| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 9, September 2024, pages 242-249
Intraoperative Takotsubo Syndrome
Gentian Hutia, b, Filadelfo Coniglionea, b, c, Alert Drishtia, Mustafa Bajraktaria, b, Alert Xhajaa, Asead Abdylib, Krenar Lilaja, Diamant Lulajb, Rudin Domia, b, d
aDepartment of Surgery, Service of Anesthesiology and Intensive Care, University of Medicine, Tirana, Albania
bDepartment of Anesthesiology and Intensive Care, American Hospital, Tirana, Albania
cDepartment of Clinical Science and Traslational Medicine, University of Rome Tor Vergata, Rome, Italy
dCorresponding Author: Rudin Domi, Department of Surgery, Service of Anesthesiology and Intensive Care, University of Medicine, Tirana, Albania
Manuscript submitted July 10, 2024, accepted August 19, 2024, published online August 22, 2024
Short title: Intraoperative Takotsubo Syndrome
doi: https://doi.org/10.14740/jmc4293
| Abstract | ▴Top |
Takotsubo cardiomyopathy is a rare condition that presents a diagnostic challenge due to its close resemblance to acute myocardial ischemia and other cardiac disorders. The excessive production of catecholamines triggers abnormal and severe changes in the myocardium, typically resulting in significant dyskinesia of the left ventricle’s apex, reduced ejection fraction, hypotension, and pulmonary edema. Recent reports suggest that potential risk factors may include postmenopausal syndrome and intense, unexpected stress, whether related to life events or medical conditions. Complications such as heart failure, thrombosis, and severe arrhythmias are infrequent and more likely to occur in patients with pre-existing cardiac conditions. We present the case of a 22-year-old woman who developed intraoperative Takotsubo cardiomyopathy during a transsphenoidal resection of a prolactin-secreting pituitary tumor under general anesthesia. Perioperative combination of cabergoline and oxymetazoline induced intraoperative hypertension, pulmonary edema, and Takotsubo stress cardiomyopathy. To our knowledge, this is the first reported case in the literature of intraoperative Takotsubo cardiomyopathy, potentially linked to the specific combination of intraoperative cabergoline and oxymetazoline.
Keywords: Takotsubo syndrome; Hypertension; Cabergoline; Oxymetazoline
| Introduction | ▴Top |
Takotsubo cardiomyopathy is characterized by severe dyskinesia of the left ventricular apex, leading to reduced stroke volume, decreased cardiac output, hypotension, pulmonary edema, and states of hypoperfusion [1]. The initiating pathophysiological process is unexpected and primarily driven by a large and abnormal release of catecholamines into the circulation. Other reported mechanisms include coronary spasms, microthrombosis, and catecholamine toxicity, which help explain complications of Takotsubo syndrome, such as heart failure, myocarditis, and malignant arrhythmias [2]. During stress, the hypothalamic-adrenal response is activated, leading to the release of norepinephrine from the locus coeruleus and increased levels of epinephrine and cortisol. Elevated norepinephrine levels further stimulate the hypothalamic-pituitary-adrenal axis, so increasing catecholamine levels [3].
The overall incidence of Takotsubo syndrome is estimated to be approximately 100 cases per 1 million people [4]. Takotsubo cardiomyopathy is reported to be approximately 2% among all patients treated in the emergency department for acute coronary syndrome, with a predominance in female patients [5, 6]. Female gender is affected more and the reported incidence is approximately 7.5% [6]. Other authors had recently reported that women over 50 years old account for 80-90% of patients suffering from Takotsubo syndrome [7].
Takotsubo diagnostic criteria are left ventricular regional wall motion abnormalities, absence of ischemic coronary artery disease, new reversible electrocardiography (ECG) changes, elevated pro-brain natriuretic peptide (BNP), mildly elevated troponin, and recovery of cardiac function [8, 9].
International Experts Consensus precizied the diagnostic process step by step based on the likelihood and severity of Takotsubo syndrome. Diagnostic criteria include clinical features (chest pain), changes in ECG, coronary angiography, coronary computed tomography (CT) angiography, and echocardiography [10].
We report a case of a rare and unexpected confirmed intraoperative Takotsubo cardiomyopathy. The patient developed pulmonary edema and hypotension following intraoperative administration of nasal oxymetazoline spray. Various diagnostic approaches were undertaken to explain and understand the situation, and intensive care unit treatment was primarily focused on managing hemodynamic and respiratory issues.
| Case Report | ▴Top |
Investigations
A 22-year-old woman was diagnosed with a prolactin-secreting pituitary macroadenoma based on clinical markers and magnetic resonance imaging (MRI) findings (Fig. 1). After confirming elevated prolactin levels (87 ng/mL, normal range: 2 - 24 ng/mL), pharmacological treatment with cabergoline (Dostinex) at a dose of 0.5 mg every 2 days was initiated. However, cabergoline treatment was unsuccessful after 1 year, necessitating neurosurgical intervention as the only viable treatment option. The patient had an unremarkable medical and anesthetic history, no cardiac risk factors, and no cardiac abnormalities detected during preoperative screening (Figs. 2 and 3). Preoperative echocardiography revealed normal cardiac size and function, as well as a normal valvular apparatus. Her preoperative blood pressure was 115/60 mm Hg, and her heart rate was 71 beats per minute, with a sinus rhythm and no QRS/QTc/JTc prolongations.
