| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 9, September 2024, pages 227-230
Bilio-Cecal Stent Migration Presenting as Massive Rectal Bleeding
Lefika Bathobakaea, f, Shady Gerisa, Mohita Jariwalab, Mansi Patelb, Jessica Escobarc, Ruhin Yuridullahd, Kamal Amerd, Yana Cavanaghd, e
aInternal Medicine, St. Joseph’s University Medical Center, Paterson, NJ, USA
bRowan University School of Osteopathic Medicine, Stratford, NJ, USA
cHealth Sciences Library, St. Joseph’s University Medical Center, Paterson, NJ, USA
dGastroenterology and Hepatology, St. Joseph’s University Medical Center, Paterson, NJ, USA
eAdvanced and Surgical Endoscopy, St. Joseph’s University Medical Center, Paterson, NJ, USA
fCorresponding Author: Lefika Bathobakae, Internal Medicine, St. Joseph’s University Medical Center, Paterson, NJ 07503, USA
Manuscript submitted June 1, 2024, accepted July 10, 2024, published online August 10, 2024
Short title: Bilio-Cecal Stent Migration
doi: https://doi.org/10.14740/jmc4262
| Abstract | ▴Top |
Endoscopic biliary stenting is a well-established intervention for the treatment of biliary, hepatic, and pancreatic disorders. The common indications include strictures, neoplasms, stones, infections, and bile leaks. Stents can be occluded, predisposing patients to ascending cholangitis and biliary sepsis. Distal stent migration is another known complication of endoscopic stenting and is usually spontaneous. Bowel perforation, abscesses, bleeding, and pancreatitis are rare complications of distal stent migration and are usually limited to the duodenum. Herein, we describe an extremely rare case of bilio-cecal stent migration presenting as rectal bleeding.
Keywords: Biliary stent migration; Endoscopic stenting; Rectal bleeding; Cecal impaction; Epigastric pain
| Introduction | ▴Top |
The first case of endoscopic biliary stenting was reported in the 1980s for the management of malignant obstructive jaundice [1]. Since then, biliary stenting has been widely adopted to treat biliary, hepatic, and pancreatic disorders [2-5]. Although rare, biliary stenting may have complications, with stent occlusion and cholangitis being the most common complications [6]. Biliary stent migration is a known, yet infrequent long-term complication of endoscopic stenting and is usually without incident [3]. Most displaced stents find refuge in the duodenum and are passed spontaneously through the rectum [2-4, 6]. Bilio-cecal stent migration and rectal bleeding are exceedingly rare [4] and potentially life-threatening complications. Only a few cases of stent-related rectal bleeding have been reported in the literature [5, 7].
| Case Report | ▴Top |
A 64-year-old male presented to the emergency department (ED) complaining of acute-onset epigastric pain and hematochezia. The patient was discharged a week prior after being admitted for acute gallstone pancreatitis and choledocholithiasis. His medical history was significant for chronic pancreatitis, pancreatic exocrine insufficiency, pancreatic cyst, and pancreatic duct calculi status post stent placement the year prior. During his recent hospitalization, the patient’s blood work was notable for elevated amylase (572 U/L) and carcinoembryonic antigen (CEA) (2,610 ng/mL) levels. An endoscopic ultrasound (EUS) revealed pancreatic duct obstruction in the genu of the pancreas. During endoscopic retrograde cholangiopancreatography (ERCP), the bile duct was deeply cannulated with the Hydratome sphincterotome® (Boston Scientific), and contrast was injected. A filling defect was seen in the lower third of the main bile duct, consistent with stone (Fig. 1). Biliary sphincterotomy was performed with a Hydratome sphincterotome using ERBE electrocautery® (ERBE USA), and there was no post-sphincterotomy bleeding. The ventral pancreatic duct was also deeply cannulated, and contrast was injected. The pancreatic duct in the genu of the pancreas was completely obstructed by a narrowing that did not appear to be a stone or a mass. The biliary tree was swept with a 12-mm balloon starting at the bifurcation and a small amount of pus was observed. Both pus and sludge were swept from the duct. One diminutive stone was also removed, and no stones remained in the biliary tree. One 4-Fr 5-cm plastic stent with a single external flap and no internal flaps was placed into the ventral pancreatic duct. One 10-Fr 9-cm transpapillary plastic stent with a single external flap and a single internal flap was placed into the common bile duct (CBD) (Fig. 1). Once bile flowed through the stent and optimal stent positioning were confirmed, the endoscope was withdrawn from the patient. The next day, a robotic cholecystectomy was performed to prevent future episodes of gallstone pancreatitis, and the patient was discharged with plans for outpatient follow-up with the gastroenterology clinic.
