually, the patient had some trouble opening her left eyelid and some blurred vision in the left eye at ophthalmology follow-up. Her gait ataxia improved significantly, and she could ambulate over 200 feet without assistive devices. The patient’s 90 day modified Rankin Scale was a 0.
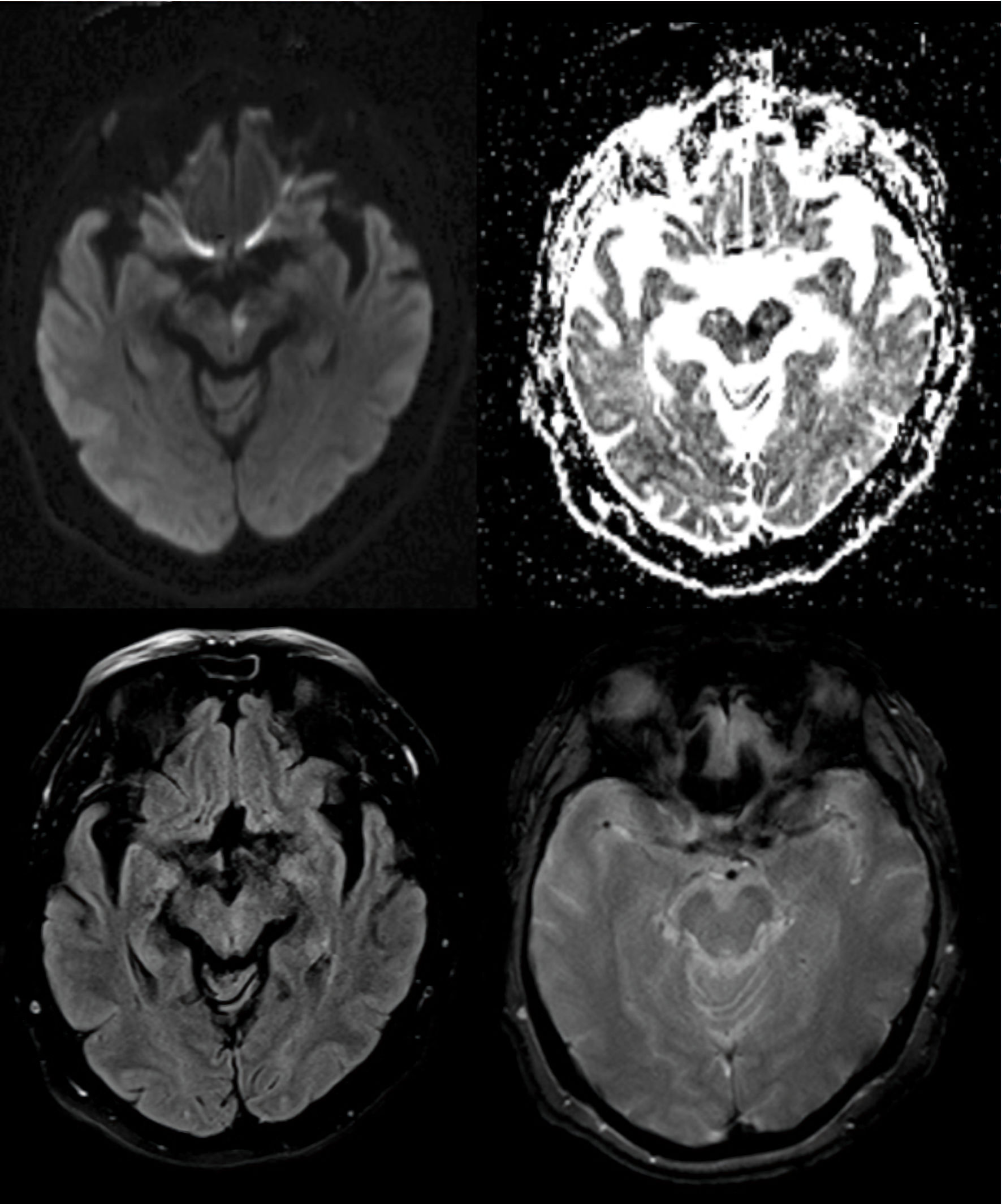 Click for large image | Figure 2. MRI 48 h post presentation. Abnormal MRI now shows a left MLF lesion on the DWI (top left) with an ADC correlate (top right) as well as a faint FLAIR abnormality (bottom left). Absence of any post thrombolytic hemorrhage is noted on the GRE (bottom right). MRI: magnetic resonance imaging; MLF: medial longitudinal fasciculus; DWI: diffusion-weighted imaging; FLAIR: fluid-attenuated inversion recovery; ADC: apparent diffusion coefficient; GRE: gradient echo sequence. |
| Discussion | ▴Top |
INO and gait ataxia is indicative of an ischemic stroke localizing to the MLF [3]. This case report identifies a patient who presented with a left INO without corresponding findings on imaging, but clinical stroke syndrome warranting thrombolytics through utilization of a WAKE-UP protocol. This case describes a discrepancy between the most sensitive imaging modality available for stroke compared to clinical exam in the acute phase, reinforcing the value of clinical correlation. Few studies have documented the capture of an acute phase of stroke with negative MRI findings. Furthermore, less studies have effectively documented thrombolysis in these situations. Our study highlights the value of clinical exam findings, which may show discrepancies with an MRI negative for acute infarction. Prior literature describes varying rates ranging from 0-21% or more for similar discrepancies. An analysis involving 401 patients conducted by Sylaja et al [4], showed 25.6% of the participants with stroke deficits demonstrated DWI MRI negative imaging. Many of these cases of false-negative DWI MRI occurred in patients with brain stem strokes, such as our patient described above. A separate study by Krasnianski et al [1], also showed similarly negative findings on MRI with brainstem stroke syndromes in 8/30 patients. Additionally, in a retrospective analysis by Lovblad et al [5], 194 cases of acute ischemic stroke were diagnosed clinically within 24 h of onset and studied with DWI MRI. Results showed a moderate negative predictive value of 69.5%, indicating that DWI MRI negative imaging did not sufficiently rule out a stroke diagnosis. Similar to Sylaja et al [4] and Krasnianski et al [1], Lovblad et al [5] showed that most of the false negative findings were in patients with resolving deficits localized to the brain stem.
