| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 11, November 2024, pages 319-323
Ingested Magnets Found Inadvertently During Elective Magnetic Resonance Imaging
Jennifer R. Sawyera, Lance M. Rellandb, c, Molly S. Hageleb, Joseph D. Tobiasb, c, d
aHeritage College of Osteopathic Medicine - Dublin Campus, Dublin, Ohio and Ohio University, Athens, OH, USA
bDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
cDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
dCorresponding Author: Joseph D. Tobias, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted July 2, 2024, accepted September 13, 2024, published online October 10, 2024
Short title: Magnets and MRI
doi: https://doi.org/10.14740/jmc4280
| Abstract | ▴Top |
In the presence of a strong magnetic field such as for magnetic resonance imaging (MRI), ferromagnetic objects may become a source of patient or healthcare provider injury. To prevent such problems, careful screening of patients and healthcare workers is mandatory prior to MRI to identify contraindications to MRI including the presence of external or internal ferromagnetic products. We present a 2-year, 11-month-old child who presented for MRI to evaluate a potential vertebral anomaly. During initial scanning and image acquisition, image distortion was noted which was subsequently determined to be the result of ingested magnetic objects. The basic principles of MRI are discussed, safety pathways to prevent patient and practitioner risk related to ferromagnetic objects presented, and previous reports of patient-related adverse effects from internal ferromagnetic devices reviewed.
Keywords: Magnetic resonance imaging; Radiologic imaging; Ferromagnetic; Adverse effects
| Introduction | ▴Top |
Magnetic resonance imaging (MRI) is based on the magnetization properties of atomic nuclei [1, 2]. During data acquisition and image formation, a strong external magnetic field aligns protons (hydrogen nuclei) that would otherwise be randomly oriented within the structures being examined. The alignment of these protons is then disrupted by external radio frequency (RF) pulses that bring them to a higher energy state. The relaxation phase during which the nuclei return to their lower energy alignment with the magnetic field generates signals. The generated signals are detected in an RF coil, processed (digitized/sampled), and subjected to Fourier transformation for image formation. The varying intensity levels in these images are represented by corresponding shades of gray in a matrix of pixels.
The use of nuclear magnetic resonance was first reported in the medical literature by Raymond Damadian in 1971 when it was used to distinguish between healthy and malignant tissue in rats [3]. By the 1980s, the use of MRI in non-invasive diagnostic radiology became prevalent due to its ability to produce high-quality images without exposing a patient to ionizing radiation [2]. Although free of ionizing radiation and generally considered safe for patients and healthcare providers, MRI may pose other safety risks and have specific contraindications [4-6]. When ferromagnetic objects are within or in the vicinity of the magnetic field of the device, injury may occur to the patient or healthcare providers. The force from the magnet on a ferromagnetic object can result in a projectile effect. Implanted wires (such as in pacemakers) can be displaced or heated by induced currents from the RF magnetic field resulting in burning. Finally, ferromagnetic objects impact image quality causing image degradation and artifacts.
To prevent such problems, careful screening of patients and healthcare workers is mandatory prior to MRI to identify contraindications to MRI including the presence of external or internal ferromagnetic products. We present a 2-year, 11-month-old child who presented for MRI to evaluate a potential vertebral anomaly. During initial scanning and image acquisition, image distortion was noted, which was subsequently determined to be the result of ingested magnetic objects. Safety pathways to prevent patient and practitioner risk related to ferromagnetic objects are presented, and previous reports of patient-related adverse effects from internal ferromagnetic devices are reviewed.