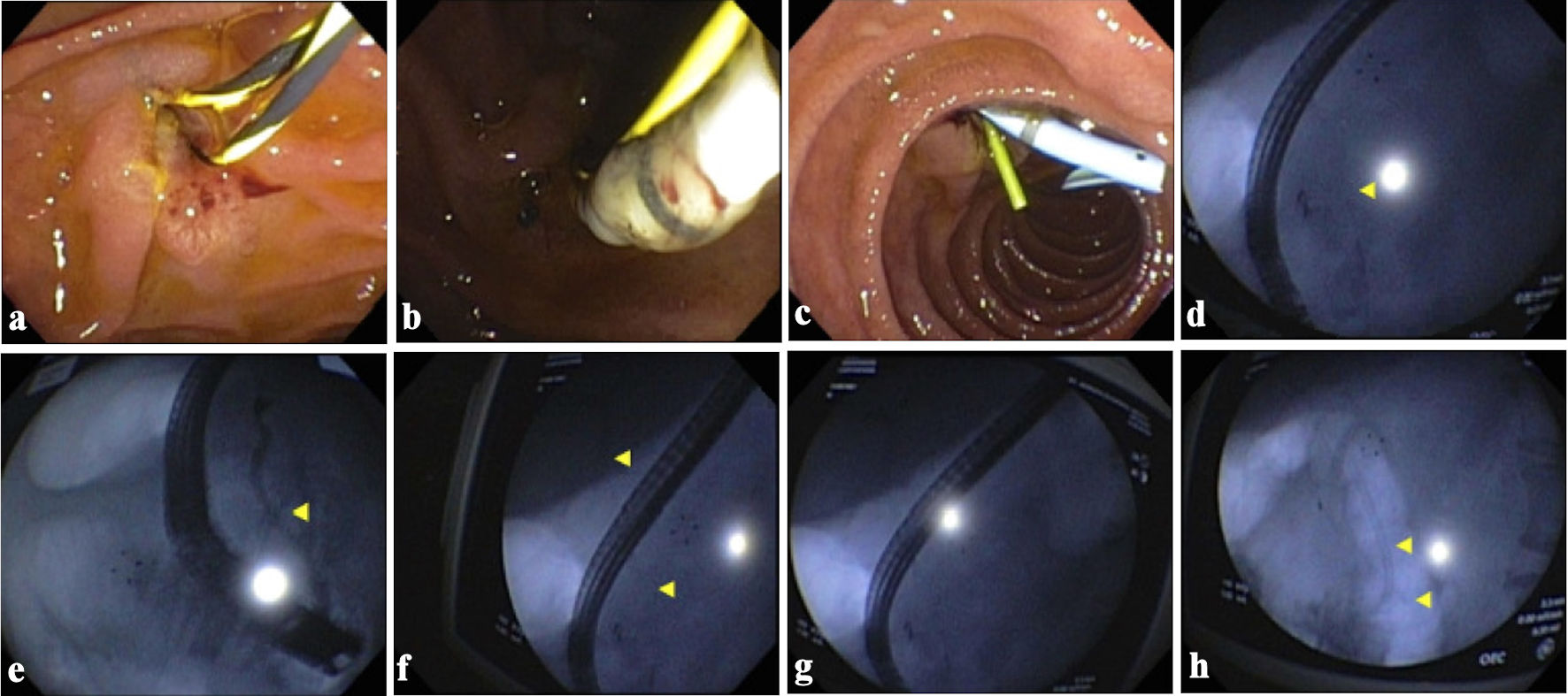 Click for large image | Figure 1. Endoscopic retrograde cholangiopancreatography images showing a filling defect in the biliary duct, sphincterotomy, and stent placement. (a) Image showing a short 0.035-inch soft Jagwire being passed into the biliary tree. (b) Endoscopic image showing a cannulating sphincterotome being inserted into the biliary tree. (c) Image showing a one 4-Fr 5-cm plastic stent with a single external flap and no internal flaps being placed into the common bile duct (CBD)/ventral pancreatic duct (PD). (d) CBD wire. (e) PD w/cutoff a level of genu. (f-h) CBD wire. Yellow arrows in (d-f) show a filling defect consistent with a stone in genu of the pancreas. Yellow arrows in (f) and (h) show a filling defect consistent with a stone as seen on the cholangiogram. w/cutoff: with cutoff. |
On readmission, the patient was extremely pale, diaphoretic, and in acute distress due to abdominal pain. The abdomen was soft, diffusely tender to palpation, but without flank ecchymosis or peritoneal signs. Digital rectal examination demonstrated 200 mL of blackish maroon liquid stool with no palpable masses. The rest of the physical examination was unremarkable. The patient’s initial hemoglobin was 8.6 g/dL, a drop from 12.3 g/dL was observed during his most recent hospitalization. Two hours later, his hemoglobin level dropped again to 5.5 g/dL, and lactate level increased to 6.5 mmol/L. Laboratory values were also notable for a white blood cell count of 15.2 ×103 /mm3, blood glucose level of 914 mg/dL, alkaline phosphatase level of 266 U/L, aspartate aminotransferase (AST) level of 114 U/L, and alanine aminotransferase (ALT) level of 121 U/L. Owing to concerns for a mixed shock state, the patient was empirically started on vancomycin and piperacillin-tazobactam to cover for biliary sepsis. The patient received four units of packed red blood cells (PRBCs) and was transferred to the medical intensive care unit (ICU) for vasopressor support and insulin drip according to the hyperosmolar hyperglycemic syndrome protocol.