Another study conducted by Oppenheim et al [6], showed that eight out of 139 patients presented with an initial negative DW MRI despite presentation of acute neurological deficit. These eight patients had a final diagnosis of stroke after a positive follow-up MRI corroborated the clinical exam findings. Limitations of the MRI suggested by the paper refer to lesions that can be too small for clear resolution, sub-optimal signal-to-noise ratio, and blurry image analysis due to brain stem distortions. Slice interpolation can also contribute to missing information between slices. Similarly, the limitations of our study include the use of a 1.5-T magnet, which can be less sensitive to detect small lesions/infarctions. Furthermore, only one patient was studied in this case report, and it would benefit from further review of patients who received MRI in the acute phase to provide supportive evidence. Other limitations include that our case report did not utilize perfusion-weighted imaging, which has been utilized to identify abnormalities in posterior circulation strokes during early phases [7].
Conclusions
This case is unique in that the protocol for thrombolysis for patients with discovered or wake-up symptoms, based on the WAKE-UP study, requires the presence of a DWI lesion and the absence of a FLAIR lesion. We advocate to proceed with thrombolysis even if the DWI is negative, but the exam and history are consistent with a focal neurological deficit likely from a stroke in such discovered/wake-up patients, because the DWI may be falsely negative in the acute setting. In summary, our case illustrates the importance of treating neurological deficits of an acute stroke presentation despite negative DWI MRI, especially in the acute phase when there is high clinical suspicion of stroke (particularly brainstem strokes). Additionally, it also highlights the appropriate use of a WAKE-UP protocol for stroke that occurs without a well-defined inception time.
Acknowledgments
Our thanks to the Kaiser Permanente Stroke Team.
Financial Disclosure
We have no perceived funding information to disclose.
Conflict of Interest
We have no perceived conflict of interest to disclose.
Informed Consent
The patient’s surrogate has given informed consent for publication of information related to their medical information in this case report.
Author Contributions
Huma Manjra wrote the manuscript. Visha Samboju edited the manuscript. Navdeep Sangha contributed to the study design and edited manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Krasnianski M, Lindner A, Zierz S. Brainstem infarctions with normal MRI. Eur J Med Res. 2002;7(3):125-127.
pubmed - Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B, Cheripelli B, et al. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med. 2018;379(7):611-622.
doi pubmed - Ueno Y, Honda S. A case of traumatic medial longitudinal fasciculus syndrome whose causal lesion was detected by thin-section MRI with susceptibility-weighted imaging. Case Rep Ophthalmol. 2022;13(2):368-373.
doi pubmed pmc - Sylaja PN, Coutts SB, Krol A, Hill MD, Demchuk AM, VISION Study Group. When to expect negative diffusion-weighted images in stroke and transient ischemic attack. Stroke. 2008;39(6):1898-1900.
doi pubmed - Lovblad KO, Laubach HJ, Baird AE, Curtin F, Schlaug G, Edelman RR, Warach S. Clinical experience with diffusion-weighted MR in patients with acute stroke. AJNR Am J Neuroradiol. 1998;19(6):1061-1066.
pubmed pmc - Oppenheim C, Stanescu R, Dormont D, Crozier S, Marro B, Samson Y, Rancurel G, et al. False-negative diffusion-weighted MR findings in acute ischemic stroke. AJNR Am J Neuroradiol. 2000;21(8):1434-1440.
pubmed pmc - Choi JH, Oh EH, Park MG, Baik SK, Cho HJ, Choi SY, Lee TH, et al. Early MRI-negative posterior circulation stroke presenting as acute dizziness. J Neurol. 2018;265(12):2993-3000.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