| Case Report | ▴Top |
Review of this case and presentation in this format followed the guidelines of the Institutional Review Board of Nationwide Children’s Hospital. A 2-year, 11-month-old girl presented for general anesthesia during scheduled MRI of the spine without contrast to investigate a congenital sacral dimple. The past history was significant for 22q11.2 deletion syndrome, developmental delay, feeding disorder, failure to thrive as an infant, moderate obstructive sleep apnea, hypotonia, vitiligo, short stature, and a congenital sacral dimple. Pre-imaging screening, history, and physical examination were unremarkable. The preoperative anesthesia physical examination revealed a small, retrognathic mandible. The remainder of the airway examination was normal. Pulmonary and cardiac exams were normal. The abdomen was soft and non-distended with no palpable masses. The patient was held nil per os for 6 h and transported to the MRI induction room. After the application of standard American Society of Anesthesiologists’ monitors, anesthesia was induced by the inhalation of incremental concentrations of sevoflurane in nitrous oxide and oxygen. After the induction of anesthesia, a peripheral intravenous cannula was placed, and a laryngeal mask airway placed. Anesthesia was maintained with sevoflurane in air and oxygen. Upon initiation of MRI, initial scout sequences demonstrated prominent susceptibility artifacts emanating from the abdomen (Fig. 1). Imaging was immediately terminated, and a radiograph of the abdomen demonstrated a string of round metallic objects within the left side of the abdomen (Fig. 2). The patient’s trachea was intubated and she was transported to the operating room while anesthetized. Repeat abdominal exam revealed that the abdomen was soft, non-distended, without palpable masses. The patient’s mother reported decreased appetite over the past few days, but denied emesis or other complaints. Endoscopy of the stomach and upper small bowel failed to reveal any metallic objects. Diagnostic laparoscopy located the metallic objects along with a small bowel to small bowel fistula in the mid-ileum. The laparoscopic incision was extended, and the foreign body removed, which was noted to be a string of nine magnetic beads (Fig. 3). A small portion of the ileum was resected and an end-to-end anastomosis performed. Postoperatively, the patient was held nil per os until return of bowel function. The remainder of her postoperative course was unremarkable. Her diet was advanced on postoperative day (POD) 1. She was discharged to home on POD 2. On further questioning, the mother identified the metallic beads as those played with by her and her sibling, and that she occasionally placed these objects in her mouth.
