| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 11, November 2024, pages 324-329
Tonsillar Diffuse Large B-Cell Lymphoma of Non-Germinal Center Type With Cluster of Differentiation 5 Positive in a Pediatric Girl
Ibrahim Alharbia, Fay Khalid Salawatib, Shaimaa Alnajjarb, c , Ascia Khalid Alabbasib
aDepartment of Pediatrics, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
bCollage of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
cCorresponding Author: Shaimaa Alnajjar, Collage of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
Manuscript submitted July 3, 2024, accepted September 4, 2024, published online October 10, 2024
Short title: Tonsillar Lymphoma Positive for CD5
doi: https://doi.org/10.14740/jmc4288
| Abstract | ▴Top |
Lymphoma is a common malignancy in children. It is the second most common malignancy in children older than 1 year of age. Most extranodal non-Hodgkin lymphoma (NHL) in the head and neck is usually caused by diffuse large B-cell lymphoma (DLBCL), but pediatric DLBCL with cluster of differentiation (CD)5 expression is rarely discussed in the literature. An 8-year-old Saudi female presented with painful swallowing for a year. She underwent tonsillectomy. Histopathology and immunohistochemistry studies show stage II NHL as DLBCL in the left tonsil, non-germinal center B-cell (non-GCB) with aberrant CD5 expression. She completed all cycles of chemotherapy. She experienced febrile neutropenia after the first cycle but did not have any other complications. Current chemotherapy has an excellent prognosis, but the treatment approach depends on the disease stage risk classification. We emphasized that malignancy is not excluded by the absence of constitutional symptoms.
Keywords: Pediatric; Tonsilitis; Non-Hodgkin lymphoma; Non-GCB
| Introduction | ▴Top |
Diffuse large B-cell lymphoma (DLBCL) causes most extranodal non-Hodgkin lymphoma (NHL) in the head and neck. DLBCL is the most prevalent type of NHL affecting children with congenital or acquired immunodeficiency. It accounts for 20% of pediatric lymphomas. Although it can arise among individuals of any age, most of those who are at greater risk for it are middle-aged and older. Additionally, this condition affects males more than females [1, 2].
The clinical presentation of DLBCL varies, including the presence of constitutional symptoms, diffuse lymphadenopathy, hepatosplenomegaly, and, in some cases, extranodal disease. They may have signs and symptoms in the oral region, manifesting as numerous swellings that develop rapidly. Usually, these lesions are painless. They usually cover intact or ulcerated mucosa [3].
The best way to diagnose DLBCL is to perform an excisional biopsy on suspicious-looking tissue that seems abnormally enlarged after a clinical evaluation and radiographic imaging. This method prevents sampling mistakes and false negatives, which can occur with fine needle aspiration or core biopsy in a highly diverse tissue and enables a large amount of tissue to be evaluated by pathology. The histological features of DLBCL include the widespread proliferation of giant lymphocytes resembling centroblasts or immunoblasts. These giant cells usually have nuclei that are twice as large as normal lymphocytes or equivalent to or larger than normal macrophages [4].
The mainstay therapy for DLBCL is chemotherapy with curative intention at the initial diagnosis [5]. Also, non-germinal center B-cell (non-GCB) type patients have a poorer prognosis compared with GCB type [1].
This report presents a pediatric case of non-Hodgkin’s DLBCL non-GCB type in the left tonsil who initially presented with painful swallowing.
| Case Report | ▴Top |
An 8-year-old Saudi female presented at the otolaryngology clinic with 1-year history of painful swallowing, recurrent tonsillitis, snoring, and mouth breathing. She had no history of fever, weight loss, night sweating, upper respiratory tract infection symptoms, obstructive sleep apnea, hearing loss or any other head and neck symptoms.
Examination revealed left sided grade 4 tonsillitis, adenoid hypertrophy and bilateral sub centimetric enlarged cervical lymph nodes.
Investigations
Neck and chest computed tomography (CT) scans showed small nonspecific axillary and cervical lymphadenopathy, with no evidence of mediastinal or hilar lymphadenopathy, pulmonary masses or consolidation (Fig. 1a-c).