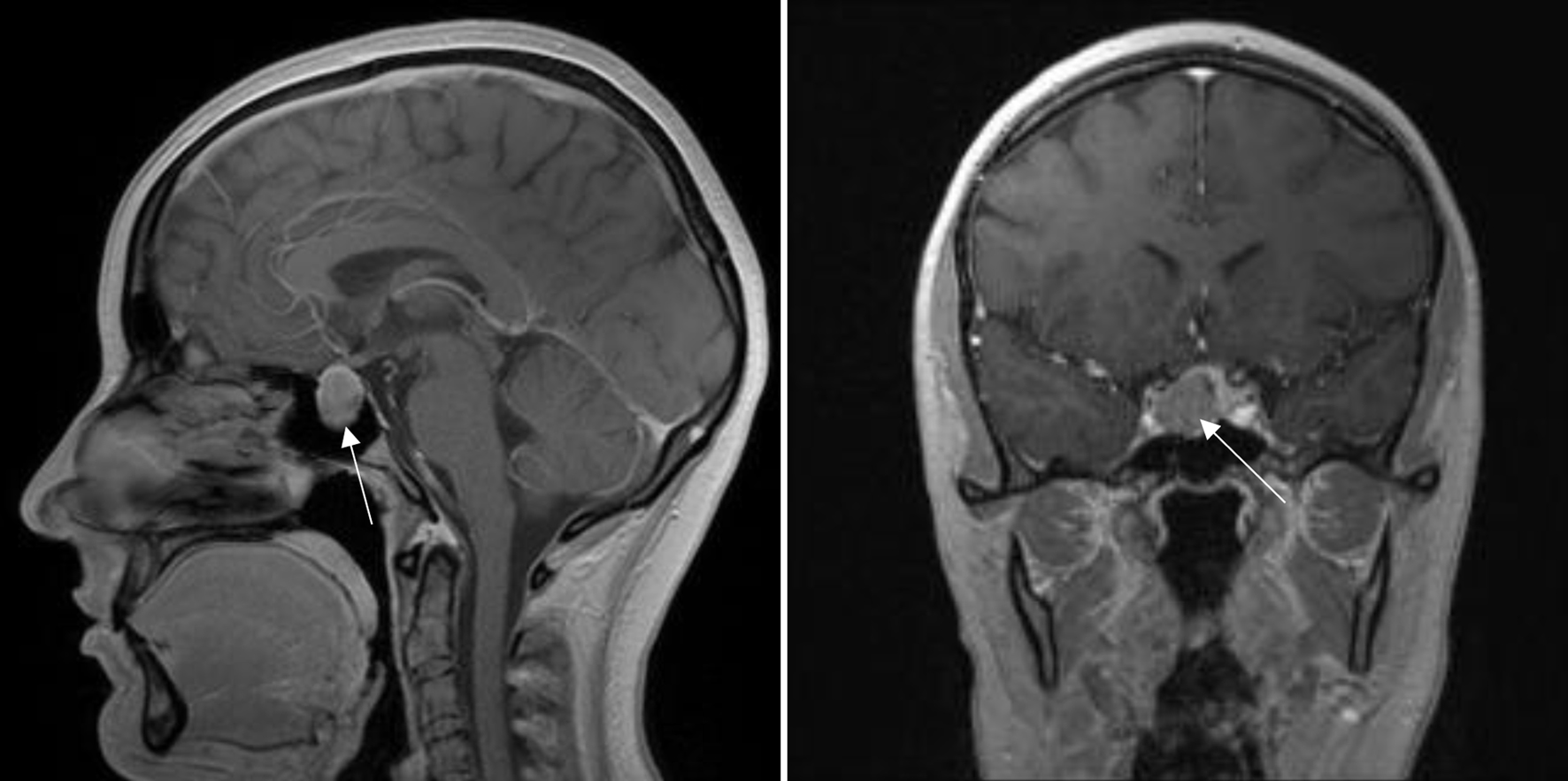 Click for large image | Figure 1. Magnetic resonance imaging examination showing hypophysial prolactinoma, suprasellar formation till optic chiasma (arrow). |
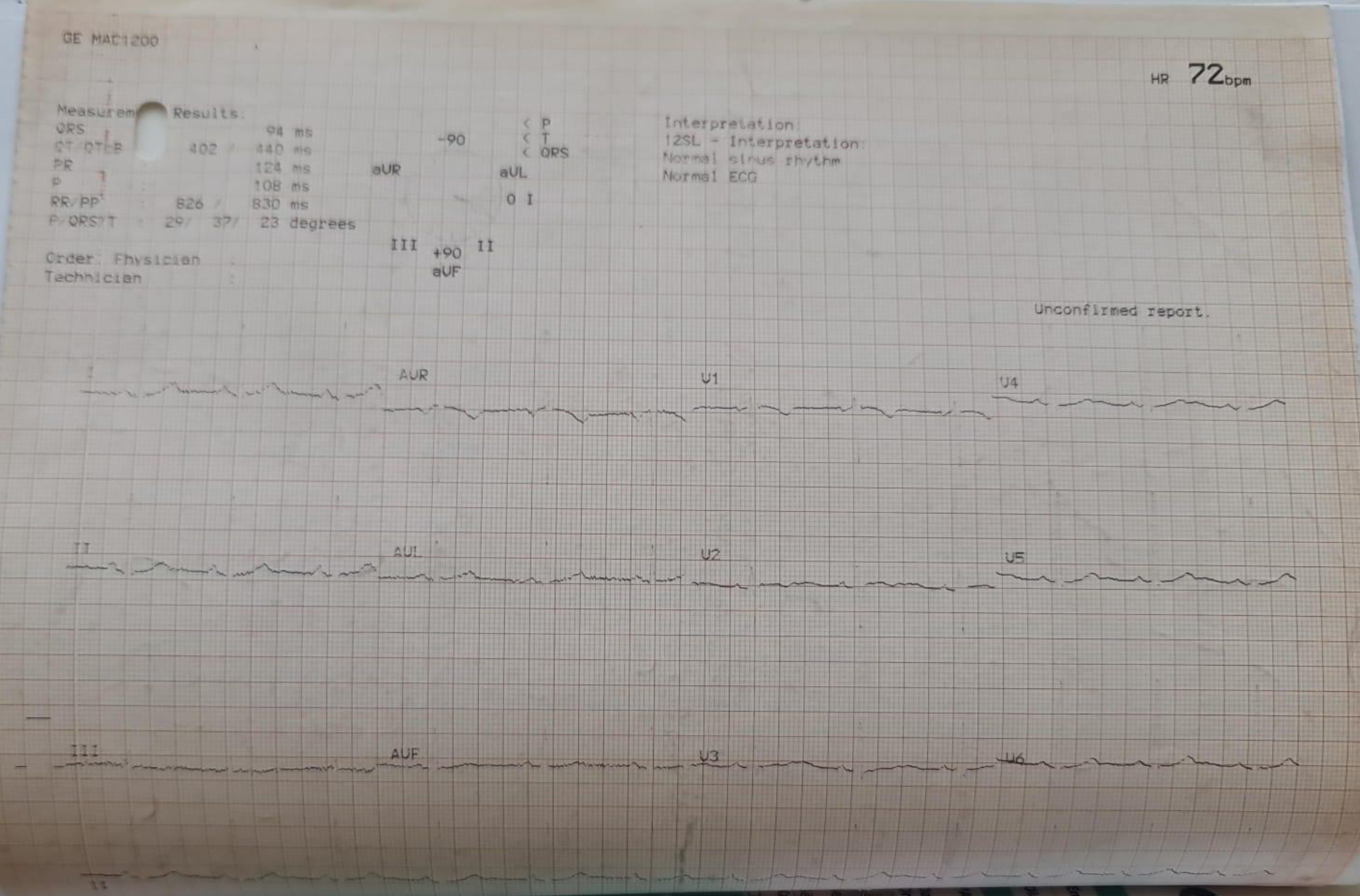 Click for large image | Figure 2. Preoperative normal electrocardiogram. |
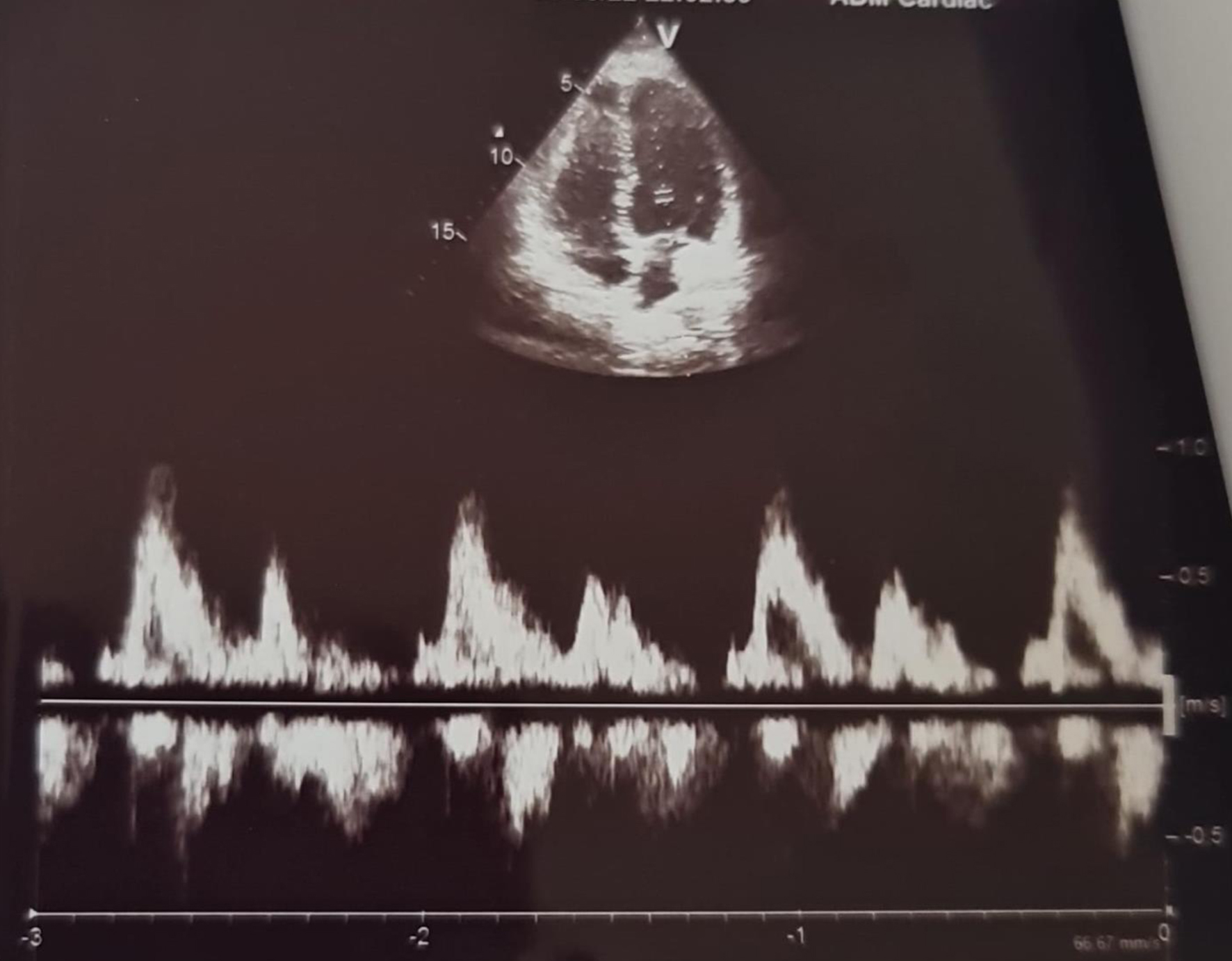 Click for large image | Figure 3. Preoperative normal echocardiography examination. |
Diagnosis
Anesthesia induction and endotracheal intubation were performed without complications. Anesthesia was maintained using total intravenous anesthesia (TIVA) with propofol (100 µg/kg/min) and remifentanil (0.3 µg/kg/min), ensuring adequate anesthesia and stable hemodynamic parameters. During transsphenoidal resection of the pituitary tumor, the anesthesiologist was requested to maintain mild hypotension to facilitate the surgical procedure. For this purpose, invasive blood pressure monitoring was instituted. Additionally, to ensure a clear surgical field and minimize bleeding, a decongestant spray is typically used by the surgical team. The neurosurgeon administered several intranasal puffs of oxymetazoline 0.1%. Approximately 10 min afterward, the patient developed sudden and persistent hypertension, with blood pressure rising to 190 - 203 mm Hg/100 - 110 mm Hg lasting at least 20 min, followed by desaturation to 85%, with a PaO2 of 51 mm Hg. The patient subsequently experienced classic pulmonary edema, leading to the surgery being halted and postponed.