The nuclear imaging results were negative for active arterial extravasation. Upper endoscopy revealed a normal esophagus with a non-bleeding gastric ulcer and clean ulcer base. The duodenum and major papillae were normal without evidence of a CBD stent. Colonoscopy performed the next day revealed severe diverticulosis in the sigmoid and descending colon and non-bleeding hemorrhoids. A foreign body was noted in the cecum, which was successfully removed using a snare (Fig. 2). Given the absence of colonic ulceration or stigmata of recent bleeding in the cecum, we hypothesized that the migrated stent lodged in the colonic diverticulum, resulting in localized injury and rectal bleeding. The patient had no further bleeding incidents after the procedure. Hemoglobin level and blood glucose levels normalized, and the patient was discharged on day 7 of admission. At a 2-week follow-up appointment with the gastroenterology clinic, the patient denied melena, hematochezia, or hematemesis, and his hemoglobin level was stable.
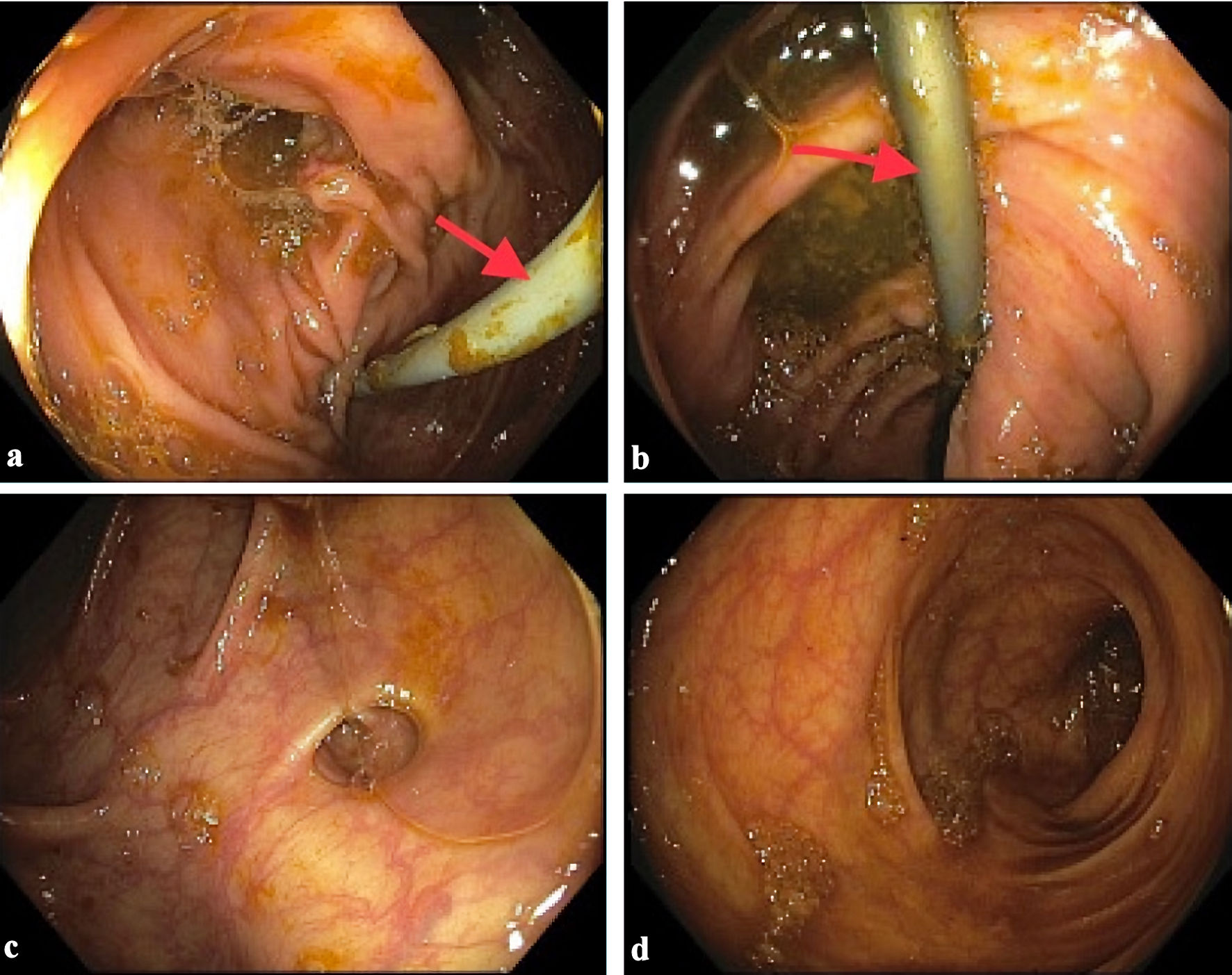 Click for large image | Figure 2. Endoscopic image showing a migrated stent impacted in the cecum and extending into the ascending colon. (a) Cecum. (b) Ascending colon. (c) Sigmoid colon. (d) Rectum. Red arrows (a) and (b) show a migrated stent impacted in the cecum. |
| Discussion | ▴Top |
Endoscopic biliary stenting is a less invasive procedure for treating benign and malignant biliary disorders [2, 6, 8]. Stenting restores biliary tract patency and helps ease pruritus, jaundice, and cholangitis associated with biliary tract obstructions [9]. Biliary stenting is associated with a 5% risk of early complications such as pancreatitis, infection, bleeding, perforation, and early stent migration [10]. Late complications are more common and include stent occlusions and late stent migration [10]. Stent migration has been observed in 5-10% of cases, and stents usually pass through the rectum without complications [2, 8, 10]. Gut perforation and abscesses, lower gastrointestinal bleeding, and fistulas are rare, occurring in less than 1% of cases, and are mostly found in the duodenum [2, 3, 6, 10-13]. Colonic diverticulosis, adhesions from previous surgeries, and abdominal hernias predispose patients to bowel perforations [2, 4, 8, 10], as they impede stent migration through the gut. Bilio-cecal stent migration with rectal bleeding is an