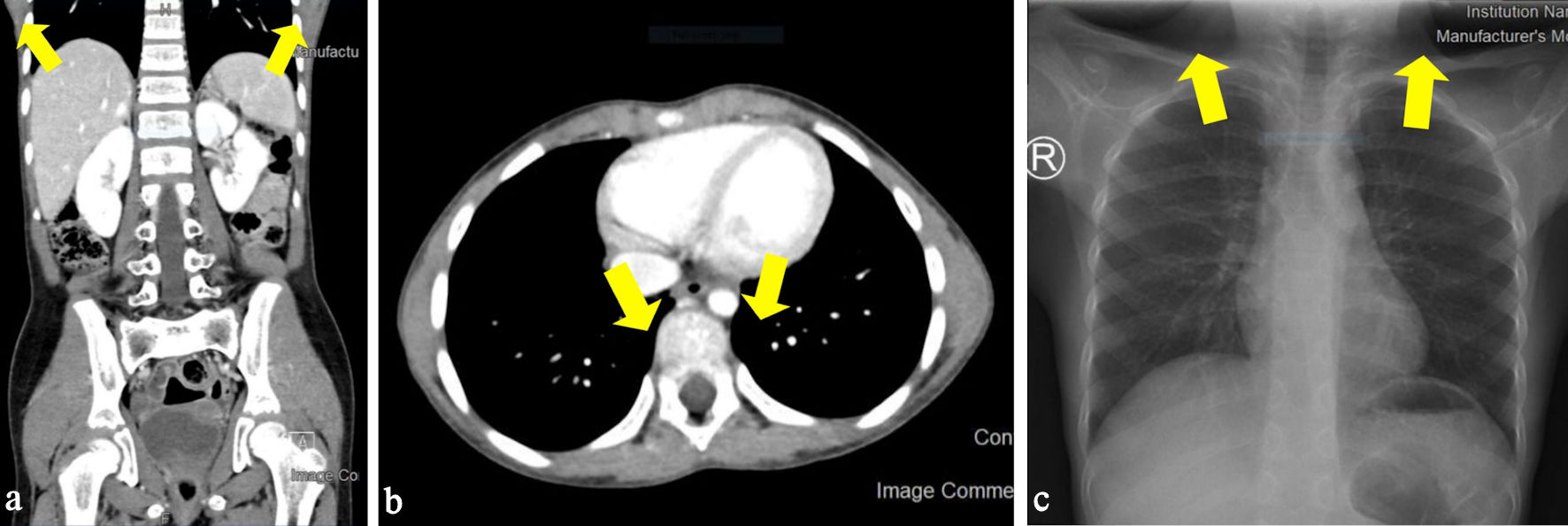 Click for large image | Figure 1. (a) Small axillary lymph nodes (arrow). (b) No mediastinal or hilar lymph nodes (arrow). (c) Small cervical lymph nodes (arrow). |
The patient underwent tonsillectomy, and the specimen was sent to the histopathology lab. The macroscopic examination was found to be composed of three pieces of firm lobulated mass measured 3 × 2 × 2 cm. On cut section, a homogenous, white, lobulated, and solid mass was found.
Tonsil mass specimen morphology and immunohistochemistry
As per our center’s policy, all tonsils resected should be examined histologically. Pathological examination showed expansion of the stroma by dense lymphoid infiltrates (hematoxylin and eosin stain × 100) (Fig. 2a).