Treatment
Aggressive intraoperative treatment for pulmonary edema was initiated in the operating room (OR), including the administration of diuretics, increasing the inspiratory fraction of oxygen (FiO2) to 100%, applying positive end-expiratory pressure (PEEP) of 10 cm H2O, elevating the head of the bed, and infusing nitroglycerin to normalize blood pressure. An intraoperative bronchoscopy was performed to remove a large amount of pink, frothy secretions. The patient was then transferred to the intensive care unit (ICU) after improving vital signs to tolerate safe transportation.
Follow-up and outcomes
A pulmonary CT scan revealed characteristic opacities consistent with pulmonary edema (Fig. 4). Transthoracic echocardiography done in ICU (60 min from symptoms onset) confirmed a reduction in cardiac function, with an ejection fraction (EF) of 35%, basal and septal hypokinesia, typical signs of left ventricular ballooning, and mild to moderate mitral valve regurgitation (Figs. 5 and 6). Takotsubo cardiomyopathy was diagnosed. ECG revealed sinus tachycardia with heart rate 115-111, ST-T depression 0.5 mm in V3-V5 and D2, D3, aVF derivations (Fig. 7). Troponin level was 0.6 µg/L (normal range less than 0.019 µg/L) and pro-BNP was 51.29 pmol/L (normal range 0 - 14.75 pmol/L). Coronary angiography resulted without coronary obstruction and abnormalities (Fig. 8). Treatment in ICU consisted of continued treatment of pulmonary edema and low-dose norepinephrine 0.05 µg/kg/min. Due to reduced cardiac function, mild hypotension, tachycardia, absence of left ventricular outflow obstruction, and the risk of catecholamine-induced arrhythmia, we opted for norepinephrine as a supportive measure. At low doses, it