infrequent event with few cases reported to date [5, 7]. Here, we report a unique case of bilio-cecal stent impaction presenting as rectal bleeding. This case adds to the limited literature on this subject and raises awareness about this potential complication. Although there was no colonic ulceration or stigmata of recent bleeding noted in the cecum, we postulated that the migrated stent lodged in the colonic diverticulum causing ulceration and bleeding.
Biliary stent migration can be spontaneous, and patients may not have symptoms. In some cases, patients can present with abdominal pain, nausea, vomiting, pruritus, jaundice, weight loss, or steatorrhea [3, 4, 7, 8, 10, 11]. Blake et al [6] presented a unique case of recto-vaginal fistula secondary to biliary stent migration, in which the patient complained of passing flatus and stools through the vagina. The management of migrated stents depends on the location and the patient’s clinical presentation [10]. Conservative treatment is often employed with the expectation of spontaneous passage through the rectum [6, 8]. Serial abdominal X-ray examinations can confirm stent passage or track its location through the digestive tract [6]. In this case, the patient was critically ill and actively bleeding from the rectum. A decision was made to forego imaging studies of the abdomen and proceed with upper endoscopy and colonoscopy.
Endoscopic stent retrieval using forceps, baskets, or the lasso technique is the most preferred approach [4, 8]. Some sources recommend endoscopy with clip placement even in cases of bowel perforation due to stent migration [4]. Alcaide et al [12] described a case of sigmoid perforation due to a migrated biliary stent, which was closed endoscopically with a through-the-scope clip. In this case, a colonoscopy was deemed to be appropriate for stent removal. Interventional radiology techniques such as percutaneous drainage and fluoroscopy may also be used to manage migrated stents. Culnan et al [3] reported an unusual case of ileal perforation and abscess caused by a displaced biliary stent that was managed with percutaneous drainage and fluoroscopy. Open surgery may be considered as an option for bowel obstruction or perforation refractory to endoscopic management [2, 10, 11]. Even so, open surgeries have a high risk of bleeding and infection and may be contraindicated in patients with coagulopathic disorders [8].