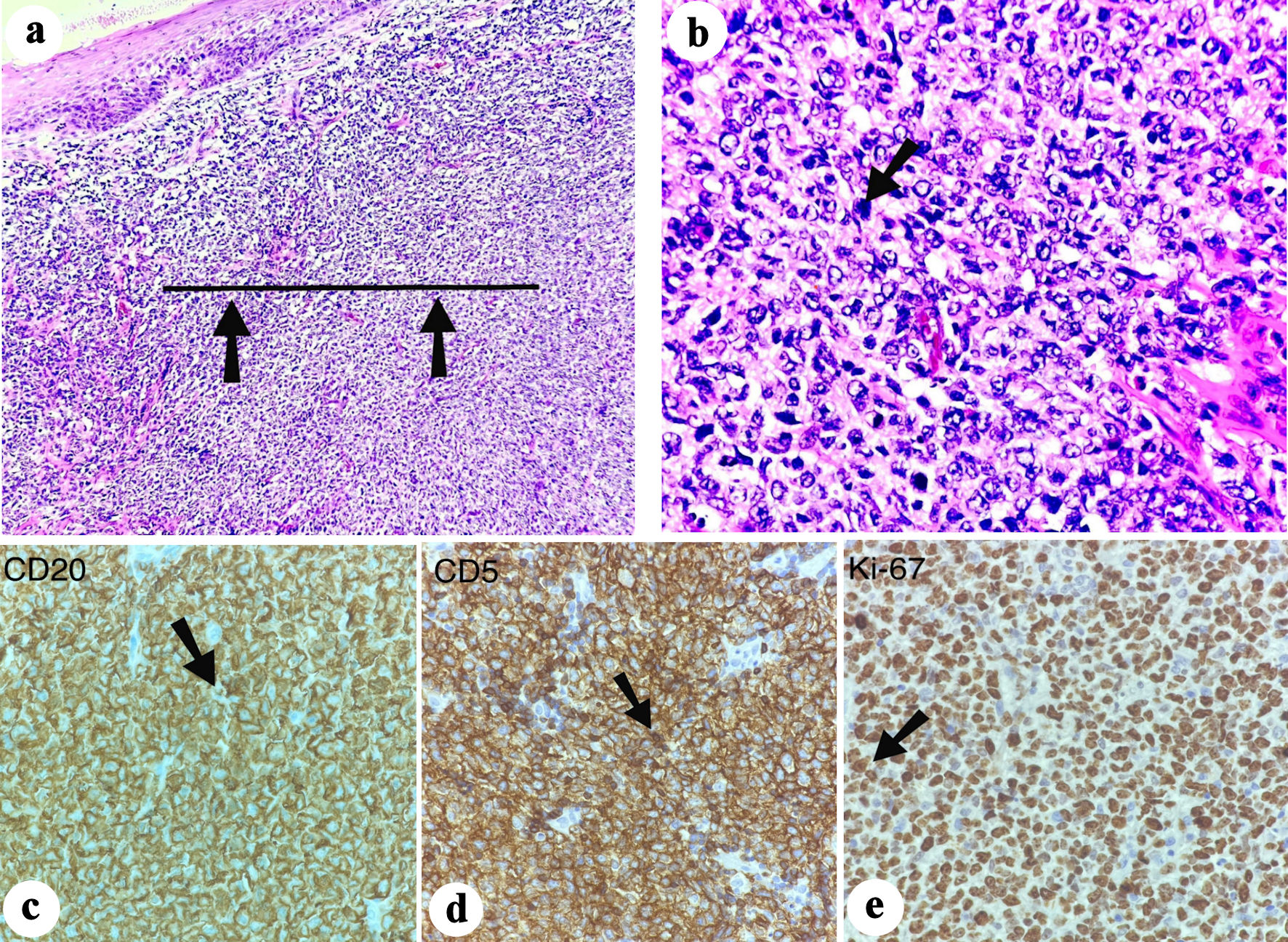 Click for large image | Figure 2. (a) Hematoxylin and eosin staining, × 100. The straight horizontal line and black arrows point at the infiltrates that are composed of large cells with high nucleo-cytoplasmic ratio, vesicular nuclei, and inconspicuous nucleoli. (b) A malignant lymphocyte with positive CD20 and positive CD5 (Ki-67 proliferation index of about 80%) (black arrow). (c) Malignant B cells that are positive for CD20 (black arrow). (d) Malignant B cells that are positive for CD5 (black arrow). (e) Malignant B cells that are positive for Ki-67 (black arrow). Ki-67: antigen Kiel 67; CD: cluster of differentiation. |
Immunohistochemistry was performed on formalin-fixed paraffin-embedded sections using ultraView Universal DAB Detection kit with the following antibody clones: leukocyte common antigen (LCA) (RP2/18), cluster of differentiation (CD)3 (26V6), CD30 (BERH), CD15 (MMA), CD20 (L26), CD5 (SP19), CD10 (SP67), B-cell lymphoma 2 (BCL2) (SP66), BCL6 (GL191E/A8), pan-cytokeratin (PAN-CK) (36), Epstein-Barr virus (EBV) (CS1-4), paired box 5 (PAX5) (SP34), CD23 (SP23), and cyclin D1 (SP4-R).