also enhanced inotropism. Hemodialysis was performed removing 2.5 L from the patient. After 9 h, the patient was successfully extubated under normal respiratory and hemodynamic parameters. Ten hours later, the EF was 45% and the next day, EF was returned to 60% normal value. The patient was transferred to the ward in a stable condition and referred to the cardiologist and endocrinologist.
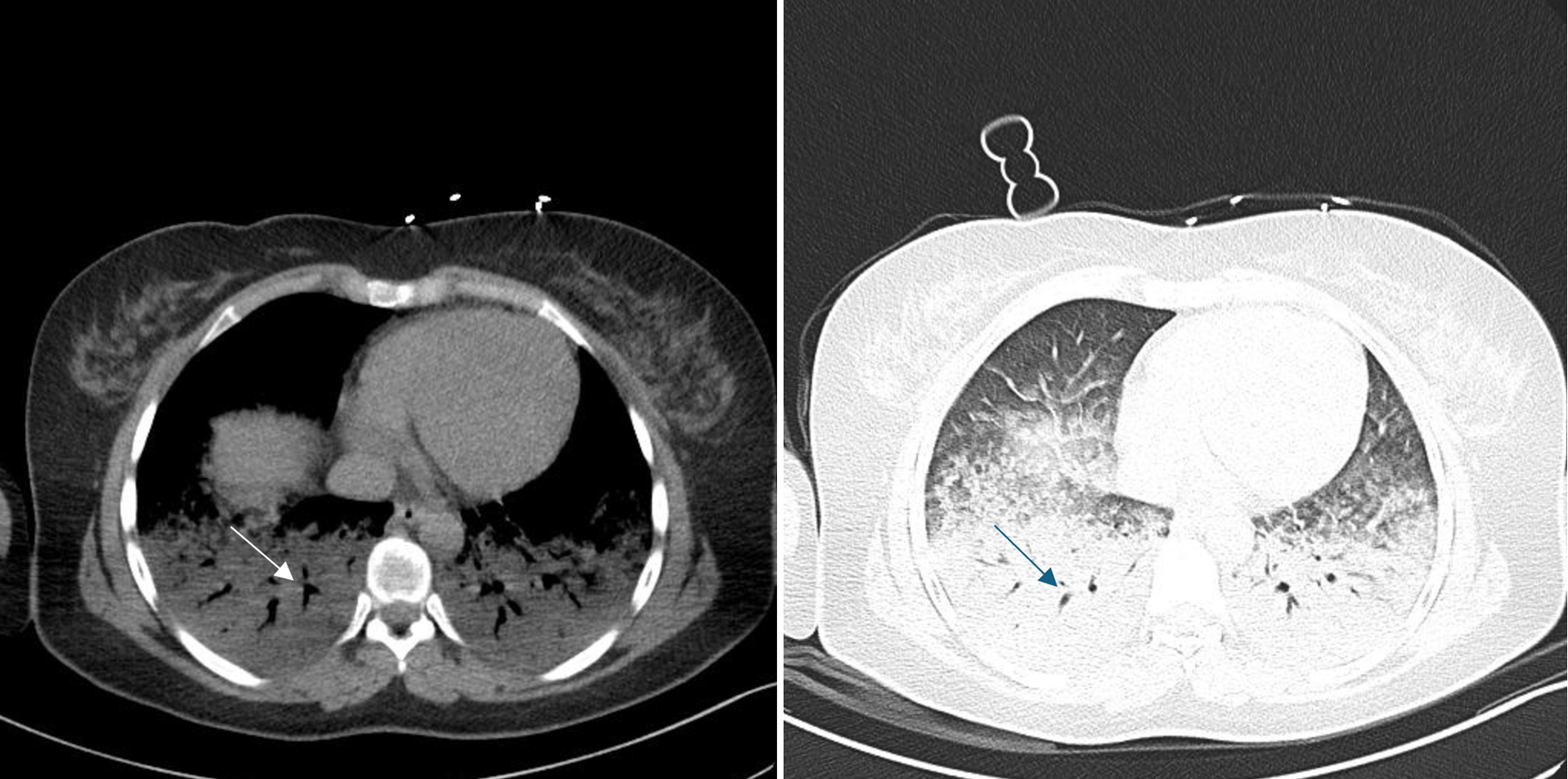 Click for large image | Figure 4. Chest computed tomography examination. Arrow indicates basal bilateral pulmonary infiltration. |
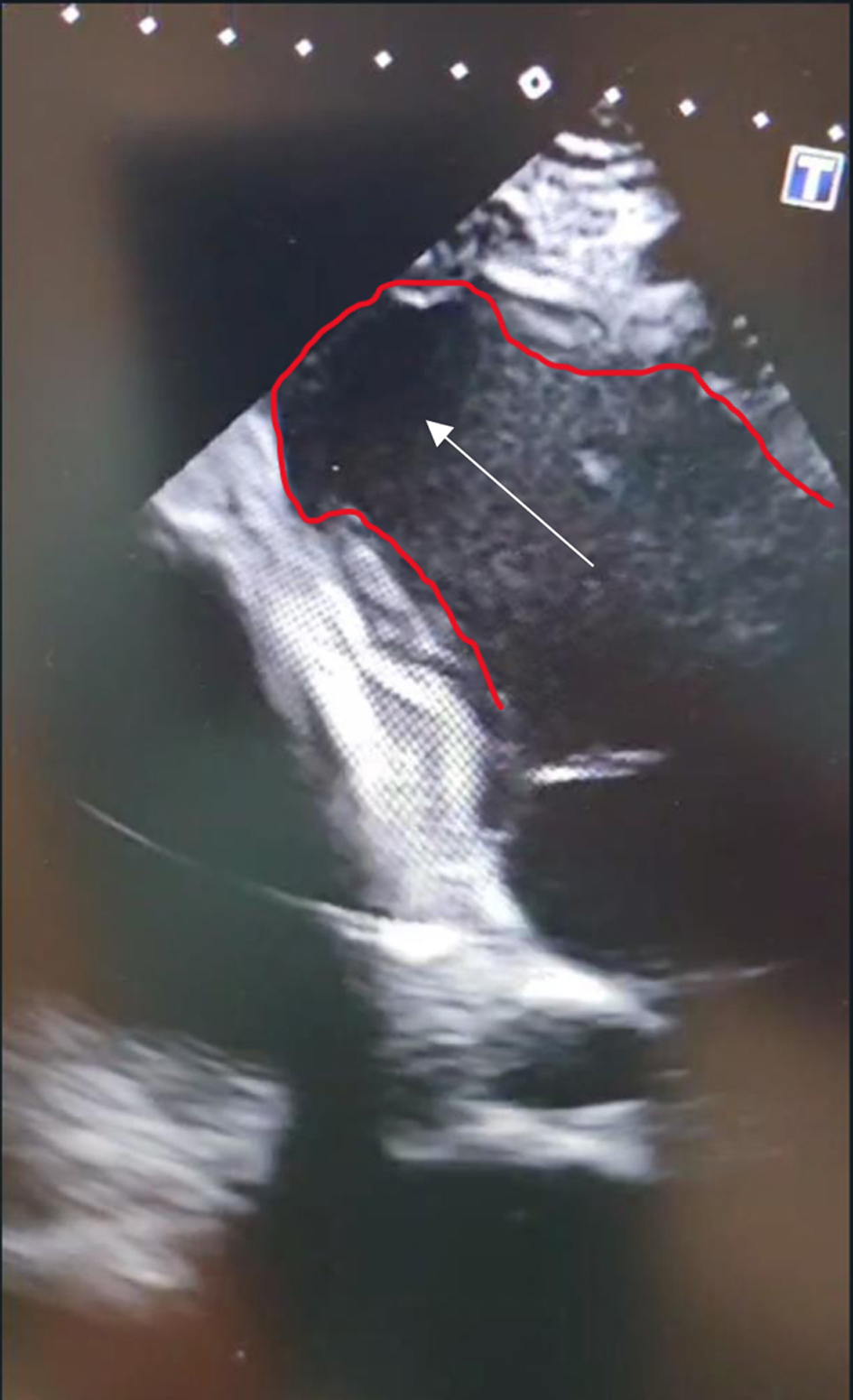 Click for large image | Figure 5. Characteristic takotsubo heart changes verified during transthoracic echocardiography. Arrow indicates apex balloon shape of left ventricle. |
 Click for large image | Figure 6. Takotsubo diagnosis confirmed by echocardiography. Arrow indicates characteristic “takotsubo” heart shape. |
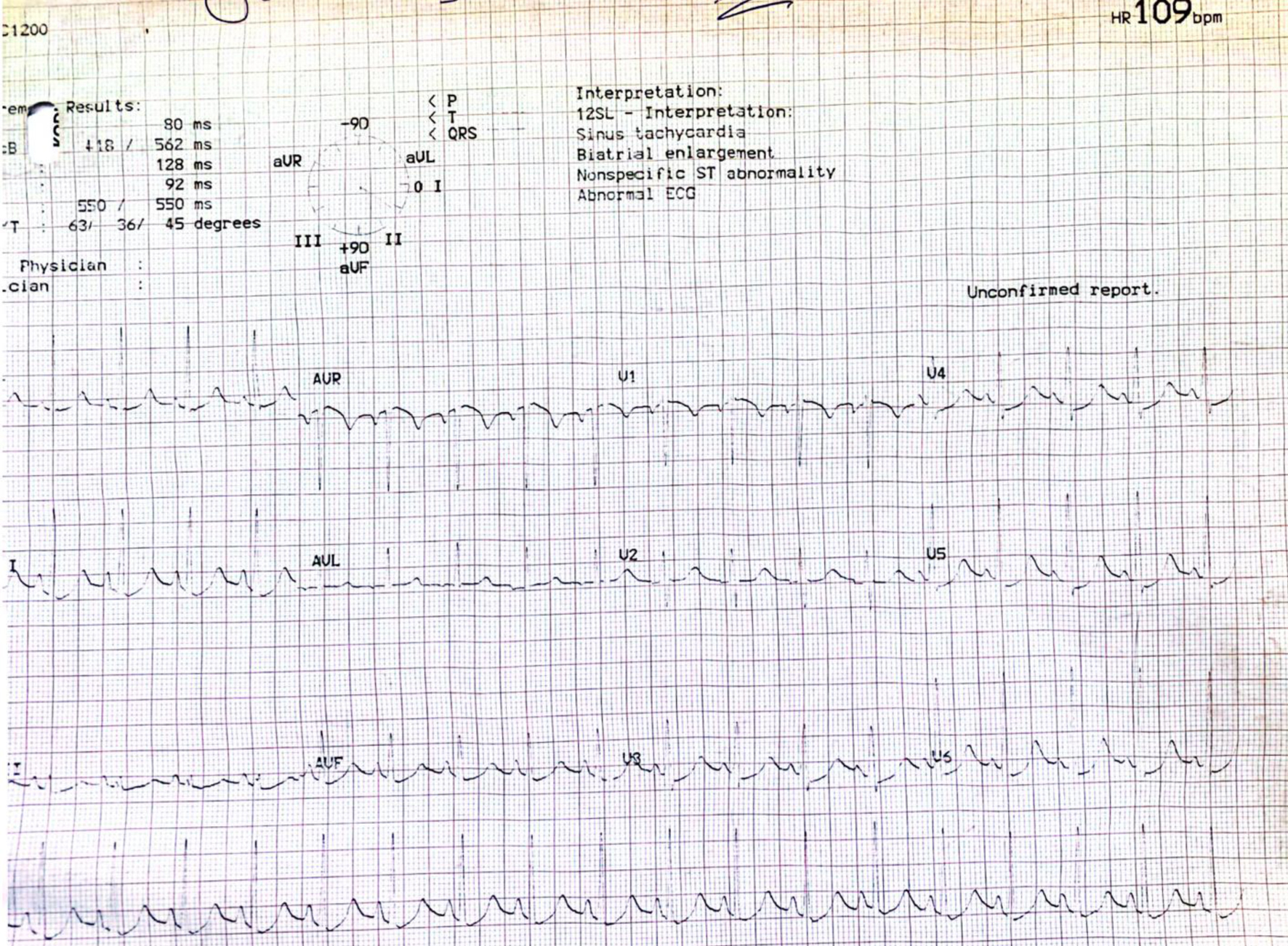 Click for large image | Figure 7. Echocardiography examination upon arrival in intensive care unit showing sinus tachycardia, ST denivelation in V3-V5, D2, D3, aVF derivations. |
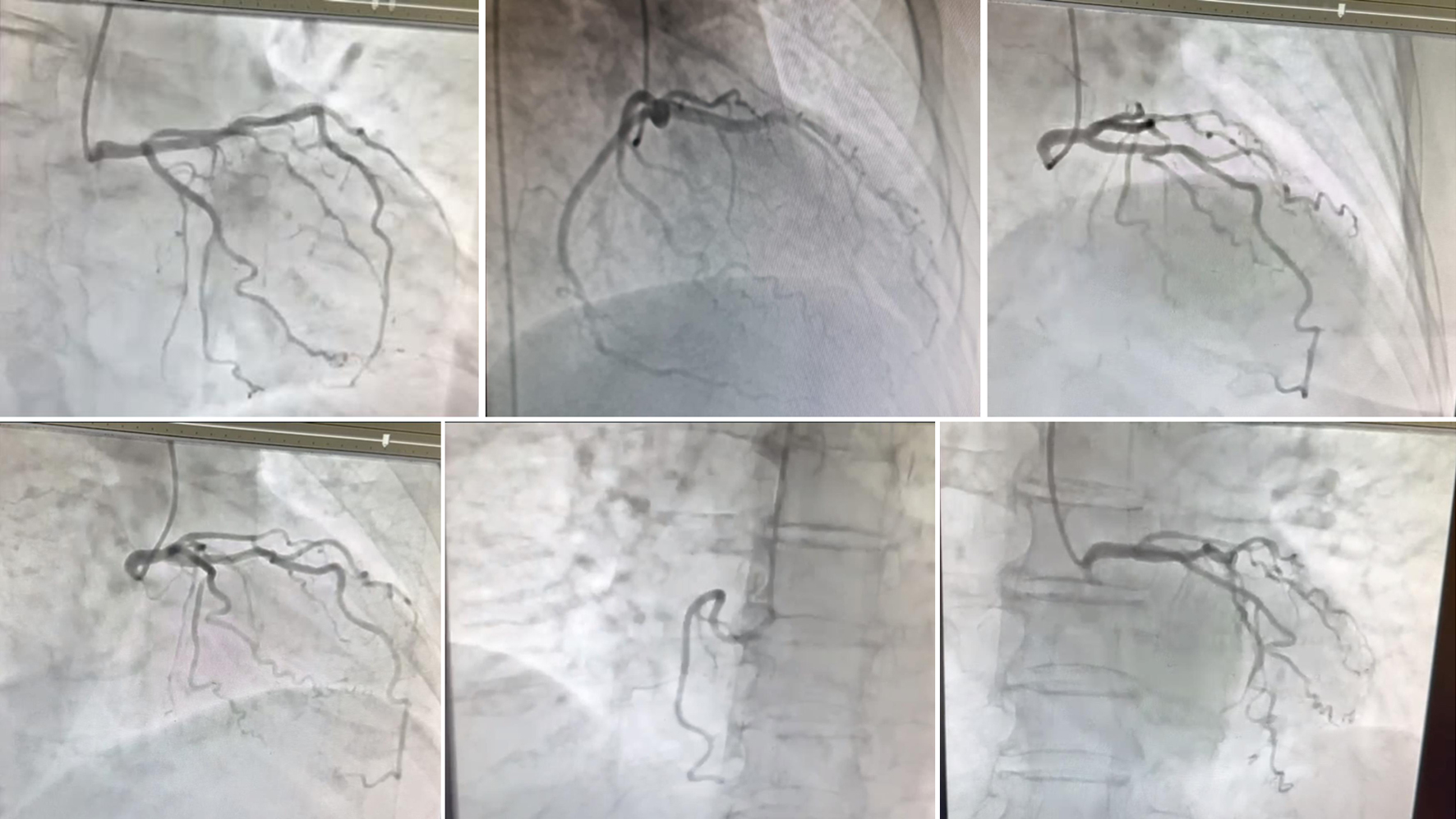 Click for large image | Figure 8. Coronary angiography resulted without coronary obstruction and abnormalities. |
| Discussion | ▴Top |
Our patient developed intraoperative Takotsubo cardiomyopathy despite having no previous cardiac conditions, under adequate general anesthesia, and following the intraoperative combination of oxymetazoline and cabergoline. This is the first reported case in the literature of intraoperative Takotsubo cardiomyopathy, potentially linked to the specific combination of intraoperative cabergoline and oxymetazoline.