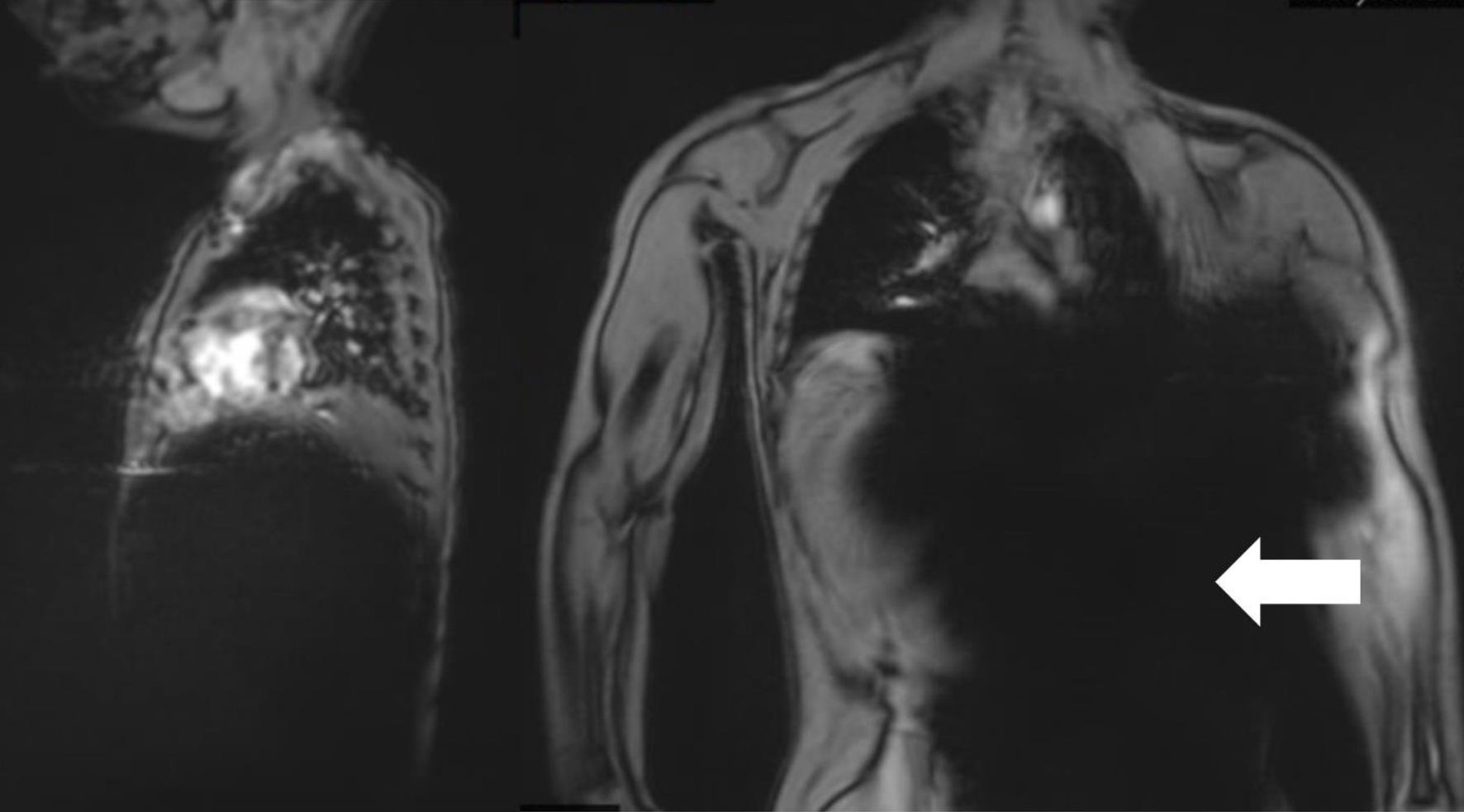 Click for large image | Figure 1. Initial magnetic resonance imaging scout sequences demonstrating prominent susceptibility artifacts (white arrow) emanating from the abdomen suggestive of a ferromagnetic foreign body. |
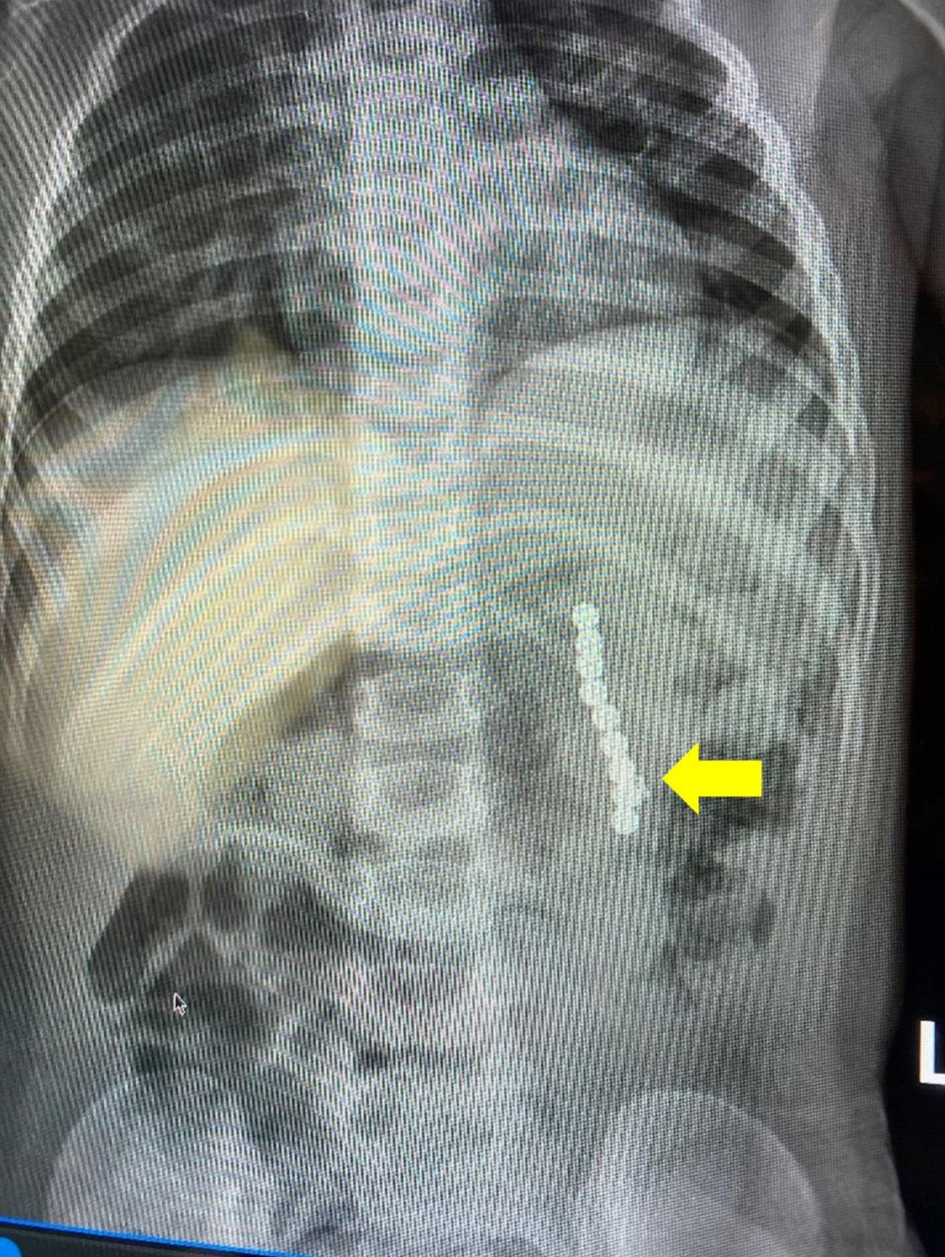 Click for large image | Figure 2. Due to the scout sequences demonstrating prominent imaging artifacts, MR scanning was immediately terminated and a radiograph of the abdomen was obtained which demonstrated a string of rounded metallic objects (yellow arrow) within the left side of the abdomen. MR: magnetic resonance. |
 Click for large image | Figure 3. Photograph of magnetic metallic beads similar to those swallowed by our patient. |
| Discussion | ▴Top |
MRI is frequently preferred over other imaging technologies in pediatric patients as it lacks ionizing radiation, provides high quality imaging, and is generally considered safe. When proper procedures are not followed, if accurate information is not received from the patient, or if deviations from safety protocols occur, morbidity or even mortality can occur. The magnet in a 1.5 Tesla (T) MRI machine produces a magnetic field that is estimated to be approximately 30,000 times stronger than that of the Earth [5]. While the strength of the majority of MRI machines in use by hospitals today are 1.5 - 3.0 T, the US Food and Drug Administration (FDA) has approved the clinical use of magnets up to 8 T in strength. Although increasing the magnetic field has the benefit of improving the efficiency and image quality, it may also increase risks to safety [6].
Because of the inherent dangers in the potential interaction of any ferromagnetic object within the magnetic field during MRI, specific safety procedures are in place to prevent adverse events. One of these safety procedures includes dividing the magnetic resonance site into four zones, each with a different level of restriction. The patient waiting area is a public space with no restrictions and defines zone I. Zone II is where patients are prepared for the procedure, give their medical history, and have routine preoperative physical examinations and preoperative anesthesia evaluations performed. Screening questionnaires and other safety evaluations are also performed in zone II. Zone II includes the reception area, dressing