Immunohistochemistry study shows that about 80% of tumor cells are positive for antigen Kiel 67 (Ki-67) and the following clones: LCA, CD20, PAX5, CD5, multiple myeloma oncogene (MUM), BCL6 and BCL2 (weak patchy) (Fig. 2b-e), and negative for CD2, CD3, CD4, CD8, CD10, CD15, CD30, cyclin D1, EBV, CD23 and CK-PAN.
Fluorescence in situ hybridization (FISH) result showed no BCL6, IGH-BCL2, or myelocytomatosis oncogene (MYC) rearrangement in 100% of 200 nuclei analyzed.
Diagnosis
After a tumor board meeting, the diagnosis was confirmed to be stage II NHL consistent with DLBCL, non- GCB subtype with aberrant CD5 expression.
Treatment
Chemotherapy regimen including cyclophosphamide, oncovin (vincristine), prednisolone, doxorubicin, and methotrexate (COPADM I) was planned for the patient.
Follow-up and outcomes
The patient arrived at the emergency room a few days after the first round of chemotherapy, complaining of a congested throat and fever documented at 39.7 °C. Upon arrival, laboratory investigations showed decreased levels of absolute neutrophil count (ANC) of 0.001, and the patient was treated as a case of febrile neutropenia. After 3 days, ANC improved (ANC = 15.1), and she was discharged.
| Discussion | ▴Top |
DLBCL is an aggressive form of cancer, it is considered one of the most common NHLs seen among pediatric patients. It constitutes about 10-20% of all NHLs in children, with predominance of GCB subtype, which comprises around 70% of pediatric cases. However, DLBCL in children has a better prognosis than adults, with a high event-free survival (EFS) rate of nearly 90% [3, 6]. In this report, we are presenting a unique case of an 8-year-old Saudi female with non-GCB subtype DLBCL.
The clinical manifestations include the presence of constitutional symptoms, diffuse lymphadenopathy, hepatosplenomegaly and, in some cases extranodal disease [3]. Conversely, pediatric patients with DLBCL rarely present with full picture of constitutional symptoms and/or multiple extranodal disease. The clinical presentation of pediatric lymphoma in general is variable.
Tonsillar lymphomas are uncommon in pediatric patients. It is typically seen in elderly males which often presents as swelling of tonsils, sore throat, difficulty swallowing, and cervical lymphadenopathy. However, DLBCL is the most common histological type found in tonsillar lymphoma [6]. The prevalence of tonsillar lymphoma in children is about 0.021/100,000 (1 in 5,000,000) patients per year. Most of the cases of tonsillar lymphoma in children are unilateral (80%). The incidence of tonsillar lymphoma demonstrates a notable male predominance by 2.1:1, and it is higher among children of White ethnicity compared to individuals of other ethnic backgrounds. Higher rates of head and neck lymphoma were recorded in North America, Australia/New Zealand, and Europe compared to Asia and Africa [7, 8]. Unlike the usual presentation, our patient is a female, she presented with recurrent tonsillitis, snoring, and mouth breathing with no constitutional symptoms.
Risk factors for both adults and children include the presence of personal or family history of NHLs or DLBCL, genetic predisposition, primary immunodeficiencies, organ transplantation, autoimmune diseases, and infections such as human immunodeficiency virus (HIV), Epstein-Barr virus (EBV), Kaposi sarcoma herpesvirus/human herpesvirus 8 (KSHV/HHV8), hepatitis C virus (HCV), and there is an emerging evidence suggesting an association between hepatitis B virus (HBV) and DLBCL [9]. None of the aforementioned factors are present in our patient.