Eighty percent of patients with Takotsubo cardiomyopathy develop apical akinesia or dyskinesia, ST-segment elevation, and slightly increased levels of troponin and pro-BNP [11, 12].
Templin and colleagues reported that physical triggers (such as surgery) accounted for 36% of Takotsubo cardiomyopathy cases, emotional triggers for approximately 27%, combined physical and emotional triggers for 7.8%, and 28.5% had an unknown origin [12].
Several mechanisms have been proposed to explain Takotsubo stress cardiomyopathy. The primary mechanisms include catecholamine-induced myocardial toxicity, disruption of the microvasculature, and coronary spasm [13]. The low estrogen theory is also suggested as a possible mechanism due to the high incidence of Takotsubo cardiomyopathy in postmenopausal women [14]. However, our patient had normal endocrinological screening results, except for elevated prolactin levels.
Jabaudon and colleagues reported Takotsubo syndrome after the induction of anesthesia [15]. Adequate premedication and careful anesthesia induction can mitigate the stress and hemodynamic effects of endotracheal intubation. Some studies have reported that isoflurane may provide better myocardial protection than propofol [16]. However, there are currently no data in the literature on which anesthetic offers superior protection against Takotsubo cardiomyopathy syndrome.
Diagnostic criteria for Takotsubo cardiomyopathy include transient akinesia or dyskinesia of the apical portion of the left ventricle (primarily but not exclusively), absence of acute or chronic coronary syndrome, nonspecific ST changes on ECG, exclusion of pheochromocytoma [17], and mildly elevated levels of troponin