rooms, and MRI screening rooms. The transition from zone II to zone III is monitored by safety personnel. Zone III includes the scanner control room and the anesthesia induction room. Zone III has potential danger because of its proximity to the scanner. Zone IV has the highest risk and the greatest restrictions as it contains the magnetic resonance scanner and the magnet. When unattended, zone IV must be locked, and if a patient experiences an emergency while in zone IV, they are relocated elsewhere before life-saving measures can begin [5].
All patients and healthcare providers are routinely screened for implants or other ferromagnetic foreign bodies. A safety screening questionnaire is used in all patients to determine whether MRI is safe. Questions include current medications and allergies, MRI history, and medical and surgical history. It also includes a comprehensive list of both surgically implanted and removable medical devices the patient may have that the technologist would need to be aware of, as well as personal items on a patient that would need to be removed. In addition, some MRI suites include a standard metal detector that must be passed through to enter zone III. Personnel who operate magnetic resonance equipment must be extensively trained in how to keep themselves, untrained staff, and patients safe [5, 6]. Despite these safety precautions, as illustrated by our case, adverse events related to unidentified ferromagnetic objects may occur.
A 2019 review outlined 1,568 adverse events reported to the FDA related to the use of magnetic resonance systems over a 10-year period [7]. Of these events, 10 resulted in death of a patient, but only four were directly related or caused by improper use of the magnetic resonance system. Adverse events were categorized by cause. Thermal events were the most common at 59% followed by mechanical at 11%. Projectiles, caused by unidentified ferromagnetic objects, were next at 9% and accounted for 133 of the 1,568 events. Objects that were involved in the projectile events included walkers, wheelchairs, stretchers, and chairs, gas cylinders, magnet components exposed during service, tools, patient monitoring equipment, carts, intravenous (IV) poles, surgical tools, firearms, floor polishers, and firefighting equipment. The majority of the projectile events recorded were attributable to human error and in most cases, not due to the patient. The review did not cite any examples of adverse events due to the ingestion of a ferromagnetic object similar to our patient.