DLBCL exhibits considerable heterogeneity as a disease. Its diagnosis necessitates the examination of a tumor biopsy through histopathological and molecular analysis to accurately identify and characterize the condition. The cells in DLBCL typically express specific B-cell antigens, including CD19, CD20, CD22, CD79a, and CD30 in some cases [4]. Immunohistochemistry study of our patient showed CD20 and aberrant CD5 expression.
However, to evaluate the clinical status of a patient prior to treatment, it is recommended to perform a comprehensive set of assessments by conducting a full history and physical examination. In addition to laboratory tests that include complete blood count with differential, blood film morphology analysis, coagulation profile evaluation, electrolyte measurement, lactate dehydrogenase (LDH) determination (if > 2 upper limit of normal (ULN)), analysis of lymphocyte subsets, assessment of immunoglobulin (Ig) levels (IgG, IgM, IgA), testing for specific antibody responses to tetanus, Haemophilus influenzae type b (Hib), 13-valent pneumococcal conjugate vaccine (PCV-13) (Prevenar), meningococcal B/C vaccines (Men B/C), screening for human immunodeficiency virus (HIV) infection, and hepatitis B screening (prior to rituximab administration). It is also important to conduct bilateral bone marrow aspirate and trephine biopsy, along with a lumbar puncture to analyze cerebrospinal fluid. Moreover, the initial radiological investigations should include chest X-ray and abdominal ultrasound, followed by cross-sectional imaging of the neck, chest, abdomen, and pelvis to stage the condition. Lastly, cranial, or spinal magnetic resonance imaging (MRI) can be performed in case of neuropathy [10].
Overall, the treatment decisions for DLBCL should be determined by patient’s risk group based on the stage of the disease, and the presence or absence of resected disease [4, 10]. In our case, the patient has been diagnosed with stage II NHL, specifically DLBCL. By taking the previous point into consideration, the treatment plan for our patient involves chemotherapy with COPADM I. As of March 24, 2024, she has already completed all cycles of chemotherapy, including initially receiving both COP (cyclophosphamide, oncovin, prednisolone) and COPADM I.
Current chemotherapy has shown an excellent prognosis in patients with DLBCL. Yet, the outcome in case of relapsed/refractory (r/r) disease is poor, since the cure rates are less than 30%, and there is no standard treatment. However, rituximab-containing salvage regimens have shown a complete or partial response in 60-70% of the cases. Nonetheless, the long-term survival rate remains below 10% for patients who have not undergone transplantation [5, 11].
As said before, tonsillar lymphoma is an extremely rare entity. We reviewed the literature and found several adult and pediatric cases. We will summarize the main findings here. Several studies between 2002 and 2022 have reported cases of individuals experiencing various symptoms related to tonsillar abnormalities. Aroor et al reported a case for a 13-year-old male complaining of headache localized in the left side, with diplopia and left parapharyngeal mass [12]. Another case reported by Azamar et al involved a 10-year-old male who had pharyngodynia, dysphagia, hypersalivation, orthopnea and asymmetrical tonsils [13]. While Toader et al presented a case of a 5-year- old male suffering from nasal obstruction along with snoring, hyponasal speech, mouth breathing during sleeping, obstructive sleep apnea, abnormal sleep position, adenoidal hypertrophy and left tonsillar enlargement [14]. Unlike the previous presentations, Amit et al reported a case of a 6-year-old male who only complained of left tonsil enlargement and stridor [15]. Siupsinskiene et al documented a case of a 4-year-old male with a history of sore throat accompanied by otalgia, snoring, difficulty breathing and mass in the right tonsils [16]. As well, two cases reported by Al-Essa involved a 7-year-old female with a left palatine tonsil mass associated with snoring and voice change, and the other 10-year-old male, who had right palatine tonsillar mass, recurrent sore throat and change of voice [17].
Similarly, in the case presented in our report, the patient is of typical age (8 years old). She had a history of recurrent tonsillitis accompanied by snoring, mouth breathing, and unilateral tonsillar enlargement. The diagnosis was made based on the tonsillectomy specimen’s histopathology.