and BNP. Our patient met all these criteria, presenting with transiently reduced EF, new nonsignificant ST changes, and mildly elevated troponin and pro-BNP levels. Significant ST-segment elevation is not always observed in Takotsubo syndrome. The transient nature of Takotsubo syndrome was confirmed in our patient through clinical improvement and repeat echocardiographic examinations. During the ICU stay, echocardiography showed a significant improvement in cardiac function, increasing from 35% upon ICU admission to 60% before transfer to the ward. No other inotropic support was required, except for norepinephrine, to avoid unnecessary arrhythmias.
Our patient was on chronic cabergoline therapy, a medication commonly used to treat hyperprolactinemia. Cabergoline is a long-acting dopamine D2 receptor agonist. As a dopaminergic drug, cabergoline is contraindicated in uncontrolled hypertension due to its effects on alpha and/or beta receptors. Several studies have reported the use of cabergoline in hypertensive pregnant women to suppress lactation after cesarean section [18].
Humphrey et al reported on the hemodynamic effects of cabergoline during the postpartum period in normotensive women. They enrolled 224 postpartum women and found no hypertensive response in normotensive patients [19]. However, the official information for Dostinex (cabergoline) lists hypertension as a potential side effect. Additionally, cabergoline can reduce the efficacy of several antihypertensive drugs (e.g., angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers, minoxidil, and angiotensin receptor blockers (ARBs)) and potentiate the hypertensive effects of isoprenaline, orciprenaline, and oxymetazoline [20-22].