Reports of patients having a magnetic resonance scan with an unidentified ingested ferromagnetic foreign body, such as occurred in our patient, are rare. Our review of the literature identified only three previous reports including two children and one adult (Table 1) [8-10]. In the first of these cases, a 5-year-old male with neck pain underwent MRI and later developed severe abdominal pain due to bowel perforations resulting from 11 magnets that had been swallowed [8]. In the second case, a 3-year-old child developed diffuse swelling and redness of the forehead and the right orbital region following a 10-day history of an upper respiratory infection [9]. Extinction of facial imaging due to a ferromagnetic object in the nasal region was noted. Upon further inspection, a small button battery was found in his nasal cavity. In the final of these three cases, a 65-year-old male with schizophrenia and intellectual disability developed severe abdominal pain, hypovolemia, and septic shock after MRI that were subsequently identified as being the result of ingesting metal sockets and a clevis pin [10].
 Click to view | Table 1. Reported Cases of Ferromagnetic Objects Identified Incidentally During MRI |
Learning points
The incidental identification of unidentified ingested ferromagnetic objects during MRI is rare. However, such events are an important consideration, especially in patients who are unreliable historians. Foreign body ingestion in children under the age of 6 is estimated to account for over 75,000 emergency department (ED) visits per year. The most frequent objects include coins, toys, jewelry, and batteries [11]. Each of these have the potential to cause significant morbidity and mortality during MRI. It is possible for these objects to move or become heated due to the impact of the magnetic field. During such movement, bowel perforation or local tissue damage may occur. As MRI in children is often performed under general anesthesia, this may mask clinical signs and symptoms. With current screening technology and procedures, the safety of MRI has been increased. However, additional screening modalities may be required especially if the patient is an unreliable historian. Bailey et al reported that at their institution they have implemented a hand-held ferromagnetic scanner, and testing has shown it is able to identify small magnets within patients [8]. Susini et al reported their anecdotal experience with use of a handheld magnet to identify superficial metallic objects in four patients [12]. However, the device has not been evaluated for identifying a metallic object within the gastrointestinal tract through tissue and with the potential for a gas interface between the object and the magnet. These additional screening tools may have a role in preventing the clinical scenario noted in our patient.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained for anesthetic care and the use of de-identified information for publication.
Author Contributions
JRS: preparation of initial, subsequent, and final drafts; JDT: concept, writing, and review of all drafts; LMR and MSH: perioperative care of patient, and review of final draft.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Pooley RA. AAPM/RSNA physics tutorial for residents: fundamental physics of MR imaging. Radiographics. 2005;25(4):1087-1099.
doi pubmed - Smith HJ. The history of magnetic resonance imaging and its reflections in Acta Radiologica. Acta Radiol. 2021;62(11):1481-1498.
doi pubmed - Damadian R. Tumor detection by nuclear magnetic resonance. Science. 1971;171(3976):1151-1153.
doi pubmed - Dill T. Contraindications to magnetic resonance imaging: non-invasive imaging. Heart. 2008;94(7):943-948.
doi pubmed - Shah A, Aran S. A review of magnetic resonance (MR) safety: the essentials to patient safety. Cureus. 2023;15(10):e47345.
doi pubmed pmc - Mittendorff L, Young A, Sim J. A narrative review of current and emerging MRI safety issues: What every MRI technologist (radiographer) needs to know. J Med Radiat Sci. 2022;69(2):250-260.
doi pubmed pmc - Delfino JG, Krainak DM, Flesher SA, Miller DL. MRI-related FDA adverse event reports: A 10-yr review. Med Phys. 2019;46(12):5562-5571.
doi pubmed - Bailey JR, Eisner EA, Edmonds EW. Unwitnessed magnet ingestion in a 5 year-old boy leading to bowel perforation after magnetic resonance imaging: case report of a rare but potentially detrimental complication. Patient Saf Surg. 2012;6(1):16.
doi pubmed pmc - Metterlein T, Haubner F, Knoppke B, Graf B, Zausig Y. An unexpected ferromagnetic foreign body detected during emergency magnetic resonance imaging: a case report. BMC Res Notes. 2014;7:808.
doi pubmed pmc - Glover NM, Roten R. Gastric perforation during MRI after ingestion of ferromagnetic foreign bodies. Clin Pract Cases Emerg Med. 2021;5(3):362-364.
doi pubmed pmc - Orsagh-Yentis D, McAdams RJ, Roberts KJ, McKenzie LB. Foreign-body ingestions of young children treated in US emergency departments: 1995-2015. Pediatrics. 2019;143(5):e20181988.
doi pubmed - Susini P, Pozzi M, Di Secli D, Nisi G, Cuomo R, Brimaldi L. Off-label application of the breast expander magnet: An alternative approach to enable localisation and removal of ferromagnetic subcutaneous foreign bodies. Surg Practice. 2024;28:32-37.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