As most of the tonsillar lymphomas occur in adult patients, we will go over certain facts. The incidence of DLBCL increases with age [9]. Unlike the pediatric age group, the most prevalent lymphoid neoplasm in adults is DLBCL, which accounts for approximately 30-40% of all diagnosed lymphoid cases [18].
Here we review several case reports of tonsillar lymphoma in adults. Rajabato et al presented a case of a 59-year-old male who exhibited symptoms such as sore throat, dysphagia, odynophagia, unusual snoring, and swelling of the right tonsil [6]. While Rai et al reported a case of 65-year-old male with swelling in the left tonsillar fossa along with dysphagia and dysphonia [2]. Furthermore, Jiang et al documented a case of a 40-year-old male who complained of swelling in the right palatine tonsil, dysphagia, suffocation, and snoring [19]. Torres et al reported a case of a 50-year-old male who presented with odynophagia, along with tonsillar enlargement and painful cervical swelling on the left side [20].
There are many factors affecting the outcome of adult tonsillar lymphoma. These include the stage of the disease and the size of the mass. In addition, the presence of B symptoms and World Health Organization (WHO) Performance Score affect treatment outcome. However, the patients who presents with early-stage disease have a 5-year survival rate of 65-85% [2]. None of the cases in the literature were positive for CD5 (Table 1) [2, 6, 12-17, 19, 20].
 Click to view | Table 1. Review of the Tonsillar Lymphoma Literature |
CD5 is expressed in 1) chronic lymphocytic leukemia (CML); 2) mantle cell lymphoma; 3) splenic marginal zone lymphoma; 4) DLBCL. In DLBCL, approximately 5-10% of cases show CD5 positivity, and some may manifest as splenic lesions. CD5+ DLBCL has a poor prognosis and a relatively high incidence of central nervous system (CNS) relapse even in the rituximab era. Eighty-three percent of patients who experienced CNS relapse had brain parenchymal disease. Immunohistochemically, 82% of CD5+ DLBCLs are classified as the non-GCB type.
CD5+ DLBCL had been recognized as an aggressive immunophenotypic subgroup of DLBCL in the 2008 WHO classification of hematolymphoid neoplasm; however, it was eliminated from the list of subgroups of DLBCLs in the revised 2016 classification [21]. Nevertheless, there is much controversy regarding the clinical significance of CD5 expression, and many researchers still assert that this subgroup exhibits an extremely unfavorable prognosis with frequent treatment failure. A study retrospectively investigated 405 DLBCLs recruited from three university hospitals in Korea from 1997 to 2013 [22]. The clinical profile, immunophenotype, and chromosomal structural alterations of the BCL2 and MYC genes were compared according to CD5 expression. A total of 29 cases of de novo CD5+ DLBCL were identified out of 405 in their series (7.4%). Clinicopathologic correlation was performed in all 29 CD5+ DLBCLs and 166 CD5- DLBCLs, which were eligible for full clinical review and further pathologic examination. Compared with CD5- counterparts, CD5+ DLBCLs showed female preponderance, frequent bone marrow involvement, higher LDH level, advanced Ann Arbor stages and poorer prognosis (all P < 0.05). Pathologically, the expression of CD5 positively correlated with that of BCL2, MYC and Ki-67 (all P < 0.05). Coexpression of BCL2 and MYC, which is referred to as a double-expressor, was relatively more common in CD5+ DLBCL, whereas translocation or amplification of these genes was very rare. In conclusion, the expression of CD5 is an independent poor prognostic factor of DLBCLs, and this subgroup displays unique clinicopathologic features [23]. Although the exact mechanism remains uncertain, consistent activation of BCL2 and MYC by alternative pathways other than chromosomal translocation may contribute to the pathogenesis [24, 25].
Conclusions
In summary, tonsillar DLBCL is rare among pediatric patients. The predominant clinical characteristics seen in pediatric patients include unilateral tonsillar enlargement and cervical lymphadenopathy. The treatment decision should be made based on the risk stratification.