Approximately 10 min after the neurosurgeon administered oxymetazoline (a standard, uneventful procedure using the same concentration as in previous cases) as nasal puffs, severe hypertension and pulmonary edema were observed. Oxymetazoline is an alpha-1A adrenoreceptor agonist primarily used to treat nasal congestion and allergic reactions, including eye irritation and facial erythema. In transsphenoidal hypophyseal tumor removal, oxymetazoline is utilized to achieve intense local mucosal vasoconstriction, thereby facilitating a cleaner surgical site. The concomitant use of cabergoline can exacerbate the hypertensive effects of oxymetazoline, which led to the severe hypertension observed in our patient [20-22].
Conclusion
Our case appears to be the first reported in the literature. The patient was well managed and discharged without any sequelae. The combination of oxymetazoline and cabergoline could have been avoided with an adequate preoperative evaluation. Stopping cabergoline preoperatively may also be considered. Collaboration among the neurosurgeon, anesthesiologist, and hospitalist can enhance preoperative assessment, reduce complications, and ensure patient safety.
Learning points
Careful preoperative evaluation, with attention to chronic medication adjustments and thorough knowledge of drug interactions, is essential to ensure patient safety. Cabergoline must be avoided or discontinued before surgery if hypertensive drugs are planned for use.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent has been obtained from the patient.
Author Contributions
GH, FC, and RD: paper writing; AXH, AA, and MB: language editing; KL, DL, and AD: literature searching.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Desmet WJ, Adriaenssens BF, Dens JA. Apical ballooning of the left ventricle: first series in white patients. Heart. 2003;89(9):1027-1031.
doi pubmed pmc - Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Nakama Y, Kagawa E, et al. Presentation of Tako-tsubo cardiomyopathy in men and women. Clin Cardiol. 2010;33(1):42-45.
doi pubmed pmc - Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352(6):539-548.
doi pubmed - Deshmukh A, Kumar G, Pant S, Rihal C, Murugiah K, Mehta JL. Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J. 2012;164(1):66-71.e61.
doi pubmed - Komamura K, Fukui M, Iwasaku T, Hirotani S, Masuyama T. Takotsubo cardiomyopathy: Pathophysiology, diagnosis and treatment. World J Cardiol. 2014;6(7):602-609.
doi pubmed pmc - Wedekind H, Moller K, Scholz KH. [Tako-tsubo cardiomyopathy. Incidence in patients with acute coronary syndrome]. Herz. 2006;31(4):339-346.
doi pubmed - Matta AG, Carrie D. Epidemiology, pathophysiology, diagnosis, and principles of management of takotsubo cardiomyopathy: a review. Med Sci Monit. 2023;29:e939020.
doi pubmed pmc - Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, Sheppard MN, et al. Current state of knowledge on Takotsubo syndrome: a Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2016;18(1):8-27.
doi pubmed - Stiermaier T, Reil JC, Sequeira V, Rawish E, Mezger M, Patz T, Paitazoglou C, et al. Hemodynamic assessment in Takotsubo syndrome. J Am Coll Cardiol. 2023;81(20):1979-1991.
doi pubmed - Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, et al. International expert consensus document on Takotsubo syndrome (Part II): diagnostic workup, outcome, and management. Eur Heart J. 2018;39(22):2047-2062.
doi pubmed pmc - Boyd B, Solh T. Takotsubo cardiomyopathy: Review of broken heart syndrome. JAAPA. 2020;33(3):24-29.
doi pubmed - Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, et al. Clinical features and outcomes of Takotsubo (Stress) cardiomyopathy. N Engl J Med. 2015;373(10):929-938.
doi pubmed - Pelliccia F, Kaski JC, Crea F, Camici PG. Pathophysiology of Takotsubo syndrome. Circulation. 2017;135(24):2426-2441.
doi pubmed - Hovgaard HL, Zaremba T, Aaroe J. Relapsing classical Takotsubo syndrome in a postmenopausal woman successfully managed with psychology consultations. Cureus. 2019;11(8):e5361.
doi pubmed pmc - Jabaudon M, Bonnin M, Bolandard F, Chanseaume S, Dauphin C, Bazin JE. Takotsubo syndrome during induction of general anaesthesia. Anaesthesia. 2007;62(5):519-523.
doi pubmed - Oras J, Redfors B, Ali A, Lundgren J, Sihlbom C, Thorsell A, Seeman-Lodding H, et al. Anaesthetic-induced cardioprotection in an experimental model of the Takotsubo syndrome - isoflurane vs. propofol. Acta Anaesthesiol Scand. 2017;61(3):309-321.
doi pubmed - Domi R, Sula H, Kaci M, Paparisto S, Bodeci A, Xhemali A. Anesthetic considerations on adrenal gland surgery. J Clin Med Res. 2015;7(1):1-7.
doi pubmed pmc - AlSaad D, ElSalem S, Abdulrouf PV, Thomas B, Alsaad T, Ahmed A, AlHail M. A retrospective drug use evaluation of cabergoline for lactation inhibition at a tertiary care teaching hospital in Qatar. Ther Clin Risk Manag. 2016;12:155-160.
doi pubmed pmc - Humphrey S, Baechler M, Schiff M, Hitti J. Cabergoline for postpartum lactation suppression: Effect on blood pressure and pulse. Int J Gynaecol Obstet. 2022;159(3):776-782.
doi pubmed - Wang R, Souza NF, Fortes JA, Santos GJ, Faria Neto JR, Zytinski L. Apical ballooning syndrome secondary to nasal decongestant abuse. Arq Bras Cardiol. 2009;93(5):e75-78.
doi pubmed - S YH, Jernberg T. Bromocriptine-induced coronary spasm caused acute coronary syndrome, which triggered its own clinical twin—Takotsubo syndrome. Cardiology. 2011;119(1):1-6.
doi pubmed - https://reference.medscape.com/drug/dostinex-cabergoline-342876.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