Learning points
Biliary stenting is an effective and widely adopted intervention for managing biliary disorders such as obstructions and choledocholithiasis. Stents can be occluded or displaced in the gut, leading to their spontaneous passage through the rectum. Rarely, displaced biliary stents can be trapped in the digestive tract, causing perforation or small bowel obstructions. Biliary stent impaction in the cecum causing massive hemorrhage is a very rare event that warrants immediate intervention
Acknowledgments
We are grateful to the patient for allowing us to share this interesting case report with the rest of the medical community.
Financial Disclosure
No funding was obtained for the writing or submission of this case report.
Conflict of Interest
A portion of this case report was presented as a poster at the American College of Gastroenterology Annual Conference, in October 2023, and published as an abstract in the American Journal of Gastroenterology.
Informed Consent
The patient consented to the publication of this case report.
Author Contributions
LB and SG conceptualized the idea of this case report. MJ, MP, JE, and RY helped write the case report. KA and YC supervised the patient’s care and edited and proofread the final version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
ED: emergency department; CEA: carcinoembryonic antigen; EUS: endoscopic ultrasound; ERCP: endoscopic retrograde cholangiopancreatography; PRBCs: packed red blood cells; ICU: intensive care unit; CBD: common bile duct
| References | ▴Top |
- Mangiavillano B, Pagano N, Baron TH, Arena M, Iabichino G, Consolo P, Opocher E, et al. Biliary and pancreatic stenting: Devices and insertion techniques in therapeutic endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography. World J Gastrointest Endosc. 2016;8(3):143-156.
doi pubmed pmc - Tzovaras G, Liakou P, Makryiannis E, Paroutoglou G. Acute appendicitis due to appendiceal obstruction from a migrated biliary stent. Am J Gastroenterol. 2007;102(1):195-196.
doi pubmed - Culnan DM, Cicuto BJ, Singh H, Cherry RA. Percutaneous retrieval of a biliary stent after migration and ileal perforation. World J Emerg Surg. 2009;4:6.
doi pubmed pmc - Cerisoli C, Diez J, Gimenez M, Oria M, Pardo R, Pujato M. Implantation of migrated biliary stents in the digestive tract. HPB (Oxford). 2003;5(3):180-182.
doi pubmed pmc - Namdar T, Raffel AM, Topp SA, Namdar L, Alldinger I, Schmitt M, Knoefel WT, et al. Complications and treatment of migrated biliary endoprostheses: a review of the literature. World J Gastroenterol. 2007;13(40):5397-5399.
doi pubmed pmc - Blake AM, Monga N, Dunn EM. Biliary stent causing colovaginal fistula: case report. JSLS. 2004;8(1):73-75.
pubmed pmc - Kumar K, Sinha R, Nafe ZM. Post ERCP gastrointestinal hemorrhage: An unusual complication of migrated biliary stent. J Family Med Prim Care. 2020;9(2):1212-1214.
doi pubmed pmc - Garg K, Zagzag J, Khaykis I, Liang H. Surgical relief of small bowel obstruction by migrated biliary stent: extraction without enterotomy. JSLS. 2011;15(2):232-235.
doi pubmed pmc - Levy MJ, Baron TH, Gostout CJ, Petersen BT, Farnell MB. Palliation of malignant extrahepatic biliary obstruction with plastic versus expandable metal stents: An evidence-based approach. Clin Gastroenterol Hepatol. 2004;2(4):273-285.
doi pubmed - Jones M, George B, Jameson J, Garcea G. Biliary stent migration causing perforation of the caecum and chronic abdominal pain. BMJ Case Rep. 2013;2013:bcr2013009124.
doi pubmed pmc - Rybinski F, Heinrich H, Zimmerli M, Kahl S. The pierced colon: when biliary stents go the wrong way. ACG Case Rep J. 2023;10(3):e01019.
doi pubmed pmc - Alcaide N, Lorenzo-Pelayo S, Herranz-Bachiller MT, de la Serna-Higuera C, Barrio J, Perez-Miranda M. Sigmoid perforation caused by a migrated biliary stent and closed with clips. Endoscopy. 2012;44(Suppl 2 UCTN):E274.
doi pubmed - Akbulut S, Cakabay B, Ozmen CA, Sezgin A, Sevinc MM. An unusual cause of ileal perforation: report of a case and literature review. World J Gastroenterol. 2009;15(21):2672-2674.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