Learning points
The learning point we aim to address in this case report is that the absence of constitutional symptoms does not exclude malignancy. Recurrent tonsillitis, unilateral tonsillar enlargement, and lymphadenopathy are also concerning.
Acknowledgments
None to declare.
Financial Disclosure
No funds were received for this research.
Conflict of Interest
The authors declare that there are no conflicts of interest that could potentially influence the results or interpretation of the study. This includes financial, personal, or professional relationships that could be perceived as having biased the work. The research was conducted with the utmost integrity and transparency, and the authors have no affiliations or financial involvement with any organization or entity that could pose a conflict of interest.
Informed Consent
Written informed consent was obtained.
Author Contributions
Ibrahim Alharbi MD, principal author: supervision and critical review. Fay Khalid Salawati: manuscript writing and literature review. Shaimaa Alnajjar: manuscript writing. Ascia Khalid Alabbasi: manuscript writing.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
ANC: absolute neutrophil count; Ki-67: antigen Kiel 67; BCL: B-cell lymphoma; CNS: central nervous system; CML: chronic lymphocytic leukemia; CT: computed tomography; CD: cluster of differentiation; COP: cyclophosphamide, oncovin, prednisolone; COPADM I: cyclophosphamide, oncovin, prednisone, Adriamycin, methotrexate; DLBCL: diffuse large B-cell lymphoma; EBV: Epstein-Barr virus; EFS: event-free survival; GCB: germinal center B-cell; Hib: Haemophilus influenzae type b; KSHV/HHV8: Kaposi sarcoma herpesvirus/human herpesvirus 8; HCV: hepatitis C virus; HIV: human immunodeficiency virus; Ig: immunoglobulin; LDH: lactate dehydrogenase; LCA: leukocyte common antigen; MRI: magnetic resonance imaging; MUM: multiple myeloma oncogene; MYC: myelocytomatosis oncogene; non-GCB: non-germinal center B-cell; NHL: non-Hodgkin lymphoma; OSA: obstructive sleep apnea; PAX-5: paired box protein; CK-PAN: pan cytokeratin; PCV13: 13-valent pneumococcal conjugate vaccine; ULN: upper limit of normal
| References | ▴Top |
- Yan S, Ma J, Yang M, Liu B, Li S, Yang L, Zhang Q, et al. Analysis of the clinicopathologic characteristics and prognosis of head and neck lymphoma. Anal Cell Pathol (Amst). 2022;2022:4936099.
doi pubmed pmc - Rai SJ, Kamath RR. Non-Hodgkin’s lymphoma: an unusual presentation. Otorhinolaryngology Clinics: An International Journal. 2021;13(2):8-10.
- Sheikh IN, Elgehiny A, Ragoonanan D, Mahadeo KM, Nieto Y, Khazal S. Management of aggressive non-Hodgkin lymphomas in the pediatric, adolescent, and young adult population: an adult vs. pediatric perspective. Cancers (Basel). 2022;14(12):2912.
doi pubmed pmc - Harker-Murray PD, Pommert L, Barth MJ. Novel therapies potentially available for pediatric B-cell non-Hodgkin lymphoma. J Natl Compr Canc Netw. 2020;18(8):1125-1134.
doi pubmed - Melchardt T, Egle A, Greil R. How I treat diffuse large B-cell lymphoma. ESMO Open. 2023;8(1):100750.
doi pubmed pmc - Rajabato W, Chandika V, Harahap AS. Unilateral tonsillar swelling as a manifestation of diffuse large B cell lymphoma (DLBCL): case report. Maedica (Bucur). 2021;16(4):750-752.
doi pubmed pmc - Adil EA, Medina G, Cunningham MJ. Pediatric tonsil cancer: a national and institutional perspective. J Pediatr. 2018;197:255-261.e251.
doi pubmed - Shamloo N, Ghannadan A, Jafari M, Ahmadi S, Mortazavi H, Baharvand M. Head and neck lymphoma in an iranian population. Iran J Otorhinolaryngol. 2017;29(94):261-267.
pubmed pmc - Wang SS. Epidemiology and etiology of diffuse large B-cell lymphoma. Semin Hematol. 2023;60(5):255-266.
doi pubmed pmc - Bhuller K, Bomken S, Burke A, et al. Guideline for management of mature B-cell non-Hodgkin lymphoma. Children's Cancer and Leukemia Group. 2020. https://www.cclg.org.uk/write/MediaUploads/Member%20area/Treatment%20guidelines/CCLG_B-NHL_guidelines_2020_Final.pdf.
- Moleti ML, Testi AM, Foa R. Treatment of relapsed/refractory paediatric aggressive B-cell non-Hodgkin lymphoma. Br J Haematol. 2020;189(5):826-843.
doi pubmed - Aroor R, Ravikumar A, Shetty VV, Bhat VS, Saldanha M, Sinha D. Unusual presentation of diffuse large B-cell lymphoma of nasopharynx. J Datta Meghe Inst Med Sci Univ. 2022;17(2):424-428.
- Azamar A, Torre-Gonzalez C, Juarez-Villegas L, Sadowinski-Pine S, Alvarez-Neri H. Asymmetric palatine tonsil in a pediatric patient: Is it always a malignant neoplasm? Bol Med Hosp Infant Mex. 2021;78(5):461-466.
doi pubmed - Toader C, Toader M, Stoica A, Pop G, Oprea A, Constantin AS, Niculescu L, et al. Tonsillar lymphoma masquerading as obstructive sleep apnea - pediatric case report. Rom J Morphol Embryol. 2016;57(2 Suppl):885-891.
pubmed - Amit S, Purwar N, Agarwal A, Lalchandani D. Tonsillar follicular lymphoma in a child. BMJ Case Rep. 2012;2012:10-13.
doi pubmed pmc - Siupsinskiene N, Padervinskis E, Poskiene L, Endeley N, Vaitkus S. An unusual case of a sore throat and otalgia in a 4-year-old boy. Medicina (Kaunas). 2012;48(5):277-279.
pubmed - Al-Essa, Abdul-Rahman Ali. Non endemic Burkitt's lymphoma of the tonsil. Saudi Journal of Otorhinolaryngology Head and Neck Surgery. 2002;4(2):52-54.
- Shi Y, Han Y, Yang J, Liu P, He X, Zhang C, Zhou S, et al. Clinical features and outcomes of diffuse large B-cell lymphoma based on nodal or extranodal primary sites of origin: Analysis of 1,085 WHO classified cases in a single institution in China. Chin J Cancer Res. 2019;31(1):152-161.
doi pubmed pmc - Jiang R, Zhang HM, Wang LY, Pian LP, Cui XW. Ultrasound features of primary non-Hodgkin's lymphoma of the palatine tonsil: A case report. World J Clin Cases. 2021;9(28):8470-8475.
doi pubmed pmc - Barbosa Torres L, Torres D, Cardoso A. Non-Hodgkin lymphoma presenting as tonsillitis. J Med Imaging Case Reports. 2020;4(1):19-21.
doi - Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J (eds). WHO classification of tumours of haematopoietic and lymphoid tissues. International Agency for Research on Cancer. 2017. (Medicine Series). https://books.google.com.sa/books?id=Qdt9swEACAAJ.
- Na HY, Choe JY, Shin SA, Kim HJ, Han JH, Kim HK, Oh SH, et al. Characteristics of CD5-positive diffuse large B-cell lymphoma among Koreans: High incidence of BCL2 and MYC double-expressors. PLoS One. 2019;14(10):e0224247.
doi pubmed pmc - Cabecadas J, Nava VE, Ascensao JL, Gomes da Silva M. How to diagnose and treat CD5-positive lymphomas involving the spleen. Curr Oncol. 2021;28(6):4611-4633.
doi pubmed pmc - Jaffe ES. Diagnosis and classification of lymphoma: impact of technical advances. Semin Hematol. 2019;56(1):30-36.
doi pubmed pmc - Fallah J, Olszewski AJ. Diagnostic and therapeutic splenectomy for splenic lymphomas: analysis of the National Cancer Data Base. Hematology. 2019;24(1):378-386.
pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


